Share of people who have received at least one dose of a COVID-19 vaccine relative to a country's total population. Date is on the map. Commons source.
COVID-19 vaccine doses administered per 100 people by country. Date is on the map. Commons source.
| COVID-19 vaccine | |
|---|---|
| Drug class | |
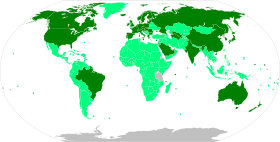 Map of countries by approval status
Approved for general use, mass vaccination underway
EUA (or equivalent) granted, mass vaccination underway
EUA granted, limited vaccination
Approved for general use, mass vaccination planned
EUA granted, mass vaccination planned
EUA pending
No data available | |
| Clinical data | |
| Uses | Prevent COVID-19 |
| Common types | mRNA, viral vector |
| Subtypes | mRNA: Pfizer, Moderna Viral vector: AstraZeneca, Janssen |
| |
COVID‑19 vaccine is a vaccine that provides immunity against severe acute respiratory syndrome coronavirus 2 (SARS‑CoV‑2), the virus that causes COVID‑19. They reduce the severity and risk of deaths.[1][2] Many countries have implemented phased distribution plans that prioritized those at highest risk of complications, such as older people, and those at high risk of exposure and transmission, such as healthcare workers.[3]
Prior to the COVID‑19 pandemic, knowledge existed about the structure and function of coronavirus diseases like severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). This knowledge accelerated the development of various vaccine platforms during early 2020.[4] The initial focus of SARS-CoV-2 vaccines was on preventing symptomatic, often severe illness.[5] On 10 January 2020, the SARS-CoV-2 genetic sequence data was shared through GISAID, and by 19 March, the global pharmaceutical industry announced a major commitment to address COVID‑19.[6] At least 20 different vaccines have been approved in at least one country as of 2022.[7]
As of 30 January 2022[update], more than 10 billion doses of COVID‑19 vaccine has been given worldwide.[8] About 61% of people have received at least one dose; however, in low income countries this is only 10%.[8] In the United States they are purchased by the government and provided for free.[9]
Background[edit | edit source]
| Part of a series on the |
| COVID-19 pandemic |
|---|
|
Prior to COVID‑19, a vaccine for an infectious disease had never been produced in less than several years – and no vaccine existed for preventing a coronavirus infection in humans.[10] However, vaccines have been produced against several animal diseases caused by coronaviruses, including (as of 2003) infectious bronchitis virus in birds, canine coronavirus, and feline coronavirus.[11] Previous projects to develop vaccines for viruses in the family Coronaviridae that affect humans have been aimed at severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS). Vaccines against SARS[12] and MERS[13] have been tested in non-human animals.
According to studies published in 2005 and 2006, the identification and development of novel vaccines and medicines to treat SARS was a priority for governments and public health agencies around the world at that time.[14][15][16] There is no cure or protective vaccine proven to be safe and effective against SARS in humans.[17][18] There is also no proven vaccine against MERS.[19] When MERS became prevalent, it was believed that existing SARS research might provide a useful template for developing vaccines and therapeutics against a MERS-CoV infection.[17][20] As of March 2020, there was one (DNA-based) MERS vaccine which completed Phase I clinical trials in humans,[21] and three others in progress, all being viral-vectored vaccines: two adenoviral-vectored (ChAdOx1-MERS, BVRS-GamVac) and one MVA-vectored (MVA-MERS-S).[22]
Vaccines that use an inactive or weakened virus that has been grown in eggs typically take more than a decade to develop.[23][24] In contrast, mRNA is a molecule that can be made quickly, and research on mRNA to fight diseases was begun decades before the COVID‑19 pandemic by scientists such as Drew Weissman and Katalin Karikó, who tested on mice. Moderna began human testing of an mRNA vaccine in 2015.[23] Viral vector vaccines were also developed for the COVID‑19 pandemic after the technology was previously cleared for Ebola.[23]
As multiple COVID‑19 vaccines have been authorized or licensed for use, real-world vaccine effectiveness (RWE) is being assessed using case control and observational studies.[25] A study is investigating the long-lasting protection against SARS-CoV-2 provided by the mRNA vaccines.[26][27]
Map showing share of population fully vaccinated against COVID-19 relative to a country's total population[note 1]
Medical uses[edit | edit source]
Effectiveness[edit | edit source]
As of August 2021, studies reported that the COVID-19 vaccines available in the United States are "highly protective against severe illness, hospitalization, and death due to COVID-19".[28] In comparison with fully vaccinated people, the CDC reported that unvaccinated people were 5 times more likely to be infected, 10 times more likely to be hospitalized, and 11 times more likely to die.[29][30]
Another study found that unvaccinated people were six times more likely to test positive, 37 times more likely to be hospitalized, and 67 times more likely to die, compared to those who had been vaccinated.[31]
CDC reported that vaccine effectiveness fell from 91% against Alpha to 66% against Delta.[32] One expert stated that "those who are infected following vaccination are still not getting sick and not dying like was happening before vaccination."[33] By late August 2021 the Delta variant accounted for 99 percent of U.S. cases and was found to double the risk of severe illness and hospitalization for those not yet vaccinated.[34]
On 10 December 2021, the UK Health Security Agency reported that early data indicated a 20- to 40-fold reduction in neutralizing activity for Omicron by sera from Pfizer 2-dose vaccinees relative to earlier strains. After a booster dose (usually with an mRNA vaccine),[35] vaccine effectiveness against symptomatic disease was at 70%–75%, and the effectiveness against severe disease was expected to be higher.[36]
Mix and match[edit | edit source]
According to studies, the combination of two different COVID-19 vaccines, also called cross vaccination or mix-and-match method, provides protection equivalent to that of mRNA vaccines – including protection against the Delta variant. Individuals who receive the combination of two different vaccines produce strong immune responses, with side effects no worse than those caused by standard regimens.[37]
Duration of immunity[edit | edit source]
Available data show that fully vaccinated individuals and those previously infected with SARS-CoV-2 have a low risk of subsequent infection for at least 6 months.[38][39][40] Data are currently insufficient to determine an antibody titer threshold that indicates when an individual is protected from infection. Multiple studies show that antibody titers are associated with protection at the population level, but individual protection titers remain unknown. For some populations, such as the elderly and the immunocompromised, protection levels may be reduced after both vaccination and infection. Finally, current data suggest that the level of protection may not be the same for all variants of the virus.[38]
As new data continue to emerge,[41] recommendations will need to be updated periodically. It is important to note that at this time, there is no authorized or approved test that providers or the public can use to reliably determine if a person is protected from infection.[38]
Side effects[edit | edit source]
Side effects associated vaccines targeting COVID‑19 are of high interest to the public.[42] All vaccines that are given via intramuscular injection, including COVID‑19 vaccines, have side effects related to the mild trauma associated with the procedure and introduction of a foreign substance into the body.[43] These include soreness, redness, rash, and inflammation at the injection site. Other common side effects include fatigue, headache, myalgia (muscle pain), and arthralgia (joint pain) which generally resolve within a few days.[44][45]
One less-frequent side effect (that generally occurs in less than 1 in 1,000 people) is hypersensitivity (allergy) to one or more of the vaccine's ingredients, which in some rare cases may cause anaphylaxis.[46][47][48][49] Anaphylaxis has occurred in approximately 2 to 5 people per million vaccinated in the United States.[50] An increased risk of rare and potentially fatal thrombosis events have been associated following the administration of the Janssen (Johnson and Johnson)[51][52] and Oxford-AstraZeneca COVID‑19 vaccines,[52][53][54][55] with the highest reported rate among females in their 30s and 40s. The rate of thrombosis events following vaccination with the Johnson and Johnson and AstraZeneca vaccines has been estimated at 1 case per 100,000 vaccinations compared to between 0.22 and 1.57 cases per 100,000 per year in the general population.[52] There is no increased risk for thrombotic events after vaccination with mRNA COVID‑19 vaccines like Pfizer and Moderna.[50]
Types[edit | edit source]
.jpg)
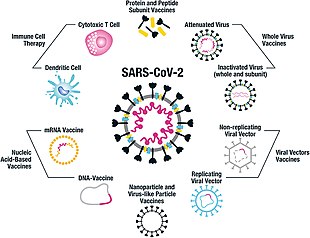
At least nine different technology platforms are under research and development to create an effective vaccine against COVID‑19.[57][58] Most of the platforms of vaccine candidates in clinical trials are focused on the coronavirus spike protein (S protein) and its variants as the primary antigen of COVID‑19 infection,[57] since the S protein triggers strong B-cell and T-cell immune responses.[59][60] However, other coronavirus proteins are also being investigated for vaccine development, like the nucleocapsid, because they also induce a robust T-cell response and their genes are more conserved and recombine less frequently (compared to Spike).[60][61][62]
Platforms developed in 2020 involved nucleic acid technologies (nucleoside-modified messenger RNA and DNA), non-replicating viral vectors, peptides, recombinant proteins, live attenuated viruses, and inactivated viruses.[10][57][63][64]
Many vaccine technologies being developed for COVID‑19 are not like vaccines already in use to prevent influenza, but rather are using "next-generation" strategies for precise targeting of COVID‑19 infection mechanisms.[57][63][64] Several of the synthetic vaccines use a 2P mutation to lock the spike protein into its prefusion configuration, stimulating an adaptive immune response to the virus before it attaches to a human cell.[65] Vaccine platforms in development may improve flexibility for antigen manipulation, and effectiveness for targeting mechanisms of COVID‑19 infection in susceptible population subgroups, such as healthcare workers, the elderly, children, pregnant women, and people with weakened immune systems.[57][63]
mRNA[edit | edit source]
.jpg)
Several COVID‑19 vaccines, including the Pfizer–BioNTech and Moderna vaccines, have been developed to use RNA to stimulate an immune response. When introduced into human tissue, the vaccine contains either self-replicating RNA or messenger RNA (mRNA), which both cause cells to express the SARS-CoV-2 spike protein. This teaches the body how to identify and destroy the corresponding pathogen. RNA vaccines often, but not always, use nucleoside-modified messenger RNA. The delivery of mRNA is achieved by a coformulation of the molecule into lipid nanoparticles which protect the RNA strands and help their absorption into the cells.[66][67][68][69]
RNA vaccines were the first COVID‑19 vaccines to be authorized in the United Kingdom, the United States and the European Union.[70][71] Authorized vaccines of this type are the Pfizer–BioNTech
Severe allergic reactions are rare. In December 2020, 1,893,360 first doses of Pfizer–BioNTech COVID‑19 vaccine administration resulted in 175 cases of severe allergic reaction, of which 21 were anaphylaxis.[78] For 4,041,396 Moderna COVID‑19 vaccine dose administrations in December 2020 and January 2021, only ten cases of anaphylaxis were reported.[78] Lipid nanoparticles (LNPs) were most likely responsible for the allergic reactions.[78]
Adenovirus vector[edit | edit source]
These vaccines are examples of non-replicating viral vector vaccines, using an adenovirus shell containing DNA that encodes a SARS‑CoV‑2 protein.[79][80] The viral vector-based vaccines against COVID‑19 are non-replicating, meaning that they do not make new virus particles, but rather produce only the antigen which elicits a systemic immune response.[79]
Authorized vaccines of this type are the Oxford–AstraZeneca COVID‑19 vaccine,
Convidecia and the Janssen COVID‑19 vaccine are both one-shot vaccines which offer less complicated logistics and can be stored under ordinary refrigeration for several months.[87][88]
Sputnik V uses Ad26 for its first dose, which is the same as Janssen's only dose, and Ad5 for the second dose, which is the same as Convidecia's only dose.[89]
On 11 August 2021, the developers of Sputnik V proposed, in view of the Delta case surge, that Pfizer test the Ad26 component (termed its 'Light' version)[90] as a booster shot:
Delta cases surge in US & Israel shows mRNA vaccines need a heterogeneous booster to strengthen & prolong immune response. #SputnikV pioneered mix&match approach, combo trials & showed 83.1% efficacy vs Delta. Today RDIF offers Pfizer to start trial with Sputnik Light as booster.[91]
Inactivated virus[edit | edit source]
Inactivated vaccines consist of virus particles that are grown in culture and then killed using a method such as heat or formaldehyde to lose disease producing capacity, while still stimulating an immune response.[92]
Authorized vaccines of this type are the Chinese CoronaVac[93][94][95] and the Sinopharm BIBP
Subunit[edit | edit source]
Subunit vaccines present one or more antigens without introducing whole pathogen particles. The antigens involved are often protein subunits, but can be any molecule that is a fragment of the pathogen.[102]
The authorized vaccines of this type are the peptide vaccine EpiVacCorona,
The V451 vaccine was previously in clinical trials, which were terminated because it was found that the vaccine may potentially cause incorrect results for subsequent HIV testing.
Other types[edit | edit source]
Additional types of vaccines that are in clinical trials include virus-like particle vaccines, multiple DNA plasmid vaccines,[110]
Scientists investigated whether existing vaccines for unrelated conditions could prime the immune system and lessen the severity of COVID‑19 infection.[119] There is experimental evidence that the BCG vaccine for tuberculosis has non-specific effects on the immune system, but no evidence that this vaccine is effective against COVID‑19.[120]
Formulation[edit | edit source]
As of September 2020[update], eleven of the vaccine candidates in clinical development use adjuvants to enhance immunogenicity.[57] An immunological adjuvant is a substance formulated with a vaccine to elevate the immune response to an antigen, such as the COVID‑19 virus or influenza virus.[121] Specifically, an adjuvant may be used in formulating a COVID‑19 vaccine candidate to boost its immunogenicity and efficacy to reduce or prevent COVID‑19 infection in vaccinated individuals.[121][122] Adjuvants used in COVID‑19 vaccine formulation may be particularly effective for technologies using the inactivated COVID‑19 virus and recombinant protein-based or vector-based vaccines.[122] Aluminum salts, known as "alum", were the first adjuvant used for licensed vaccines, and are the adjuvant of choice in some 80% of adjuvanted vaccines.[122] The alum adjuvant initiates diverse molecular and cellular mechanisms to enhance immunogenicity, including release of proinflammatory cytokines.[121][122]
In November 2021, the full nucleotide sequences of the AstraZeneca and Pfizer/BioNTech vaccines were released by the UK Medicines and Healthcare Products Regulatory Agency, in response to a freedom of information request.[123]
History[edit | edit source]
Since January 2020, vaccine development has been expedited via unprecedented collaboration in the multinational pharmaceutical industry and between governments.[57]
Multiple steps along the entire development path are evaluated, including:[10][124]
- the level of acceptable toxicity of the vaccine (its safety),
- targeting vulnerable populations,
- the need for vaccine efficacy breakthroughs,
- the duration of vaccination protection,
- special delivery systems (such as oral or nasal, rather than by injection),
- dose regimen,
- stability and storage characteristics,
- emergency use authorization before formal licensing,
- optimal manufacturing for scaling to billions of doses, and
- dissemination of the licensed vaccine.
Challenges[edit | edit source]
There have been several unique challenges with COVID‑19 vaccine development.
The urgency to create a vaccine for COVID‑19 led to compressed schedules that shortened the standard vaccine development timeline, in some cases combining clinical trial steps over months, a process typically conducted sequentially over several years.[125] Public health programs have been described as in "[a] race to vaccinate individuals" with the early wave vaccines.[126]
Timelines for conducting clinical research – normally a sequential process requiring years – are being compressed into safety, efficacy, and dosing trials running simultaneously over months, potentially compromising safety assurance.[125][127] As an example, Chinese vaccine developers and the government Chinese Center for Disease Control and Prevention began their efforts in January 2020,[128] and by March were pursuing numerous candidates on short timelines, with the goal to showcase Chinese technology strengths over those of the United States, and to reassure the Chinese people about the quality of vaccines produced in China.[125][129]
The rapid development and urgency of producing a vaccine for the COVID‑19 pandemic was expected to increase the risks and failure rate of delivering a safe, effective vaccine.[63][64][130] Additionally, research at universities is obstructed by physical distancing and closing of laboratories.[131][132]
Vaccines must progress through several phases of clinical trials to test for safety, immunogenicity, effectiveness, dose levels and adverse effects of the candidate vaccine.[133][134] Vaccine developers have to invest resources internationally to find enough participants for Phase II–III clinical trials when the virus has proved to be a "moving target" of changing transmission rates across and within countries, forcing companies to compete for trial participants.[135] Clinical trial organizers also may encounter people unwilling to be vaccinated due to vaccine hesitancy[136] or disbelief in the science of the vaccine technology and its ability to prevent infection.[137] As new vaccines are developed during the COVID‑19 pandemic, licensure of COVID‑19 vaccine candidates requires submission of a full dossier of information on development and manufacturing quality.[138][139][140]
Organizations[edit | edit source]
Internationally, the Access to COVID‑19 Tools Accelerator is a G20 and World Health Organization (WHO) initiative announced in April 2020.[141][142] It is a cross-discipline support structure to enable partners to share resources and knowledge. It comprises four pillars, each managed by two to three collaborating partners: Vaccines (also called "COVAX"), Diagnostics, Therapeutics, and Health Systems Connector.[143] The WHO's April 2020 "R&D Blueprint (for the) novel Coronavirus" documented a "large, international, multi-site, individually randomized controlled clinical trial" to allow "the concurrent evaluation of the benefits and risks of each promising candidate vaccine within 3–6 months of it being made available for the trial." The WHO vaccine coalition will prioritize which vaccines should go into Phase II and III clinical trials, and determine harmonized Phase III protocols for all vaccines achieving the pivotal trial stage.[144]
National governments have also been involved in vaccine development. Canada announced funding of 96 projects for development and production of vaccines at Canadian companies and universities with plans to establish a "vaccine bank" that could be used if another coronavirus outbreak occurs,[145] and to support clinical trials and develop manufacturing and supply chains for vaccines.[146]
China provided low-rate loans to one vaccine developer through its central bank, and "quickly made land available for the company" to build production plants.[127] Three Chinese vaccine companies and research institutes are supported by the government for financing research, conducting clinical trials, and manufacturing.[147]
The United Kingdom government formed a COVID‑19 vaccine task force in April 2020 to stimulate local efforts for accelerated development of a vaccine through collaborations of industry, universities, and government agencies. The UK's Vaccine Taskforce contributed to every phase of development from research to manufacturing.[148]
In the United States, the Biomedical Advanced Research and Development Authority (BARDA), a federal agency funding disease-fighting technology, announced investments to support American COVID‑19 vaccine development, and manufacture of the most promising candidates.[127][149] In May 2020, the government announced funding for a fast-track program called Operation Warp Speed.[150][151] By March 2021, BARDA had funded an estimated $19.3 billion in COVID‑19 vaccine development.[152]
Large pharmaceutical companies with experience in making vaccines at scale, including Johnson & Johnson, AstraZeneca, and GlaxoSmithKline (GSK), formed alliances with biotechnology companies, governments, and universities to accelerate progression toward effective vaccines.[127][125]
Society and culture[edit | edit source]
Distribution[edit | edit source]
Note about table to the right: Number and percentage of people who have received at least one dose of a COVID‑19 vaccine (unless noted otherwise). May include vaccination of non-citizens, which can push totals beyond 100% of the local population. Table is updated daily by a bot.[note 2]
| Location | Vaccinated[lower-alpha 1] | Percent[lower-alpha 2] | |
|---|---|---|---|
| World[lower-alpha 3][lower-alpha 4] | 5,573,179,306 | 69.88% | |
| China[lower-alpha 5] | 1,310,292,000 | 91.89% | |
| India | 1,027,400,981 | 72.50% | |
| European Union[lower-alpha 6] | 338,183,116 | 75.13% | |
| United States[lower-alpha 7] | 269,835,963 | 81.27% | |
| Indonesia | 203,657,535 | 73.92% | |
| Brazil | 189,643,431 | 88.08% | |
| Pakistan | 162,881,618 | 69.07% | |
| Bangladesh | 151,316,328 | 88.39% | |
| Japan | 104,693,279 | 84.46% | |
| Mexico | 97,179,493 | 76.22% | |
| Vietnam | 90,497,674 | 92.17% | |
| Russia | 88,792,191 | 61.36% | |
| Nigeria | 82,325,196 | 37.67% | |
| Philippines | 78,484,848 | 67.92% | |
| Iran | 65,159,767 | 73.58% | |
| Germany | 64,876,208 | 77.82% | |
| Turkey | 57,941,051 | 67.89% | |
| Thailand | 57,005,497 | 79.62% | |
| Egypt | 56,402,018 | 50.82% | |
| France | 54,667,786 | 80.62% | |
| United Kingdom | 53,806,963 | 79.97% | |
| Italy[lower-alpha 8] | 50,890,551 | 86.20% | |
| South Korea | 44,810,095 | 86.48% | |
| Ethiopia | 43,896,866 | 35.58% | |
| Colombia | 42,971,012 | 82.84% | |
| Argentina | 41,484,679 | 91.15% | |
| Spain | 41,347,499 | 86.94% | |
| Myanmar | 34,777,314 | 64.64% | |
| Canada | 34,763,194 | 90.40% | |
| Tanzania | 34,434,933 | 52.57% | |
| Peru | 30,415,179 | 89.33% | |
| Malaysia | 28,133,279 | 82.90% | |
| Nepal | 27,772,996 | 90.92% | |
| Saudi Arabia | 27,018,975 | 74.21% | |
| Morocco | 25,019,705 | 66.79% | |
| South Africa | 24,165,157 | 40.35% | |
| Poland | 22,873,930 | 57.39% | |
| Australia | 22,236,698 | 84.95% | |
| Venezuela | 22,157,232 | 78.29% | |
| Taiwan | 21,877,888 | 91.56% | |
| Uzbekistan | 21,674,823 | 62.59% | |
| Uganda | 19,488,104 | 41.25% | |
| Mozambique | 18,647,673 | 56.56% | |
| Chile | 18,088,517 | 92.27% | |
| Sri Lanka | 17,143,761 | 78.53% | |
| Ukraine | 15,729,617 | 36.19% | |
| Angola | 15,552,099 | 43.70% | |
| Ecuador | 15,333,873 | 85.18% | |
| Cambodia | 15,280,479 | 91.13% | |
| Sudan | 15,207,452 | 32.44% | |
| Democratic Republic of the Congo | 14,629,322 | 14.78% | |
| Afghanistan | 14,526,772 | 35.32% | |
| Kenya | 14,494,372 | 26.83% | |
| Ivory Coast | 13,568,372 | 48.18% | |
| Ghana | 13,221,421 | 39.50% | |
| Netherlands | 12,775,557 | 73.00% | |
| Iraq | 11,332,925 | 25.47% | |
| Zambia | 11,158,619 | 55.74% | |
| Kazakhstan | 10,858,101 | 55.98% | |
| Cuba | 10,732,602 | 95.72% | |
| Rwanda | 10,572,981 | 76.75% | |
| United Arab Emirates | 9,991,089 | 100.00% | |
| Portugal | 9,782,964 | 95.25% | |
| Belgium | 9,266,177 | 79.50% | |
| Guatemala | 8,924,970 | 50.02% | |
| Romania | 8,187,261 | 41.65% | |
| Greece | 7,934,650 | 76.41% | |
| Algeria | 7,840,131 | 17.75% | |
| Sweden | 7,775,726 | 73.71% | |
| Somalia | 7,729,842 | 43.93% | |
| Guinea | 7,679,918 | 55.41% | |
| Bolivia | 7,361,008 | 60.94% | |
| Dominican Republic | 7,315,127 | 65.15% | |
| Tunisia | 7,218,234 | 58.42% | |
| Czech Republic | 6,976,147 | 66.48% | |
| Hong Kong | 6,914,894 | 92.34% | |
| Austria | 6,899,073 | 77.17% | |
| Israel | 6,722,953 | 71.15% | |
| Honduras | 6,550,968 | 62.79% | |
| Belarus | 6,527,591 | 68.46% | |
| Zimbabwe | 6,437,808 | 40.25% | |
| Hungary | 6,420,813 | 64.42% | |
| Chad | 6,254,729 | 35.29% | |
| Nicaragua | 6,251,151 | 89.97% | |
| Niger | 6,217,508 | 23.72% | |
| Switzerland | 6,096,607 | 69.75% | |
| Laos | 5,888,649 | 79.31% | |
| Azerbaijan | 5,373,253 | 52.10% | |
| Tajikistan | 5,282,863 | 54.18% | |
| Singapore | 5,160,551 | 91.55% | |
| Burkina Faso | 5,152,110 | 22.72% | |
| Sierra Leone | 5,015,637 | 58.28% | |
| Jordan | 4,821,579 | 43.25% | |
| Denmark | 4,781,611 | 81.29% | |
| Malawi | 4,739,457 | 23.23% | |
| El Salvador | 4,652,597 | 73.69% | |
| Costa Rica | 4,628,288 | 89.33% | |
| Finland | 4,524,428 | 81.66% | |
| Norway | 4,346,995 | 79.99% | |
| New Zealand | 4,301,076 | 82.95% | |
| Republic of Ireland | 4,108,076 | 81.78% | |
| Paraguay | 3,988,744 | 58.82% | |
| Mali | 3,959,022 | 17.52% | |
| South Sudan | 3,849,926 | 35.28% | |
| Liberia | 3,825,381 | 72.14% | |
| Benin | 3,697,190 | 27.69% | |
| Cameroon | 3,615,939 | 12.95% | |
| Panama | 3,529,545 | 80.06% | |
| Kuwait | 3,456,620 | 80.97% | |
| Serbia | 3,354,075 | 48.81% | |
| Oman | 3,257,365 | 71.18% | |
| Syria | 3,209,797 | 14.51% | |
| Uruguay | 3,009,454 | 87.92% | |
| Qatar | 2,852,001 | 105.82% | |
| Slovakia | 2,822,919 | 51.82% | |
| Lebanon | 2,740,227 | 49.92% | |
| Senegal | 2,684,696 | 15.50% | |
| Madagascar | 2,502,027 | 8.45% | |
| Central African Republic | 2,381,935 | 42.69% | |
| Croatia | 2,321,402 | 57.60% | |
| Libya | 2,316,327 | 34.00% | |
| Mongolia | 2,272,965 | 68.27% | |
| Togo | 2,246,404 | 25.39% | |
| Bulgaria | 2,107,140 | 31.07% | |
| Mauritania | 2,100,725 | 44.36% | |
| Palestine | 2,012,767 | 38.34% | |
| Lithuania | 1,957,055 | 71.16% | |
| Botswana | 1,948,922 | 74.10% | |
| Kyrgyzstan | 1,662,033 | 25.07% | |
| Georgia | 1,654,504 | 44.03% | |
| Albania | 1,347,054 | 47.39% | |
| Latvia | 1,346,184 | 71.84% | |
| Slovenia | 1,265,802 | 59.72% | |
| Bahrain | 1,241,174 | 84.31% | |
| Armenia | 1,128,072 | 38.01% | |
| Mauritius | 1,123,773 | 86.48% | |
| Moldova | 1,108,063 | 33.85% | |
| Yemen | 1,018,387 | 3.02% | |
| Lesotho | 1,014,073 | 43.98% | |
| Bosnia and Herzegovina | 943,394 | 28.91% | |
| Gambia | 934,799 | 34.55% | |
| Kosovo | 906,858 | 50.89% | |
| Timor-Leste | 883,440 | 65.86% | |
| Estonia | 869,264 | 65.55% | |
| Jamaica | 854,889 | 30.24% | |
| North Macedonia | 854,392 | 40.81% | |
| Trinidad and Tobago | 753,588 | 49.39% | |
| Fiji | 712,010 | 76.58% | |
| Bhutan | 699,116 | 89.35% | |
| Republic of the Congo | 695,760 | 11.92% | |
| Macau | 679,602 | 97.76% | |
| Cyprus | 670,969 | 74.88% | |
| Namibia | 614,204 | 23.93% | |
| Guinea-Bissau | 579,572 | 27.53% | |
| Eswatini | 511,632 | 42.58% | |
| Guyana | 495,285 | 61.24% | |
| Luxembourg | 481,957 | 74.42% | |
| Malta | 478,768 | 89.78% | |
| Haiti | 463,694 | 4.00% | |
| Brunei | 450,944 | 100.43% | |
| Comoros | 438,825 | 53.41% | |
| Maldives | 399,225 | 76.22% | |
| Papua New Guinea | 379,658 | 3.74% | |
| Djibouti | 369,633 | 32.98% | |
| Cabo Verde | 356,734 | 60.68% | |
| Solomon Islands | 343,821 | 47.47% | |
| Gabon | 311,040 | 13.02% | |
| Iceland | 309,770 | 84.00% | |
| Northern Cyprus | 301,673 | 78.80% | |
| Montenegro | 292,783 | 46.63% | |
| Equatorial Guinea | 270,109 | 16.53% | |
| Suriname | 267,820 | 45.26% | |
| Belize | 251,960 | 62.17% | |
| New Caledonia | 192,367 | 66.34% | |
| Samoa | 191,371 | 86.05% | |
| French Polynesia | 190,908 | 62.33% | |
| Vanuatu | 176,624 | 54.06% | |
| Bahamas | 174,147 | 42.48% | |
| Barbados | 163,833 | 58.17% | |
| Sao Tome and Principe | 140,256 | 61.68% | |
| Curaçao | 108,601 | 56.81% | |
| Kiribati | 100,900 | 76.88% | |
| Aruba | 90,379 | 84.90% | |
| Seychelles | 88,498 | 82.60% | |
| Tonga | 87,278 | 81.67% | |
| Jersey | 84,365 | 76.14% | |
| Isle of Man | 69,560 | 81.44% | |
| Antigua and Barbuda | 64,290 | 68.97% | |
| Cayman Islands | 62,023 | 90.25% | |
| Saint Lucia | 60,140 | 33.43% | |
| Andorra | 57,901 | 72.52% | |
| Guernsey | 54,223 | 85.62% | |
| Bermuda | 48,554 | 75.65% | |
| Grenada | 44,241 | 35.26% | |
| Gibraltar | 42,175 | 129.07% | |
| Faroe Islands | 41,715 | 85.04% | |
| Greenland | 41,243 | 72.52% | |
| Saint Vincent and the Grenadines | 37,527 | 36.10% | |
| Burundi | 34,323 | 0.27% | |
| Saint Kitts and Nevis | 33,794 | 70.88% | |
| Dominica | 32,995 | 45.57% | |
| Turks and Caicos Islands | 32,815 | 71.76% | |
| Turkmenistan | 32,240 | 0.53% | |
| Sint Maarten | 29,788 | 67.41% | |
| Liechtenstein | 26,769 | 68.02% | |
| Monaco | 26,672 | 67.49% | |
| San Marino | 26,357 | 77.50% | |
| British Virgin Islands | 19,466 | 62.55% | |
| Caribbean Netherlands | 19,109 | 72.26% | |
| Cook Islands | 15,112 | 88.73% | |
| Nauru | 13,106 | 103.27% | |
| Anguilla | 10,854 | 68.36% | |
| Wallis and Futuna | 7,150 | 61.66% | |
| Tuvalu | 6,368 | 53.40% | |
| Saint Helena, Ascension and Tristan da Cunha | 4,361 | 71.83% | |
| Falkland Islands | 2,632 | 75.57% | |
| Tokelau | 2,203 | 116.38% | |
| Montserrat | 2,104 | 47.68% | |
| Niue | 1,650 | 102.23% | |
| Pitcairn Islands | 47 | 100.00% | |
| North Korea | 0 | 0.00% | |
| |||
As of 25 January 2022[update], 9.87 billion COVID-19 vaccine doses have been administered worldwide, with 60.5 percent of the global population having received at least one dose. While 27.83 million vaccines were then being administered daily, only 9.5 percent of people in low-income countries had received at least a first vaccine by January 2022, according to official reports from national health agencies, which are collated by Our World in Data.[154]
During a pandemic on the rapid timeline and scale of COVID-19 cases in 2020, international organizations like the World Health Organization (WHO) and Coalition for Epidemic Preparedness Innovations (CEPI), vaccine developers, governments, and industry evaluated the distribution of the eventual vaccine(s).[144] Individual countries producing a vaccine may be persuaded to favor the highest bidder for manufacturing or provide first-service to their own country.[10][155][156][127] Experts emphasize that licensed vaccines should be available and affordable for people at the frontline of healthcare and having the greatest need.[10][155][127]
In April 2020, it was reported that the UK agreed to work with 20 other countries and global organizations including France, Germany and Italy to find a vaccine and to share the results, and that UK citizens would not get preferential access to any new COVID‑19 vaccines developed by taxpayer-funded UK universities.[157] Several companies planned to initially manufacture a vaccine at artificially low pricing, then increase prices for profitability later if annual vaccinations are needed and as countries build stock for future needs.[127]
An April 2020 CEPI report stated: "Strong international coordination and cooperation between vaccine developers, regulators, policymakers, funders, public health bodies, and governments will be needed to ensure that promising late-stage vaccine candidates can be manufactured in sufficient quantities and equitably supplied to all affected areas, particularly low-resource regions."[63] The WHO and CEPI are developing financial resources and guidelines for global deployment of several safe, effective COVID‑19 vaccines, recognizing the need is different across countries and population segments.[144][158][159][160][excessive citations] For example, successful COVID‑19 vaccines would be allocated early to healthcare personnel and populations at greatest risk of severe illness and death from COVID‑19 infection, such as the elderly or densely-populated impoverished people.[161][162]
The WHO had set out the target to vaccinate 40% of the population of all countries by the end-2021 and 70% by mid-2022,[163] but many countries missed the 40% target at the end of 2021.[164][165]
Access[edit | edit source]

Countries have extremely unequal access to the COVID-19 vaccine. Vaccine equity has not been achieved, or even approximated. The inequity has harmed both countries with poor access and countries with good access.[166]
Nations pledged to buy doses of the COVID‑19 vaccine before the doses were available. Though high-income nations represent only 14% of the global population, as of 15 November 2020, they had contracted to buy 51% of all pre-sold doses. Some high-income nations bought more doses than would be necessary to vaccinate their entire populations.[167]
On 18 January 2021, WHO Director-General Tedros Adhanom Ghebreyesus warned of problems with equitable distribution: "More than 39 million doses of vaccine have now been administered in at least 49 higher-income countries. Just 25 doses have been given in one lowest-income country. Not 25 million; not 25 thousand; just 25."[168]
In March, it was revealed the US attempted to convince Brazil not to purchase the Sputnik V COVID‑19 vaccine, fearing "Russian influence" in Latin America.[169] Some nations involved in long-standing territorial disputes have reportedly had their access to vaccines blocked by competing nations; Palestine has accused Israel of blocking vaccine delivery to Gaza, while Taiwan has suggested that China has hampered its efforts to procure vaccine doses.[170][171][172]
A single dose of the COVID‑19 vaccine by AstraZeneca would cost 47 Egyptian pounds (EGP), and the authorities are selling it between 100 and 200 EGP. A report by Carnegie Endowment for International Peace cited the poverty rate in Egypt as around 29.7 percent, which constitutes approximately 30.5 million people, and claimed that about 15 million of the Egyptians would be unable to gain access to the luxury of vaccination. A human rights lawyer, Khaled Ali, launched a lawsuit against the government, forcing them to provide vaccination free of cost to all members of the public.[173]
According to immunologist Dr. Anthony Fauci, mutant strains of the virus and limited vaccine distribution pose continuing risks and he said: "we have to get the entire world vaccinated, not just our own country."[174] Edward Bergmark and Arick Wierson are calling for a global vaccination effort and wrote that the wealthier nations' "me-first" mentality could ultimately backfire because the spread of the virus in poorer countries would lead to more variants, against which the vaccines could be less effective.[175]
On 10 March 2021, the United States, Britain, European Union member states and some other members of the World Trade Organization (WTO) blocked a push by more than eighty developing countries to waive COVID‑19 vaccine patent rights in an effort to boost production of vaccines for poor nations.[176] On 5 May 2021, the US government under President Joe Biden announced that it supports waiving intellectual property protections for COVID‑19 vaccines.[177] The Members of the European Parliament have backed a motion demanding the temporary lifting of intellectual properties rights for COVID‑19 vaccines.[178]
In a meeting in April 2021, the World Health Organization's emergency committee addressed concerns of persistent inequity in the global vaccine distribution.[179] Although 9 percent of the world's population lives in the 29 poorest countries, these countries had received only 0.3% of all vaccines administered as of May 2021.[180] On 15 March, Brazilian journalism agency Agência Pública reported that the country vaccinated about twice as many people who declare themselves white than black and noted that mortality from COVID‑19 is higher in the black population.[181]
In May 2021, UNICEF made an urgent appeal to industrialised nations to pool their excess COVID‑19 vaccine capacity to make up for a 125-million-dose gap in the COVAX program. The program mostly relied on the Oxford–AstraZeneca COVID‑19 vaccine produced by Serum Institute of India, which faced serious supply problems due to increased domestic vaccine needs in India from March to June 2021. Only a limited amount of vaccines can be distributed efficiently, and the shortfall of vaccines in South America and parts of Asia are due to a lack of expedient donations by richer nations. International aid organisations have pointed at Nepal, Sri Lanka, and Maldives as well as Argentina and Brazil, and some parts of the Caribbean as problem areas, where vaccines are in short supply. In mid-May 2021, UNICEF was also critical of the fact that most proposed donations of Moderna and Pfizer vaccines were not slated for delivery until the second half of 2021, or early in 2022.[182]
On 1 July 2021, the heads of the World Bank Group, the International Monetary Fund, the World Health Organization, and the World Trade Organization said in a joint statement: "As many countries are struggling with new variants and a third wave of COVID‑19 infections, accelerating access to vaccines becomes even more critical to ending the pandemic everywhere and achieving broad-based growth. We are deeply concerned about the limited vaccines, therapeutics, diagnostics, and support for deliveries available to developing countries."[183][184] In July 2021, The BMJ reported that countries have thrown out over 250,000 vaccine doses as supply exceeded demand and strict laws prevented the sharing of vaccines.[185] A survey by The New York Times found that over a million doses of vaccine had been thrown away in ten U.S. states because federal regulations prohibit recalling them, preventing their redistribution abroad.[186] Furthermore, doses donated close to expiration often cannot be administered quickly enough by recipient countries and end up having to be discarded.[187]
Amnesty International and Oxfam International have criticized the support of vaccine monopolies by the governments of producing countries, noting that this is dramatically increasing the dose price by five times and often much more, creating an economic barrier to access for poor countries.[188][189] Médecins Sans Frontières (Doctors without Borders) has also criticized vaccine monopolies and repeatedly called from their suspension, supporting the TRIPS Waiver. The waiver was first proposed in October 2020, and has support from most countries, but delayed by opposition from EU (especially Germany - major EU countries such as France, Italy and Spain support the exemption),[190] UK, Norway, and Switzerland, among others. MSF called for a Day of Action in September 2021 to put pressure on the WTO Minister's meeting in November, which is expected to discuss the TRIPS IP waiver.[191][192][193]

On 4 August 2021, to reduce unequal distribution between rich and poor countries, the WHO called for a moratorium on a booster dose at least until the end of September. However, on 18 August, the United States government announced plans to offer booster doses 8 months after the initial course to the general population, starting with priority groups. Before the announcement, the WHO harshly criticized this type of decision, citing the lack of evidence for the need for boosters, except for patients with specific conditions. At this time, vaccine coverage of at least one dose was 58% in high-income countries and only 1.3% in low-income countries, and 1.14 million Americans already received an unauthorized booster dose. US officials argued that waning efficacy against mild and moderate disease might indicate reduced protection against severe disease in the coming months. Israel, France, Germany, and the United Kingdom have also started planning boosters for specific groups.[194][195][196] On 14 September 2021, more than 140 former world leaders, and Nobel laureates, including former President of France François Hollande, former Prime Minister of the United Kingdom Gordon Brown, former Prime Minister of New Zealand Helen Clark, and Professor Joseph Stiglitz, called on the candidates to be the next German chancellor to declare themselves in favour of waiving intellectual property rules for COVID‑19 vaccines and transferring vaccine technologies.[197] In November 2021, nursing unions in 28 countries have filed a formal appeal with the United Nations over the refusal of the UK, EU, Norway, Switzerland, and Singapore to temporarily waive patents for Covid vaccines.[198]
During his first international trip, President of Peru Pedro Castillo spoke at the seventy-sixth session of the United Nations General Assembly on 21 September 2021, proposing the creation of an international treaty signed by world leaders and pharmaceutical companies to guarantee universal vaccine access, arguing "The battle against the pandemic has shown us the failure of the international community to cooperate under the principle of solidarity".[199][200]
Optimizing the societal benefit of vaccination may benefit from a strategy that is tailored to the state of the pandemic, the demographics of a country, the age of the recipients, the availability of vaccines, and the individual risk for severe disease: In the UK, the interval between prime and boost dose was extended to vaccinate as many persons as early as possible,[201] many countries are starting to give an additional booster shot to the immunosuppressed[202][203] and the elderly,[204] and research predicts an additional benefit of personalizing vaccine dose in the setting of limited vaccine availability when a wave of virus Variants of Concern hits a country.[205]
While vaccines substantially reduce the probability of infection, it is still possible for fully vaccinated people to contract and spread COVID‑19.[206] Public health agencies have recommended that vaccinated people continue using preventive measures (wear face masks, social distance, wash hands) to avoid infecting others, especially vulnerable people, particularly in areas with high community spread. Governments have indicated that such recommendations will be reduced as vaccination rates increase and community spread declines.[207]
Economics[edit | edit source]
Moreover, an unequal distribution of vaccines will deepen inequality and exaggerate the gap between rich and poor and will reverse decades of hard-won progress on human development.
— United Nations, COVID vaccines: Widening inequality and millions vulnerable[208]
Vaccine inequity damages the global economy, disrupting the global supply chain.[166] Most vaccines were being reserved for wealthy countries, as of September 2021[update],[208] some of which have more vaccine than is needed to fully vaccinate their populations.[167] When people, undervaccinated, needlessly die, suffer disability, and live under lockdown restrictions, they cannot supply the same goods and services. This harms the economies of undervaccinated and overvaccinated countries alike. Since rich countries have larger economies, rich countries may lose more money to vaccine inequity than poor ones,[166] though the poor ones will lose a higher percentage of GDP and suffer longer-term effects.[209] High-income countries would profit an estimated US$4.80 for every $1 spent on giving vaccines to lower-income countries.[166]
The International Monetary Fund sees the vaccine divide between rich and poor nations as a serious obstacle to a global economic recovery.[210] Vaccine inequity disproportionately affects refuge-providing states, as they tend to be poorer, and refugees and displaced people are economically more vulnerable even within those low-income states, so they have suffered more economically from vaccine inequity.[211]
Liability[edit | edit source]
Several governments agreed to shield pharmaceutical companies like Pfizer and Moderna from negligence claims related to COVID‑19 vaccines (and treatments), as in previous pandemics, when governments also took on liability for such claims.
In the US, these liability shields took effect on 4 February 2020, when the US Secretary of Health and Human Services Alex Azar published a notice of declaration under the Public Readiness and Emergency Preparedness Act (PREP Act) for medical countermeasures against COVID‑19, covering "any vaccine, used to treat, diagnose, cure, prevent, or mitigate COVID‑19, or the transmission of SARS-CoV-2 or a virus mutating therefrom". The declaration precludes "liability claims alleging negligence by a manufacturer in creating a vaccine, or negligence by a health care provider in prescribing the wrong dose, absent willful misconduct." In other words, absent "willful misconduct", these companies can not be sued for money damages for any injuries that occur between 2020 and 2024 from the administration of vaccines and treatments related to COVID‑19.[212] The declaration is effective in the United States through 1 October 2024.[212]
In December 2020, the UK government granted Pfizer legal indemnity for its COVID‑19 vaccine.[213]
In the European Union, the COVID‑19 vaccines are licensed under a Conditional Marketing Authorisation which does not exempt manufacturers from civil and administrative liability claims.[214] While the purchasing contracts with vaccine manufacturers remain secret, they do not contain liability exemptions even for side-effects not known at the time of licensure.[215]
The Bureau of Investigative Journalism, a nonprofit news organization, reported in an investigation that unnamed officials in some countries, such as Argentina and Brazil, said that Pfizer demanded guarantees against costs of legal cases due to adverse effects in the form of liability waivers and sovereign assets such as federal bank reserves, embassy buildings or military bases, going beyond the expected from other countries such as the US.[216] During the pandemic parliamentary inquiry in Brazil, Pfizer's representative said that its terms for Brazil are the same as for all other countries with which it has signed deals.[217]
Controversy[edit | edit source]
In June 2021, a report revealed that the UB-612 vaccine, developed by the US-based COVAXX, was a venture initiated for profits by the Blackwater founder Erik Prince. In a series of text messages to Paul Behrends, the close associate recruited for the COVAXX project, Prince described the profit-making possibilities in selling the COVID‑19 vaccines. COVAXX provided no data from the clinical trials on safety or efficacy. The responsibility of creating distribution networks was assigned to an Abu Dhabi-based entity, which was mentioned as "Windward Capital" on the COVAXX letterhead but was actually Windward Holdings. The firm's sole shareholder, which handled "professional, scientific and technical activities", was Erik Prince. In March 2021, COVAXX raised $1.35 billion in a private placement.[218]
Misinformation[edit | edit source]

Anti-vaccination activists and other people in many countries have spread a variety of unfounded conspiracy theories and other misinformation about COVID-19 vaccines based on misunderstood or misrepresented science, religion, exaggerated claims about side effects, a story about COVID-19 being spread by 5G, misrepresentations about how the immune system works and when and how COVID-19 vaccines are made, and other false or distorted information. This misinformation has proliferated and made many people averse to vaccination.[219] This has led to governments and private organisations around the world introducing measures to encourage vaccination such as lotteries,[220] mandates[221] and free entry to events,[222] which has in turn led to further misinformation about the legality and effect of these measures themselves.[223] In January 2022, a systematic review and meta-analysis concluded that nocebo responses accounted for 72% after the first COVID-19 vaccine dose and 52% after the second dose.[224][225][226]
Research[edit | edit source]
COVID-19 vaccine clinical research uses clinical research to establish the characteristics of COVID-19 vaccines. These characteristics include efficacy, effectiveness and safety. Thirty vaccines are authorized for use by national governments, including eight approved for emergency or full use by at least one WHO-recognised stringent regulatory authority; while five are in Phase IV. 204 vaccines are undergoing clinical trials that have yet to be authorized. Nine clinical trials consider heterologous vaccination courses.
Thirty vaccines are authorized by at least one national regulatory authority for public use:[227][228]
As of July 2021, 330 vaccine candidates were in various stages of development, with 102 in clinical research, including 30 in Phase I trials, 30 in Phase I–II trials, 25 in Phase III trials, and 8 in Phase IV development.[227]See also[edit | edit source]
- 2009 swine flu pandemic vaccine
- COVID‑19 drug development
- COVID-19 vaccine clinical research: Effectiveness
- COVID‑19 drug repurposing research
- COVID‑19 vaccine card
- Universal coronavirus vaccine
- Vaccine passports during the COVID‑19 pandemic
- List of COVID-19 vaccine authorizations
Notes[edit | edit source]
- ↑ Our World in Data (OWID) vaccination maps. Click on the download tab to download the map. The table tab has a table of the exact data by country. The source tab says the data is from verifiable public official sources Archived 2021-12-21 at the Wayback Machine collated by Our World in Data. The map at the source is interactive and provides more detail. Run your cursor over the color bar legend to see the countries that apply to that point in the legend. There is an OWID vaccination info FAQ Archived 2021-03-10 at the Wayback Machine.
- ↑ The table data is automatically updated daily by a bot; see Template:COVID-19 data for more information. Scroll down past the table to find the documentation and the main reference. See also: Category:Automatically updated COVID-19 pandemic table templates.
References[edit | edit source]
- ↑ Vergano D (5 June 2021). "COVID-19 Vaccines Work Way Better Than We Had Ever Expected. Scientists Are Still Figuring Out Why". BuzzFeed News. Archived from the original on 6 October 2021. Retrieved 24 June 2021.
- ↑ Mallapaty S, Callaway E, Kozlov M, Ledford H, Pickrell J, Van Noorden R (16 December 2021). "How COVID vaccines shaped 2021 in eight powerful charts". Nature. 600 (7890): 580–583. Bibcode:2021Natur.600..580M. doi:10.1038/d41586-021-03686-x. PMID 34916666. S2CID 245262732.
- ↑ Beaumont P (18 November 2020). "Covid-19 vaccine: who are countries prioritising for first doses?". The Guardian. ISSN 0261-3077. Archived from the original on 18 January 2021. Retrieved 26 December 2020.
- ↑ Li YD, Chi WY, Su JH, Ferrall L, Hung CF, Wu TC (December 2020). "Coronavirus vaccine development: from SARS and MERS to COVID-19". Journal of Biomedical Science. 27 (1): 104. doi:10.1186/s12929-020-00695-2. PMC 7749790. PMID 33341119.
- ↑ Subbarao K (July 2021). "The success of SARS-CoV-2 vaccines and challenges ahead". Cell Host & Microbe. 29 (7): 1111–1123. doi:10.1016/j.chom.2021.06.016. PMC 8279572. PMID 34265245.
- ↑ Padilla TB (24 February 2021). "No one is safe unless everyone is safe". BusinessWorld. Archived from the original on 23 February 2021. Retrieved 24 February 2021.
- ↑ Holder, Josh (29 January 2021). "Tracking Coronavirus Vaccinations Around the World". The New York Times. Archived from the original on 22 December 2021. Retrieved 30 January 2022.
- ↑ 8.0 8.1 Richie H, Ortiz-Ospina E, Beltekian D, Methieu E, Hasell J, Macdonald B, et al. (5 March 2020). "Coronavirus (COVID-19) Vaccinations – Statistics and Research". Our World in Data. Archived from the original on 10 March 2021. Retrieved 7 February 2021.
- ↑ "COVID-19 Vaccination". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 28 January 2022. Retrieved 29 January 2022.
- ↑ 10.0 10.1 10.2 10.3 10.4 Gates B (30 April 2020). "The vaccine race explained: What you need to know about the COVID-19 vaccine". The Gates Notes. Archived from the original on 14 May 2020. Retrieved 2 May 2020.
- ↑ Cavanagh D (December 2003). "Severe acute respiratory syndrome vaccine development: experiences of vaccination against avian infectious bronchitis coronavirus". Avian Pathology. 32 (6): 567–582. doi:10.1080/03079450310001621198. PMC 7154303. PMID 14676007.
- ↑ Gao W, Tamin A, Soloff A, D'Aiuto L, Nwanegbo E, Robbins PD, et al. (December 2003). "Effects of a SARS-associated coronavirus vaccine in monkeys". Lancet. 362 (9399): 1895–1896. doi:10.1016/S0140-6736(03)14962-8. PMC 7112457. PMID 14667748.
- ↑ Kim E, Okada K, Kenniston T, Raj VS, AlHajri MM, Farag EA, et al. (October 2014). "Immunogenicity of an adenoviral-based Middle East Respiratory Syndrome coronavirus vaccine in BALB/c mice". Vaccine. 32 (45): 5975–5982. doi:10.1016/j.vaccine.2014.08.058. PMC 7115510. PMID 25192975.
- ↑ Greenough TC, Babcock GJ, Roberts A, Hernandez HJ, Thomas WD, Coccia JA, et al. (February 2005). "Development and characterization of a severe acute respiratory syndrome-associated coronavirus-neutralizing human monoclonal antibody that provides effective immunoprophylaxis in mice". The Journal of Infectious Diseases. 191 (4): 507–514. doi:10.1086/427242. PMC 7110081. PMID 15655773.
- ↑ Tripp RA, Haynes LM, Moore D, Anderson B, Tamin A, Harcourt BH, et al. (September 2005). "Monoclonal antibodies to SARS-associated coronavirus (SARS-CoV): identification of neutralizing and antibodies reactive to S, N, M and E viral proteins". Journal of Virological Methods. 128 (1–2): 21–28. doi:10.1016/j.jviromet.2005.03.021. PMC 7112802. PMID 15885812.
- ↑ Roberts A, Thomas WD, Guarner J, Lamirande EW, Babcock GJ, Greenough TC, et al. (March 2006). "Therapy with a severe acute respiratory syndrome-associated coronavirus-neutralizing human monoclonal antibody reduces disease severity and viral burden in golden Syrian hamsters". The Journal of Infectious Diseases. 193 (5): 685–692. doi:10.1086/500143. PMC 7109703. PMID 16453264.
- ↑ 17.0 17.1 Jiang S, Lu L, Du L (January 2013). "Development of SARS vaccines and therapeutics is still needed". Future Virology. 8 (1): 1–2. doi:10.2217/fvl.12.126. PMC 7079997. PMID 32201503.
- ↑ "SARS (severe acute respiratory syndrome)". National Health Service. 5 March 2020. Archived from the original on 9 March 2020. Retrieved 31 January 2020.
- ↑ Shehata MM, Gomaa MR, Ali MA, Kayali G (June 2016). "Middle East respiratory syndrome coronavirus: a comprehensive review". Frontiers of Medicine. 10 (2): 120–136. doi:10.1007/s11684-016-0430-6. PMC 7089261. PMID 26791756.
- ↑ Butler D (October 2012). "SARS veterans tackle coronavirus". Nature. 490 (7418): 20. Bibcode:2012Natur.490...20B. doi:10.1038/490020a. PMID 23038444.
- ↑ Modjarrad K, Roberts CC, Mills KT, Castellano AR, Paolino K, Muthumani K, et al. (September 2019). "Safety and immunogenicity of an anti-Middle East respiratory syndrome coronavirus DNA vaccine: a phase 1, open-label, single-arm, dose-escalation trial". The Lancet. Infectious Diseases. 19 (9): 1013–1022. doi:10.1016/S1473-3099(19)30266-X. PMC 7185789. PMID 31351922.
- ↑ Yong CY, Ong HK, Yeap SK, Ho KL, Tan WS (2019). "Recent Advances in the Vaccine Development Against Middle East Respiratory Syndrome-Coronavirus". Frontiers in Microbiology. 10: 1781. doi:10.3389/fmicb.2019.01781. PMC 6688523. PMID 31428074.
- ↑ 23.0 23.1 23.2 Loftus P, Hopkins JS, Pancevski B (17 November 2020). "Moderna and Pfizer Are Reinventing Vaccines, Starting With Covid". The Wall Street Journal. Archived from the original on 6 November 2021. Retrieved 4 October 2021.
- ↑ Sharma O, Sultan AA, Ding H, Triggle CR (14 October 2020). "A Review of the Progress and Challenges of Developing a Vaccine for COVID-19". Frontiers in Immunology. 11: 585354. doi:10.3389/fimmu.2020.585354. PMC 7591699. PMID 33163000.
- ↑ Bok K, Sitar S, Graham BS, Mascola JR (August 2021). "Accelerated COVID-19 vaccine development: milestones, lessons, and prospects". Immunity. 54 (8): 1636–1651. doi:10.1016/j.immuni.2021.07.017. PMC 8328682. PMID 34348117.
- ↑ Turner JS, O'Halloran JA, Kalaidina E, Kim W, Schmitz AJ, Zhou JQ, et al. (August 2021). "SARS-CoV-2 mRNA vaccines induce persistent human germinal centre responses". Nature. 596 (7870): 109–113. Bibcode:2021Natur.596..109T. doi:10.1038/s41586-021-03738-2. PMID 34182569.
- ↑ "Pfizer and Moderna Vaccines Likely to Produce Lasting Immunity, Study Finds". The New York Times. 28 June 2021. Archived from the original on 12 November 2021. Retrieved 23 January 2022.
- ↑ "Vaccine Effectiveness". Virginia Dept. of Health. 23 August 2021.
- ↑ Holcombe, Madeline; Waldrop, Theresa (11 September 2021). "CDC study: Unvaccinated 11 times more likely to die from Covid-19". CNN. Retrieved 2021-09-11.
{{cite web}}: CS1 maint: url-status (link) - ↑ Scobie, Heather; Johnson, Amelia; Suthar, Amitabh (10 September 2021). [https://web.archive.org/web/20220128163934/https://www.cdc.gov/mmwr/volumes/70/wr/mm7037e1.htm?s_cid=mm7037e1_w Archived] 2022-01-28 at the [[Wayback Machine]][[Category:Webarchive template wayback links]] "Monitoring Incidence of COVID-19 Cases, Hospitalizations, and Deaths, by Vaccination Status". Physiotherapy. 64 (2): 39–40. doi:10.15585/mmwr.mm7037e1. PMID 345296. S2CID 237547342. Retrieved 2021-09-10.
{{cite journal}}: Check|url=value (help)CS1 maint: url-status (link) - ↑ ""Unvaccinated 67 times more likely to die from COVID-19, adjusted data shows"". King5 News. 27 August 2021.
- ↑ Fowlkes, Ashley (2021). "Effectiveness of COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Frontline Workers Before and During B.1.617.2 (Delta) Variant Predominance – Eight U.S. Locations, December 2020–August 2021". MMWR. Morbidity and Mortality Weekly Report. 70 (34): 1167–1169. doi:10.15585/mmwr.mm7034e4. ISSN 0149-2195. PMC 8389394. PMID 34437521.
- ↑ Schreiber, Melody; Chayka, Kyle; Chayka, Kyle; Beyerstein, Lindsay; Beyerstein, Lindsay; Wilson, Jennifer; Wilson, Jennifer; Renault, Marion; Renault, Marion (2021-07-01). "The Delta Covid Variant's Urgent Message for America". The New Republic. ISSN 0028-6583. Retrieved 2021-10-28.
- ↑ "Among the unvaccinated, Delta variant more than doubles risk of hospitalization" Archived 2021-11-08 at the Wayback Machine, Los Angeles Times, 28 August 2021
- ↑ "Coronavirus (COVID-19) booster vaccine". NHS. Government Digital Service. 17 September 2021. Archived from the original on 22 December 2021. Retrieved 11 December 2021.
- ↑ SARS-CoV-2 variants of concern and variants under investigation in England, technical briefing 31 (PDF) (Briefing). Public Health England. 10 December 2021. pp. 3–5, 20–22. GOV-10645. Retrieved 10 December 2021.
- ↑ Callaway, Ewen (21 October 2021). "Mix-and-match COVID vaccines ace the effectiveness test". Nature. doi:10.1038/d41586-021-02853-4. PMID 34675430. S2CID 239455075.
- ↑ 38.0 38.1 38.2 "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 4 December 2021. Retrieved 4 December 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Levin EG, Lustig Y, Cohen C, Fluss R, Indenbaum V, Amit S, et al. (6 October 2021). "Waning Immune Humoral Response to BNT162b2 Covid-19 Vaccine over 6 Months". New England Journal of Medicine. 385 (24): e84. doi:10.1056/NEJMoa2114583. PMC 8522797. PMID 34614326.
- ↑ "COVID-19 Booster Shot". Centers for Disease Control and Prevention. 29 November 2021. Archived from the original on 21 August 2021. Retrieved 4 December 2021.
- ↑ Dolgin, Elie (17 September 2021). "COVID vaccine immunity is waning — how much does that matter?". Nature. 597 (7878): 606–607. Bibcode:2021Natur.597..606D. doi:10.1038/d41586-021-02532-4. PMID 34548661. S2CID 237593988.
- ↑ Montgomery J, Ryan M, Engler R, Hoffman D, McClenathan B, Collins L, et al. (October 2021). "Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military". JAMA Cardiology. 6 (10): 1202–06. doi:10.1001/jamacardio.2021.2833. PMC 8243257. PMID 34185045.
{{cite journal}}: CS1 maint: PMC embargo expired (link) - ↑ Polania Gutierrez JJ, Munakomi S (January 2020). "Intramuscular Injection". StatPearls. PMID 32310581. Archived from the original on 2020-12-08. Retrieved 2022-01-26.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Background document on the mRNA-1273 vaccine (Moderna) against COVID-19 (Report). World Health Organization (WHO). February 2021. hdl:10665/339218. WHO/2019-nCoV/vaccines/SAGE_recommendation/mRNA-1273/background/2021.1. Archived from the original on 2021-06-13. Retrieved 2022-01-26.
- ↑ "Background document on the mRNA-1273 vaccine (Moderna) against COVID-19". World Health Organization (WHO). Archived from the original on 26 January 2022. Retrieved 23 January 2022.
- ↑ "COVID-19 Vaccine Janssen EPAR". European Medicines Agency (EMA). 5 March 2021. Archived from the original on 15 March 2021. Retrieved 16 March 2021. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ↑ "Information about the J&J/Janssen COVID-19 Vaccine". U.S. Centers for Disease Control and Prevention (CDC). 31 March 2021. Archived from the original on 7 April 2021. Retrieved 4 October 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ CDC COVID-19 Response Team (January 2021). "Allergic Reactions Including Anaphylaxis After Receipt of the First Dose of Pfizer-BioNTech COVID-19 Vaccine – United States, December 14–23, 2020" (PDF). MMWR. Morbidity and Mortality Weekly Report. 70 (2): 46–51. doi:10.15585/mmwr.mm7002e1. PMC 7808711. PMID 33444297. Archived (PDF) from the original on 24 January 2021. Retrieved 4 October 2021.
- ↑ "COVID-19 vaccine safety update: Comirnaty" (PDF). European Medicines Agency (EMA). 28 January 2021. Archived (PDF) from the original on 2 June 2021. Retrieved 4 October 2021.
- ↑ 50.0 50.1 "Selected Adverse Events Reported after COVID-19 Vaccination". Centers for Disease Control and Prevention. CDC. 16 November 2021. Archived from the original on 23 November 2021. Retrieved 26 January 2022.
- ↑ "EUA fact sheet for healthcare providers administering vaccine" (PDF). Janssen Therapeutics. 27 August 2021. Archived (PDF) from the original on 29 September 2021. Retrieved 4 October 2021.
- ↑ 52.0 52.1 52.2 Cines DB, Bussel JB (June 2021). "SARS-CoV-2 Vaccine-Induced Immune Thrombotic Thrombocytopenia". The New England Journal of Medicine. 384 (23): 2254–56. doi:10.1056/NEJMe2106315. PMC 8063912. PMID 33861524.
- ↑ Lai CC, Ko WC, Chen CJ, Chen PY, Huang YC, Lee PI, Hsueh PR (August 2021). "COVID-19 vaccines and thrombosis with thrombocytopenia syndrome". Expert Review of Vaccines. Taylor and Francis Group. 20 (8): 1027–35. doi:10.1080/14760584.2021.1949294. PMID 34176415. S2CID 235661210. Archived from the original on 9 October 2021. Retrieved 4 October 2021.
- ↑ Greinacher A, Thiele T, Warkentin TE, Weisser K, Kyrle PA, Eichinger S (June 2021). "Thrombotic Thrombocytopenia after ChAdOx1 nCov-19 Vaccination". The New England Journal of Medicine. 384 (22): 2092–2101. doi:10.1056/NEJMoa2104840. ISSN 0028-4793. PMC 8095372. PMID 33835769.
- ↑ "Use of AstraZeneca COVID-19 vaccine in younger adults". Public Health Agency of Canada. 29 March 2021. Archived from the original on 11 October 2021. Retrieved 4 October 2021.
- ↑ Flanagan KL, Best E, Crawford NW, Giles M, Koirala A, Macartney K, et al. (2020). "Progress and Pitfalls in the Quest for Effective SARS-CoV-2 (COVID-19) Vaccines". Frontiers in Immunology. 11: 579250. doi:10.3389/fimmu.2020.579250. PMC 7566192. PMID 33123165.
- ↑ 57.0 57.1 57.2 57.3 57.4 57.5 57.6 Le TT, Cramer JP, Chen R, Mayhew S (October 2020). "Evolution of the COVID-19 vaccine development landscape". Nature Reviews. Drug Discovery. 19 (10): 667–68. doi:10.1038/d41573-020-00151-8. PMID 32887942. S2CID 221503034.
- ↑ 58.0 58.1 "COVID-19 vaccine tracker (Refresh URL to update)". London School of Hygiene & Tropical Medicine. 12 July 2021. Archived from the original on 11 October 2020. Retrieved 10 March 2021.
- ↑ Arbeitman CR, Rojas P, Ojeda-May P, Garcia ME (September 2021). "The SARS-CoV-2 spike protein is vulnerable to moderate electric fields". Nature Communications. 12 (1): 5407. arXiv:2103.12733. Bibcode:2021NatCo..12.5407A. doi:10.1038/s41467-021-25478-7. PMC 8437970. PMID 34518528.
- ↑ 60.0 60.1 Grifoni A, Weiskopf D, Ramirez SI, Mateus J, Dan JM, Moderbacher CR, et al. (June 2020). "Targets of T Cell Responses to SARS-CoV-2 Coronavirus in Humans with COVID-19 Disease and Unexposed Individuals". Cell. 181 (7): 1489–1501.e15. doi:10.1016/j.cell.2020.05.015. PMC 7237901. PMID 32473127.
- ↑ Dutta NK, Mazumdar K, Gordy JT (June 2020). Dutch RE (ed.). "The Nucleocapsid Protein of SARS-CoV-2: a Target for Vaccine Development". Journal of Virology. 94 (13). doi:10.1128/JVI.00647-20. PMC 7307180. PMID 32546606.
- ↑ Nikolaidis M, Markoulatos P, Van de Peer Y, Oliver SG, Amoutzias GD (October 2021). Hepp C (ed.). "The neighborhood of the Spike gene is a hotspot for modular intertypic homologous and non-homologous recombination in Coronavirus genomes". Molecular Biology and Evolution. 39: msab292. doi:10.1093/molbev/msab292. PMC 8549283. PMID 34638137.
- ↑ 63.0 63.1 63.2 63.3 63.4 Thanh Le T, Andreadakis Z, Kumar A, Gómez Román R, Tollefsen S, Saville M, Mayhew S (May 2020). "The COVID-19 vaccine development landscape". Nature Reviews. Drug Discovery. 19 (5): 305–06. doi:10.1038/d41573-020-00073-5. PMID 32273591.
- ↑ 64.0 64.1 64.2 Diamond MS, Pierson TC (May 2020). "The Challenges of Vaccine Development against a New Virus during a Pandemic". Cell Host & Microbe. 27 (5): 699–703. doi:10.1016/j.chom.2020.04.021. PMC 7219397. PMID 32407708.
- ↑ Cross R (29 September 2020). "The tiny tweak behind COVID-19 vaccines". Chemical & Engineering News. 98 (38). Archived from the original on 16 February 2021. Retrieved 26 January 2022.
- ↑ Krammer F (October 2020). "SARS-CoV-2 vaccines in development". Nature. 586 (7830): 516–527. Bibcode:2020Natur.586..516K. doi:10.1038/s41586-020-2798-3. PMID 32967006. S2CID 221887746.
- ↑ Park KS, Sun X, Aikins ME, Moon JJ (February 2021). "Non-viral COVID-19 vaccine delivery systems". Advanced Drug Delivery Reviews. 169: 137–151. doi:10.1016/j.addr.2020.12.008. ISSN 0169-409X. PMC 7744276. PMID 33340620.
- ↑ Kowalski PS, Rudra A, Miao L, Anderson DG (April 2019). "Delivering the Messenger: Advances in Technologies for Therapeutic mRNA Delivery". Molecular Therapy. 27 (4): 710–728. doi:10.1016/j.ymthe.2019.02.012. PMC 6453548. PMID 30846391.
- ↑ Verbeke R, Lentacker I, De Smedt SC, Dewitte H (October 2019). "Three decades of messenger RNA vaccine development". Nano Today. 28: 100766. doi:10.1016/j.nantod.2019.100766. hdl:1854/LU-8628303. S2CID 202221207. Archived from the original on 2021-10-09. Retrieved 2022-01-26.
- ↑ "COVID-19 ACIP Vaccine Recommendations". U.S. Centers for Disease Control and Prevention (CDC). Archived from the original on 3 November 2021. Retrieved 18 February 2021.
- ↑ "Safe COVID-19 vaccines for Europeans". European Commission. Archived from the original on 4 November 2021. Retrieved 19 February 2021.
- ↑ "Regulatory Decision Summary – Pfizer–BioNTech COVID-19 Vaccine". Health Canada, Government of Canada. 9 December 2020. Archived from the original on 30 January 2021. Retrieved 9 December 2020.
- ↑ "Study to Describe the Safety, Tolerability, Immunogenicity, and Efficacy of RNA Vaccine Candidates Against COVID-19 in Healthy Adults". ClinicalTrials.gov. 30 April 2020. NCT04368728. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ "A Multi-site Phase I/II, 2-Part, Dose-Escalation Trial Investigating the Safety and Immunogenicity of four Prophylactic SARS-CoV-2 RNA Vaccines Against COVID-19 Using Different Dosing Regimens in Healthy Adults". EU Clinical Trials Register. 14 April 2020. EudraCT 2020-001038-36. Archived from the original on 22 April 2020. Retrieved 22 April 2020.
- ↑ "A Study to Evaluate Efficacy, Safety, and Immunogenicity of mRNA-1273 Vaccine in Adults Aged 18 Years and Older to Prevent COVID-19". ClinicalTrials.gov. 14 July 2020. NCT04470427. Archived from the original on 11 October 2020. Retrieved 27 July 2020.
- ↑ Palca J (27 July 2020). "COVID-19 vaccine candidate heads to widespread testing in U.S." NPR. Archived from the original on 11 October 2020. Retrieved 27 July 2020.
- ↑ "CureVac Final Data from Phase 2b/3 Trial of First-Generation COVID-19 Vaccine Candidate, CVnCoV, Demonstrates Protection in Age Group of 18 to 60". CureVac (Press release). 30 June 2021. Archived from the original on 12 October 2021. Retrieved 2 July 2021.
- ↑ 78.0 78.1 78.2 Moghimi SM (March 2021). "Allergic Reactions and Anaphylaxis to LNP-Based COVID-19 Vaccines". Molecular Therapy. 29 (3): 898–900. doi:10.1016/j.ymthe.2021.01.030. PMC 7862013. PMID 33571463.
- ↑ 79.0 79.1 "What are viral vector-based vaccines and how could they be used against COVID-19?". Gavi, the Vaccine Alliance (GAVI). 2020. Archived from the original on 11 November 2021. Retrieved 26 January 2021.
- ↑ "Understanding Viral Vector COVID-19 Vaccines". U.S. Centers for Disease Control and Prevention (CDC). 13 April 2021. Archived from the original on 13 November 2021. Retrieved 19 April 2021.
- ↑ "Investigating a Vaccine Against COVID-19". ClinicalTrials.gov. 26 May 2020. NCT04400838. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ "A Phase 2/3 study to determine the efficacy, safety and immunogenicity of the candidate Coronavirus Disease (COVID-19) vaccine ChAdOx1 nCoV-19". EU Clinical Trials Register. 21 April 2020. EudraCT 2020-001228-32. Archived from the original on 5 October 2020. Retrieved 3 August 2020.
- ↑ O'Reilly P (26 May 2020). "A Phase III study to investigate a vaccine against COVID-19". ISRCTN Registry. doi:10.1186/ISRCTN89951424. ISRCTN89951424.
- ↑ Corum J, Carl Z (8 January 2021). "How Gamaleya's Vaccine Works". The New York Times. Archived from the original on 20 April 2021. Retrieved 27 January 2021.
- ↑ "A Study of Ad26.COV2.S in Adults". 4 August 2020. Archived from the original on 16 September 2020. Retrieved 23 August 2020.
- ↑ "A Study of Ad26.COV2.S for the Prevention of SARS-CoV-2-Mediated COVID-19 in Adult Participants". US National Library of Medicine. Archived from the original on 26 September 2020.
- ↑ Johnson C, McGinley L. "Johnson & Johnson seeks emergency FDA authorization for single-shot coronavirus vaccine". The Washington Post. Archived from the original on 2021-02-05. Retrieved 2022-01-26.
- ↑ "It's not just Johnson & Johnson: China has a single-dose COVID-19 vaccine that's 65% effective". Fortune. Archived from the original on 8 August 2021. Retrieved 28 February 2021.
- ↑ Wu S, Zhong G, Zhang J, Shuai L, Zhang Z, Wen Z, et al. (August 2020). "A single dose of an adenovirus-vectored vaccine provides protection against SARS-CoV-2 challenge". Nat Commun. 11 (1): 4081. Bibcode:2020NatCo..11.4081W. doi:10.1038/s41467-020-17972-1. PMC 7427994. PMID 32796842.
- ↑ "Single dose vaccine, Sputnik Light, authorized for use in Russia". Sputnik V. Archived from the original on 14 November 2021. Retrieved 12 August 2021.
- ↑ "Introducing a new member of the Sputnik family – a single dose Sputnik Light!". Twitter. Archived from the original on 2021-10-18. Retrieved 2021-08-12.
- ↑ Petrovsky N, Aguilar JC (October 2004). "Vaccine adjuvants: current state and future trends". Immunology and Cell Biology. 82 (5): 488–496. doi:10.1111/j.0818-9641.2004.01272.x. PMID 15479434. S2CID 154670.
- ↑ "Safety and Immunogenicity Study of Inactivated Vaccine for Prevention of SARS-CoV-2 Infection (COVID-19) (Renqiu)". ClinicalTrials.gov. 12 May 2020. NCT04383574. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ "Clinical Trial of Efficacy and Safety of Sinovac's Adsorbed COVID-19 (Inactivated) Vaccine in Healthcare Professionals (PROFISCOV)". ClinicalTrials.gov. 2 July 2020. NCT04456595. Archived from the original on 11 October 2020. Retrieved 3 August 2020.
- ↑ PT. Bio Farma (10 August 2020). "A Phase III, observer-blind, randomized, placebo-controlled study of the efficacy, safety, and immunogenicity of SARS-COV-2 inactivated vaccine in healthy adults aged 18–59 years in Indonesia". Registri Penyakit Indonesia. Archived from the original on 11 October 2020. Retrieved 15 August 2020.
- ↑ Chen W, Al Kaabi N (18 July 2020). "A Phase III clinical trial for inactivated novel coronavirus pneumonia (COVID-19) vaccine (Vero cells)". Chinese Clinical Trial Registry. Archived from the original on 11 October 2020. Retrieved 15 August 2020.
- ↑ Ivanova P (20 February 2021). "Russia approves its third COVID-19 vaccine, CoviVac". Reuters. Archived from the original on 28 February 2021. Retrieved 11 April 2021.
- ↑ "Kazakhstan rolls out its own COVID-19 vaccine". Reuters. 27 April 2021. Archived from the original on 4 November 2021. Retrieved 2 July 2021.
- ↑ "FarsNews Agency Iran Licenses Emergency Injection of Home-Made Anti-Coronavirus Vaccine". Fars News Agency. 14 June 2021. Archived from the original on 9 October 2021. Retrieved 25 August 2021.
- ↑ "VLA2001 COVID-19 Vaccine". Precision Vaccinations. 31 December 2020. Archived from the original on 13 January 2021. Retrieved 11 January 2021.
- ↑ "Dose Finding Study to Evaluate Safety, Tolerability and Immunogenicity of an Inactivated Adjuvanted Sars-Cov-2 Virus Vaccine Candidate Against Covid-19 in Healthy Adults". U.S. National Library of Medicine. 30 December 2020. Archived from the original on 14 February 2021. Retrieved 11 January 2021.
- ↑ "Module 2 – Subunit vaccines". WHO Vaccine Safety Basics. Archived from the original on 2021-03-20. Retrieved 2022-01-26.
- ↑ "Study of the Safety, Reactogenicity and Immunogenicity of "EpiVacCorona" Vaccine for the Prevention of COVID-19 (EpiVacCorona)". ClinicalTrials.gov. 22 September 2020. NCT04368988. Archived from the original on 29 June 2021. Retrieved 16 November 2020.
- ↑ "MVC COVID-19 Vaccine Obtains Taiwan EUA Approval". Medigen Vaccine Biologics. Archived from the original on 27 November 2021. Retrieved 7 August 2021.
- ↑ Achom, Debanish (28 December 2021). "India Clears 2 New Vaccines And Merck's Covid Pill: 10 Points". NDTV.com. Archived from the original on 28 December 2021. Retrieved 19 January 2022.
- ↑ Bottazzi, Maria Elena; Hotez, Peter J. (30 December 2021). "A COVID Vaccine for All". Scientific American. Archived from the original on 30 December 2021. Retrieved 19 January 2022.
- ↑ "Evaluation of the Safety and Immunogenicity of a SARS-CoV-2 rS (COVID-19) Nanoparticle Vaccine With/Without Matrix-M Adjuvant". ClinicalTrials.gov. 30 April 2020. NCT04368988. Archived from the original on 14 July 2020. Retrieved 14 July 2020.
- ↑ "A Study on the Safety, Tolerability and Immune Response of SARS-CoV-2 Sclamp (COVID-19) Vaccine in Healthy Adults". ClinicalTrials.gov. 3 August 2020. NCT04495933. Archived from the original on 11 October 2020. Retrieved 4 August 2020.
- ↑ "UQ-CSL V451 Vaccine". Precision Vaccinations. Archived from the original on 19 December 2020. Retrieved 11 December 2020.
- ↑ "A prospective, randomized, adaptive, phase I/II clinical study to evaluate the safety and immunogenicity of Novel Corona Virus −2019-nCov vaccine candidate of M/s Cadila Healthcare Limited by intradermal route in healthy subjects". India: Clinical Trials Registry. 15 December 2020. CTRI/2020/07/026352. Archived from the original on 22 November 2020.
- ↑ "Safety, Tolerability and Immunogenicity of INO-4800 for COVID-19 in Healthy Volunteers". ClinicalTrials.gov. 7 April 2020. NCT04336410. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ "IVI, INOVIO, and KNIH to partner with CEPI in a Phase I/II clinical trial of INOVIO's COVID-19 DNA vaccine in South Korea". International Vaccine Institute. 16 April 2020. Archived from the original on 24 September 2020. Retrieved 23 April 2020.
- ↑ "Study of COVID-19 DNA Vaccine (AG0301-COVID19)". ClinicalTrials.gov. 9 July 2020. NCT04463472. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ "Safety and Immunogenicity Study of GX-19, a COVID-19 Preventive DNA Vaccine in Healthy Adults". ClinicalTrials.gov. 24 June 2020. NCT04445389. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ "S. Korea's Genexine begins human trial of coronavirus vaccine". Reuters. 19 June 2020. Archived from the original on 11 October 2020. Retrieved 25 June 2020.
- ↑ Chang LJ (9 March 2020). "Safety and Immunity of Covid-19 aAPC Vaccine". ClinicalTrials.gov. NCT04299724. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ "Immunity and Safety of Covid-19 Synthetic Minigene Vaccine". ClinicalTrials.gov. 19 February 2020. NCT04276896. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ "A Phase I/II Randomized, Multi-Center, Placebo-Controlled, Dose-Escalation Study to Evaluate the Safety, Immunogenicity and Potential Efficacy of an rVSV-SARS-CoV-2-S Vaccine (IIBR-100) in Adults". ClinicalTrials.gov. 1 November 2020. NCT04608305. Archived from the original on 3 May 2021. Retrieved 26 January 2022.
- ↑ Johnson CY, Mufson S (11 June 2020). "Can old vaccines from science's medicine cabinet ward off coronavirus?". The Washington Post. ISSN 0190-8286. Archived from the original on 11 June 2020. Retrieved 31 December 2020.
- ↑ "Bacille Calmette-Guérin (BCG) vaccination and COVID-19". World Health Organization (WHO). 12 April 2020. Archived from the original on 30 April 2020. Retrieved 1 May 2020.
- ↑ 121.0 121.1 121.2 Tregoning JS, Russell RF, Kinnear E (March 2018). "Adjuvanted influenza vaccines". Human Vaccines & Immunotherapeutics. 14 (3): 550–564. doi:10.1080/21645515.2017.1415684. PMC 5861793. PMID 29232151.
- ↑ 122.0 122.1 122.2 122.3 Wang J, Peng Y, Xu H, Cui Z, Williams RO (August 2020). "The COVID-19 Vaccine Race: Challenges and Opportunities in Vaccine Formulation". AAPS PharmSciTech. 21 (6): 225. doi:10.1208/s12249-020-01744-7. PMC 7405756. PMID 32761294.
- ↑ Taylor R (2 November 2021). "Sequences of Covid-19 vaccines released via WhatDoTheyKnow". mySociety. Archived from the original on 5 November 2021. Retrieved 2 November 2021.
- ↑ Simpson S, Kaufmann MC, Glozman V, Chakrabarti A (May 2020). "Disease X: accelerating the development of medical countermeasures for the next pandemic". The Lancet. Infectious Diseases. 20 (5): e108–15. doi:10.1016/S1473-3099(20)30123-7. PMC 7158580. PMID 32197097.
- ↑ 125.0 125.1 125.2 125.3 Sanger DE, Kirkpatrick DD, Zimmer C, Thomas K, Wee SL (2 May 2020). "With Pressure Growing, Global Race for a Vaccine Intensifies". The New York Times. ISSN 0362-4331. Archived from the original on 11 May 2020. Retrieved 2 May 2020.
- ↑ Zabaleta N, Dai W, Bhatt U, Hérate C, Maisonnasse P, Chichester JA, et al. (August 2021). "An AAV-based, room-temperature-stable, single-dose COVID-19 vaccine provides durable immunogenicity and protection in non-human primates". Cell Host & Microbe. 29 (9): 1437–1453.e8. doi:10.1016/j.chom.2021.08.002. PMC 8346325. PMID 34428428. S2CID 231676030.
- ↑ 127.0 127.1 127.2 127.3 127.4 127.5 127.6 Steenhuysen J, Eisler P, Martell A, Nebehay S (27 April 2020). "Special Report: Countries, companies risk billions in race for coronavirus vaccine". Reuters. Archived from the original on 15 May 2020. Retrieved 2 May 2020.
- ↑ Jeong-ho L, Zheng W, Zhou L (26 January 2020). "Chinese scientists race to develop vaccine as coronavirus death toll jumps". South China Morning Post. Archived from the original on 26 January 2020. Retrieved 28 January 2020.
- ↑ Wee SL (4 May 2020). "China's coronavirus vaccine drive empowers a troubled industry". The New York Times. ISSN 0362-4331. Archived from the original on 4 May 2020. Retrieved 4 May 2020.
- ↑ Thorp HH (March 2020). "Underpromise, overdeliver". Science. 367 (6485): 1405. Bibcode:2020Sci...367.1405T. doi:10.1126/science.abb8492. PMID 32205459.
- ↑ Blackwell T (20 April 2020). "COVID-19 vaccine researchers say pandemic lockdown placing many serious obstacles to their work". National Post. Archived from the original on 23 April 2020. Retrieved 3 May 2020.
- ↑ Chen J (4 May 2020). "Covid-19 has shuttered labs. It could put a generation of researchers at risk". Stat. Archived from the original on 6 May 2020. Retrieved 4 May 2020.
- ↑ "Vaccine Safety – Vaccines". US Department of Health and Human Services. Archived from the original on 22 April 2020. Retrieved 13 April 2020.
- ↑ "The drug development process". U.S. Food and Drug Administration (FDA). 4 January 2018. Archived from the original on 22 February 2020. Retrieved 12 April 2020.
- ↑ Cohen J (June 2020). "Pandemic vaccines are about to face the real test". Science. 368 (6497): 1295–96. Bibcode:2020Sci...368.1295C. doi:10.1126/science.368.6497.1295. PMID 32554572.
- ↑ Dubé E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J (August 2013). "Vaccine hesitancy: an overview". Human Vaccines & Immunotherapeutics. 9 (8): 1763–73. doi:10.4161/hv.24657. PMC 3906279. PMID 23584253.
- ↑ Howard J, Stracqualursi V (18 June 2020). "Fauci warns of 'anti-science bias' being a problem in US". CNN. Archived from the original on 21 June 2020. Retrieved 21 June 2020.
- ↑ "Vaccines: The Emergency Authorisation Procedure". European Medicines Agency (EMA). 2020. Archived from the original on 24 September 2020. Retrieved 21 August 2020.
- ↑ Byrne J (19 October 2020). "Moderna COVID-19 vaccine under rolling review process in Canada, EU". BioPharma-Reporter.com, William Reed Business Media Ltd. Archived from the original on 25 February 2021. Retrieved 25 November 2020.
- ↑ Dangerfield K (20 November 2020). "Pfizer files for emergency use of coronavirus vaccine in U.S. – what about in Canada?". Global News. Archived from the original on 25 January 2021. Retrieved 25 November 2020.
- ↑ "G20 launches initiative for health tools needed to combat the coronavirus". The Globe and Mail. 25 April 2020. Archived from the original on 27 April 2020. Retrieved 26 January 2022.
- ↑ "Access to COVID-19 Tools (ACT) Accelerator" (PDF). World Health Organization (WHO). 24 April 2020. Archived (PDF) from the original on 25 April 2020. Retrieved 26 January 2022.
- ↑ "The ACT-Accelerator: frequently asked questions (FAQ)". World Health Organization (WHO). 2020. Archived from the original on 4 May 2021. Retrieved 16 December 2020.
- ↑ 144.0 144.1 144.2 "Update on WHO Solidarity Trial – Accelerating a safe and effective COVID-19 vaccine". World Health Organization (WHO). 27 April 2020. Archived from the original on 30 April 2020. Retrieved 2 May 2020.
It is vital that we evaluate as many vaccines as possible as we cannot predict how many will turn out to be viable. To increase the chances of success (given the high level of attrition during vaccine development), we must test all candidate vaccines until they fail. [The] WHO is working to ensure that all of them have the chance of being tested at the initial stage of development. The results for the efficacy of each vaccine are expected within three to six months, and this evidence, combined with data on safety, will inform decisions about whether it can be used on a wider scale.
- ↑ Abedi M (23 March 2020). "Canada to spend $192M on developing COVID-19 vaccine". Global News. Archived from the original on 9 April 2020. Retrieved 24 March 2020.
- ↑ "Government of Canada's research response to COVID-19". Government of Canada. 23 April 2020. Archived from the original on 13 May 2020. Retrieved 4 May 2020.
- ↑ Takada N, Satake M (2 May 2020). "US and China unleash wallets in race for coronavirus vaccine". Nikkei Asian Review. Archived from the original on 10 May 2020. Retrieved 3 May 2020.
- ↑ Morriss E (22 April 2020). "Government launches coronavirus vaccine taskforce as human clinical trials start". Pharmafield. Archived from the original on 26 June 2020. Retrieved 3 May 2020.
- ↑ Kuznia R, Polglase K, Mezzofiore G (1 May 2020). "In quest for vaccine, US makes 'big bet' on company with unproven technology". CNN. Archived from the original on 13 May 2020. Retrieved 2 May 2020.
- ↑ Cohen J (May 2020). "U.S. 'Warp Speed' vaccine effort comes out of the shadows". Science. 368 (6492): 692–93. Bibcode:2020Sci...368..692C. doi:10.1126/science.368.6492.692. PMID 32409451.
- ↑ Sink J, Fabian J, Griffin R (15 May 2020). "Trump introduces 'Warp Speed' leaders to hasten COVID-19 vaccine". Bloomberg. Archived from the original on 21 May 2020. Retrieved 15 May 2020.
- ↑ LaHucik K (17 June 2021). "U.S. injects $3B-plus into COVID-19 research to develop antiviral pill within a year". Fierce Biotech. Archived from the original on 9 October 2021. Retrieved 11 July 2021.
- ↑ Ritchie, Hannah; Mathieu, Edouard; Rodés-Guirao, Lucas; Appel, Cameron; Giattino, Charlie; Ortiz-Ospina, Esteban; Hasell, Joe; Macdonald, Bobbie; Beltekian, Diana; Dattani, Saloni; Roser, Max (2020–2022). "Coronavirus Pandemic (COVID-19)". Our World in Data. Retrieved 2023-04-07.
- ↑ Richie H., Ortiz-Ospina E, Beltekian D, Methieu E, Hasell J., Macdonald B., Giattino C., Appel C., Rodes-Guirao L., Roser M. (1 September 2021). "Coronavirus (COVID-19) Vaccinations - Statistics and Research". Our World in Data. Archived from the original on 10 March 2021. Retrieved 26 January 2022.
{{cite journal}}: CS1 maint: uses authors parameter (link) - ↑ 155.0 155.1 Gates B (April 2020). "Responding to Covid-19 - A Once-in-a-Century Pandemic?". The New England Journal of Medicine. 382 (18): 1677–1679. doi:10.1056/nejmp2003762. PMID 32109012.
- ↑ Weintraub R, Yadav P, Berkley S (2 April 2020). "A COVID-19 vaccine will need equitable, global distribution". Harvard Business Review. ISSN 0017-8012. Archived from the original on 9 June 2020. Retrieved 9 June 2020.
- ↑ Gartner A, Roberts L (3 May 2020). "How close are we to a coronavirus vaccine? Latest news on UK trials". The Telegraph. ISSN 0307-1235. Archived from the original on 4 May 2020. Retrieved 3 May 2020.
- ↑ Le TT, Cramer JP, Chen R, Mayhew S (October 2020). "Evolution of the COVID-19 vaccine development landscape". Nature Reviews. Drug Discovery. 19 (10): 667–668. doi:10.1038/d41573-020-00151-8. PMID 32887942. S2CID 221503034.
- ↑ Yamey G, Schäferhoff M, Hatchett R, Pate M, Zhao F, McDade KK (May 2020). "Ensuring global access to COVID-19 vaccines". Lancet. 395 (10234): 1405–1406. doi:10.1016/S0140-6736(20)30763-7. PMC 7271264. PMID 32243778.
CEPI estimates that developing up to three vaccines in the next 12–18 months will require an investment of at least US$2 billion. This estimate includes Phase 1 clinical trials of eight vaccine candidates, progression of up to six candidates through Phase 2 and 3 trials, completion of regulatory and quality requirements for at least three vaccines, and enhancing global manufacturing capacity for three vaccines.
- ↑ "An international randomised trial of candidate vaccines against COVID-19: Outline of Solidarity vaccine trial" (PDF). World Health Organization. 9 April 2020. Archived (PDF) from the original on 12 May 2020. Retrieved 9 May 2020.
- ↑ "COVAX: Ensuring global equitable access to COVID-19 vaccines". GAVI. 2020. Archived from the original on 25 September 2020. Retrieved 28 August 2020.
- ↑ "R&D Blueprint: A coordinated global research roadmap – 2019 novel coronavirus" (PDF). World Health Organization. 1 March 2020. Archived (PDF) from the original on 15 May 2020. Retrieved 10 May 2020.
- ↑ "WHO, UN set out steps to meet world COVID vaccination targets". 7 October 2021. Archived from the original on 31 December 2021. Retrieved 31 December 2021.
- ↑ "COVID-19: WHO calls on countries to vaccinate 70% of their population by mid-2022". 29 December 2021. Archived from the original on 31 December 2021. Retrieved 31 December 2021.
- ↑ "Covid-19 vaccinations: African nations miss WHO target". BBC. 31 December 2021. Archived from the original on 31 December 2021. Retrieved 31 December 2021.
- ↑ 166.0 166.1 166.2 166.3 The Lancet Infectious Diseases (September 2021). "COVID-19 vaccine equity and booster doses". The Lancet. Infectious Diseases. 21 (9): 1193. doi:10.1016/S1473-3099(21)00486-2. ISSN 1473-3099. PMC 8360703. PMID 34391506.
- ↑ 167.0 167.1 So AD, Woo J (December 2020). "Reserving coronavirus disease 2019 vaccines for global access: cross sectional analysis". BMJ. 371: m4750. doi:10.1136/bmj.m4750. PMC 7735431. PMID 33323376.
- ↑ Adhanom Ghebreyesus T (18 January 2021). "WHO Director-General's opening remarks at 148th session of the Executive Board". World Health Organization (WHO). Archived from the original on 12 November 2021. Retrieved 25 January 2021.
- ↑ "U.S. pressured Brazil to ditch Russia's Sputnik V vaccine". The Brazilian Report. 15 March 2021. Archived from the original on 15 March 2021. Retrieved 21 March 2021.
- ↑ Holmes O (16 February 2021). "Israel blocked Covid vaccines from entering Gaza, say Palestinians". The Guardian. Archived from the original on 16 February 2021. Retrieved 17 February 2021.
- ↑ Rasgon A (4 February 2021). "Israel's Vaccine Success Unleashes a Debate on Palestinian Inequities". The New York Times. Archived from the original on 17 February 2021. Retrieved 17 February 2021.
- ↑ Horton C (17 February 2021). "Taiwan Concerned China May Have Blocked Vaccine Purchase". Bloomberg. Archived from the original on 17 February 2021. Retrieved 17 February 2021.
- ↑ "Playing Politics with Poverty: Sisi's COVID-19 Vaccine Strategy". Carnegie Endowment for International Peace. Archived from the original on 28 February 2021. Retrieved 25 February 2021.
- ↑ Strazewski L (9 February 2021). "Dr. Fauci: Variants reveal COVID-19 vaccination as global job". American Medical Association. Archived from the original on 10 October 2021. Retrieved 4 March 2021.
- ↑ Bergmark E, Wierson A (26 February 2021). "Opinion: Without a global vaccine plan, coronavirus variants could lead to untold number of deaths". CNN. Archived from the original on 19 October 2021. Retrieved 4 March 2021.
- ↑ Blenkinsop P, Maclean W, Ellis A (10 March 2021). "Rich, developing nations wrangle over COVID vaccine patents". Reuters. Archived from the original on 11 March 2021. Retrieved 19 June 2021.
- ↑ Macias AM, Breuninger K, Franck (5 May 2021). "U.S. backs waiving patent protections for Covid vaccines, citing global health crisis". CNBC. Archived from the original on 5 May 2021. Retrieved 5 May 2021.
- ↑ Sánchez Nicolás E (11 June 2021). "Pressure builds on EU to back WTO vaccine-patent waiver". EUobserver. Archived from the original on 19 October 2021. Retrieved 14 June 2021.
- ↑ "WHO says against proof of Covid-19 vaccination for international travel". South China Morning Post. 20 April 2021. Archived from the original on 3 May 2021. Retrieved 17 May 2021.
- ↑ Goodman PS, Mandavilli A, Robbins R, Stevis-Gridneff M (15 May 2021). "What Would It Take to Vaccinate the World Against Covid?". The New York Times. ISSN 0362-4331. Archived from the original on 12 November 2021. Retrieved 17 May 2021.
- ↑ Muniz B, Fonseca B, Fernandes L, Pina R (15 March 2021). "Brasil registra duas vezes mais pessoas brancas vacinadas que negras" [Brazil registers twice as many white people vaccinated as black people]. Agência Pública (in português do Brasil). Archived from the original on 15 March 2021. Retrieved 28 May 2021.
- ↑ Schnirring L (17 May 2021). "UN agencies make urgent appeal for COVAX vaccine doses". CIDRAP. Archived from the original on 31 October 2021. Retrieved 15 June 2021.
- ↑ "First Meeting of the Task Force on COVID-19 Vaccines, Therapeutics and Diagnostics for Developing Countries". World Health Organization (WHO). 30 June 2021. Archived from the original on 19 October 2021. Retrieved 5 July 2021.
- ↑ Tapper J, McKie R (3 July 2021). "Vaccines 'outpaced by variants', WHO warns, as Delta now in 98 countries". The Guardian. Archived from the original on 21 October 2021. Retrieved 5 July 2021.
- ↑ Mahase E (July 2021). "Covid-19: Countries dump vaccines as demand slumps and sharing proves difficult". BMJ. 374: n1893. doi:10.1136/bmj.n1893. PMID 34315725. S2CID 236457553. Archived from the original on 8 August 2021. Retrieved 10 August 2021.
- ↑ Levin D (1 August 2021). "The U.S. is wasting vaccine doses, even as cases rise and other countries suffer shortages". The New York Times. Archived from the original on 9 August 2021. Retrieved 10 August 2021.
- ↑ "Covid-19 vaccines: Why some African states can't use their vaccines". BBC News. 8 June 2021. Archived from the original on 14 November 2021. Retrieved 20 August 2021.
- ↑ "G7 support for pharma monopolies is putting millions of lives at risk" (Press release). Amnesty International. 10 June 2021. Archived from the original on 19 October 2021. Retrieved 20 August 2021.
- ↑ "Vaccine monopolies make cost of vaccinating the world against COVID at least 5 times more expensive than it could be" (Press release). Oxfam International. 29 July 2021. Archived from the original on 10 January 2022. Retrieved 20 August 2021.
- ↑ Stiglitz, Joseph (15 December 2021). "If Olaf Scholz is serious about progress, he must back a patent waiver for Covid vaccines". The Guardian. Archived from the original on 15 December 2021. Retrieved 15 December 2021.
- ↑ "Countries must not let another opportunity slip by to advance the global waiver on overcoming COVID-19 medical-tool monopolies". Médecins Sans Frontières (MSF)/Doctors Without Borders. 13 September 2021. Archived from the original on 10 October 2021. Retrieved 23 September 2021.
- ↑ "MSF calls for no patents or profiteering on COVID-19 drugs and vaccines / No profiteering on COVID-19 drugs and vaccines, says MSF". Médecins Sans Frontières (MSF) International. Archived from the original on 2020-12-11. Retrieved 2022-01-26.
- ↑ "Governments must act fast on consensus supporting historic move to suspend monopolies during pandemic / COVID-19: Governments must build consensus around waiver". Médecins Sans Frontières (MSF) International. Archived from the original on 2021-10-23. Retrieved 2022-01-26.
- ↑ "The WHO is right to call a temporary halt to COVID vaccine boosters". Nature. 596 (7872): 317. 17 August 2021. Bibcode:2021Natur.596..317.. doi:10.1038/d41586-021-02219-w. PMID 34404945. S2CID 237199262.
- ↑ "WHO slams wealthy nations' rush towards Covid booster shots while millions worldwide lack first jab". France 24. Agence France-Presse. 18 August 2021. Archived from the original on 2 November 2021. Retrieved 21 August 2021.
- ↑ Kramer J (18 August 2021). "The U.S. plans to authorize boosters—but many already got a third dose". National Geographic. Archived from the original on 10 October 2021. Retrieved 21 August 2021.
- ↑ "More than 140 former heads of state and Nobel laureates call on candidates for German chancellor to waive intellectual property rules for COVID-19 vaccines". Oxfam International. 14 September 2021. Archived from the original on 19 October 2021. Retrieved 22 September 2021.
- ↑ Walker, Peter (29 November 2021). "Nursing unions around world call for UN action on Covid vaccine patents". The Guardian. Archived from the original on 29 November 2021. Retrieved 29 November 2021.
- ↑ Psaledakis D (22 September 2021). "Developing nations' plea to world's wealthy at U.N.: stop vaccine hoarding". Reuters. Archived from the original on 10 November 2021. Retrieved 29 September 2021.
- ↑ PERÚ, Empresa Peruana de Servicios Editoriales S. A. EDITORA. "Peru: President suggests global agreement at UN ensuring universal access to vaccines". Andina (in español). Archived from the original on 30 October 2021. Retrieved 29 September 2021.
- ↑ Baraniuk C (February 2021). "Covid-19: How the UK vaccine rollout delivered success, so far". BMJ. 372: n421. doi:10.1136/bmj.n421. PMID 33602672. S2CID 231946710.
- ↑ "Additional Dose of mRNA COVID‑19 Vaccine for Patients Who Are Immunocompromised". U.S. Centers for Disease Control and Prevention (CDC). 13 August 2021. Archived from the original on 7 October 2021. Retrieved 16 August 2021.
- ↑ "France plans rollout of Covid vaccine booster shots – but only for the vulnerable". France 24. 4 August 2021. Archived from the original on 22 October 2021. Retrieved 16 August 2021.
- ↑ "Israel to offer 3rd COVID booster shot to older citizens". Associated Press. 29 July 2021. Archived from the original on 31 October 2021. Retrieved 16 August 2021.
- ↑ Hunziker P (24 July 2021). "Personalized-dose Covid-19 vaccination in a wave of virus Variants of Concern: Trading individual efficacy for societal benefit". Precision Nanomedicine. 4 (3): 805–820. doi:10.33218/001c.26101. Archived from the original on 9 October 2021. Retrieved 26 January 2022.
- ↑ Thompson MG, Burgess JL, Naleway AL, Tyner HL, Yoon SK, Meece J, et al. (April 2021). "Interim Estimates of Vaccine Effectiveness of BNT162b2 and mRNA-1273 COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Health Care Personnel, First Responders, and Other Essential and Frontline Workers - Eight U.S. Locations, December 2020-March 2021" (PDF). MMWR Morb Mortal Wkly Rep. 70 (13): 495–500. doi:10.15585/mmwr.mm7013e3. PMC 8022879. PMID 33793460. Archived (PDF) from the original on 2021-08-28. Retrieved 2022-01-26.
- ↑ CDC (11 February 2020). "When You've Been Fully Vaccinated". U.S. Centers for Disease Control and Prevention (CDC). Archived from the original on 28 July 2021. Retrieved 29 April 2021.
- ↑ 208.0 208.1 "COVID vaccines: Widening inequality and millions vulnerable". United Nations. 19 September 2021. Archived from the original on 31 December 2021. Retrieved 30 October 2021.
- ↑ "Impact of vaccine inequity on economic recovery". UN Development program. Archived from the original on 2021-11-03. Retrieved 2022-01-26.
- ↑ Elliott L (5 October 2021). "IMF cuts global economic forecast as pandemic 'hobbles' growth". The Guardian. Archived from the original on 27 October 2021. Retrieved 6 October 2021.
- ↑ "Refugees face dire consequences from COVID-19 underfunding, UNHCR warns". United Nations. 17 September 2021. Archived from the original on 30 October 2021. Retrieved 30 October 2021.
- ↑ 212.0 212.1 Azar A (4 February 2020). "Notice of Declaration under the Public Readiness and Emergency Preparedness Act for medical countermeasures against COVID-19". Archived from the original on 25 April 2020. Retrieved 22 April 2020.
- ↑ Lintern S (2 December 2020). "Pfizer given protection from legal action over coronavirus vaccine by UK government". The Independent. Archived from the original on 5 May 2021. Retrieved 8 May 2021.
- ↑ "Questions and Answers: Conditional Marketing Authorisation of COVID-19 Vaccines in the EU". European Commission. 11 December 2020. Question: What is the difference in liability between EU Conditional Marketing Authorisation vs Emergency Use Authorisations?. Archived from the original on 4 October 2021. Retrieved 29 December 2020.
- ↑ Haahr T (7 September 2020). "COVID-19: MEPs want safe vaccines, full transparency and liability for companies". European Parliament. Ms. Gallina stressed negotiations with companies had been difficult but underlined that those companies developing and manufacturing COVID-19 vaccines would indeed be liable according to current laws and if something goes wrong they could be taken to court. This also goes for compensation for hidden defects. Archived from the original on 13 October 2021. Retrieved 29 December 2020.
- ↑ "Investigation: Drugmaker 'bullied' Latin American nations". Al Jazeera. 11 March 2021. Archived from the original on 31 October 2021. Retrieved 15 June 2021.
- ↑ Barcellos R (13 May 2021). "Carlos Murillo diz que cláusulas criticadas pelo Brasil valem em 110 países" [Carlos Murillo says critical clauses for Brazil are valid in 110 countries]. CNN Brasil (in Portuguese). Archived from the original on 28 June 2021. Retrieved 15 June 2021.
{{cite news}}: CS1 maint: unrecognized language (link) - ↑ "EXCLUSIVE Blackwater founder Prince takes role in COVID vaccine venture". Reuters. 4 June 2021. Archived from the original on 9 October 2021. Retrieved 4 June 2021.
- ↑ Lynas M (20 April 2020). "COVID: Top 10 current conspiracy theories". Alliance for Science. Archived from the original on 5 August 2020. Retrieved 4 October 2021.
- ↑ Burakovsky A (28 August 2021). "Russia's COVID-19 response slowed by population reluctant to take domestic vaccine". KRQE. Archived from the original on 21 September 2021. Retrieved 20 September 2021.
- ↑ "A Covid pass takes France by storm". WLFI News. Archived from the original on 20 September 2021. Retrieved 20 September 2021.
- ↑ "MLB offers free tickets for COVID-19 vaccinations". Kron4. 4 June 2021. Archived from the original on 9 October 2021. Retrieved 4 October 2021.
- ↑ Gore D (10 May 2021). "Exploring the legality of COVID-19 vaccine mandates". factcheck.org. Archived from the original on 10 October 2021. Retrieved 4 October 2021.
- ↑ Haas, Julia W.; Bender, Friederike L.; Ballou, Sarah; Kelley, John M.; Wilhelm, Marcel; Miller, Franklin G.; Rief, Winfried; Kaptchuk, Ted J. (18 January 2022). "Frequency of Adverse Events in the Placebo Arms of COVID-19 Vaccine Trials: A Systematic Review and Meta-analysis". JAMA Network Open. 5 (1): e2143955–e2143955. doi:10.1001/jamanetworkopen.2021.43955. ISSN 2574-3805. Archived from the original on 27 January 2022. Retrieved 28 January 2022.
- ↑ Haas, JW; Bender, FL; Ballou, S; Kelley, JM; Wilhelm, M; Miller, FG; Rief, W; Kaptchuk, TJ (4 January 2022). "Frequency of Adverse Events in the Placebo Arms of COVID-19 Vaccine Trials: A Systematic Review and Meta-analysis". JAMA network open. 5 (1): e2143955. doi:10.1001/jamanetworkopen.2021.43955. PMID 35040967.
- ↑ Smith, Ian (19 January 2022). "'Nocebo effect' cause of most COVID vaccine side effects, study says". euronews. Archived from the original on 24 January 2022. Retrieved 28 January 2022.
- ↑ 227.0 227.1 "COVID-19 vaccine tracker (Refresh URL to update)". vac-lshtm.shinyapps.io. London School of Hygiene & Tropical Medicine. 12 July 2021. Retrieved 10 March 2021.
- ↑ "Approved Vaccines". COVID 19 Vaccine Tracker, McGill University. 12 July 2021.
Further reading[edit | edit source]
- Krause PR, Fleming TR, Longini IM, Peto R, Briand S, Heymann DL, et al. (July 2021). "SARS-CoV-2 Variants and Vaccines". N Engl J Med. 385 (2): 179–186. doi:10.1056/NEJMsr2105280. PMC 8262623. PMID 34161052.
- Kyriakidis NC, López-Cortés A, González EV, Grimaldos AB, Prado EO (February 2021). "SARS-CoV-2 vaccines strategies: a comprehensive review of phase 3 candidates". NPJ Vaccines. 6 (1): 28. doi:10.1038/s41541-021-00292-w. PMC 7900244. PMID 33619260.
- Ramsay M, ed. (2020). "Chapter 14a: COVID-19". Immunisation against infectious disease. Public Health England. Archived from the original on 2019-11-12. Retrieved 2022-01-26.
- Development and Licensure of Vaccines to Prevent COVID-19: Guidance for Industry (PDF) (Report). U.S. Food and Drug Administration (FDA). June 2020. Archived from the original on 2021-04-16. Retrieved 2022-01-26.
Vaccine protocols[edit | edit source]
- "Protocol mRNA-1273-P301" (PDF). Moderna. Archived (PDF) from the original on 2020-09-28. Retrieved 2022-01-26.
- "Protocol C4591001 PF-07302048 (BNT162 RNA-Based COVID-19 Vaccines)" (PDF). Pfizer. Archived from the original (PDF) on 28 September 2020. Retrieved 21 September 2020.
- "Protocol AZD1222 – D8110C00001" (PDF). AstraZeneca. Archived (PDF) from the original on 2020-09-28. Retrieved 2022-01-26.
- "Protocol VAC31518COV3001; Phase 3 (Ensemble)" (PDF). Janssen Vaccines & Prevention. Archived from the original on 2021-02-02. Retrieved 2022-01-26.
- "Protocol VAC31518COV3009; Phase 3 (Ensemble 2)" (PDF). Janssen Vaccines & Prevention. Archived from the original on 2021-02-25. Retrieved 2022-01-26.
- "Protocol VAT00008 – Study of Monovalent and Bivalent Recombinant Protein Vaccines against COVID-19 in Adults 18 Years of Age and Older Protocol" (PDF). Sanofi Pasteur. Archived (PDF) from the original on 2021-07-23. Retrieved 2022-01-26.
External links[edit | edit source]
| Wikiquote has quotations related to: COVID-19 vaccine |
- "The different types of COVID-19 vaccines". World Health Organization (WHO). Archived from the original on 2021-02-16. Retrieved 2022-01-26.
- "COVID-19 vaccine tracker and landscape". World Health Organization (WHO). Archived from the original on 2020-10-11. Retrieved 2022-01-26.
- COVID‑19 Vaccine Tracker Archived 2020-03-23 at the Wayback Machine. Regulatory Affairs Professionals Society (RAPS)
- "STAT's Covid-19 Drugs and Vaccines Tracker". Stat. 27 April 2020. Archived from the original on 27 April 2020. Retrieved 26 January 2022.
- "COVID-19 vaccines: development, evaluation, approval and monitoring". European Medicines Agency (EMA). Archived from the original on 2021-02-26. Retrieved 2022-01-26.
- "Vaccine Development – 101". U.S. Food and Drug Administration (FDA). 27 August 2021. Archived from the original on 12 November 2021. Retrieved 26 January 2022.
- "Tracking Omicron and Other Coronavirus Variants". The New York Times. Archived from the original on 2021-11-30. Retrieved 2022-01-26.
- M.I.T. Lecture 10: Kizzmekia Corbett, Vaccines on YouTube
- M.I.T. Lecture 12: Dan Barouch, Covid-19 Vaccine Development on YouTube
- "COVID-19 vaccines: research and development". European Medicines Agency (EMA). Archived from the original on 2021-11-11. Retrieved 2022-01-26.
- "The 5 Stages of COVID-19 Vaccine Development: What You Need to Know About How a Clinical Trial Works". Johnson & Johnson. 23 September 2020. Archived from the original on 11 November 2021. Retrieved 26 January 2022.
- "How patent laws get in the way of the global coronavirus vaccine rollout". The Conversation. Archived from the original on 2021-11-14. Retrieved 2022-01-26.
- "A New Entry in the Race for a Coronavirus Vaccine: Hope". The New York Times. Archived from the original on 2020-05-20. Retrieved 2022-01-26.
- "Halting Progress and Happy Accidents: How mRNA Vaccines Were Made". The New York Times. Archived from the original on 2022-01-19. Retrieved 2022-01-26.
- "Coronavirus vaccine – weekly summary of Yellow Card reporting". Medicines and Healthcare products Regulatory Agency (MHRA). Archived from the original on 2021-05-20. Retrieved 2022-01-26.
- "Joint Statement from HHS Public Health and Medical Experts on COVID-19 Booster Shots". U.S. Centers for Disease Control and Prevention (CDC). 18 August 2021. Archived from the original on 10 November 2021. Retrieved 26 January 2022.
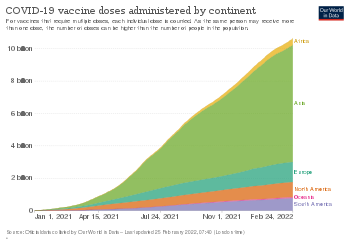
![Map showing share of population fully vaccinated against COVID-19 relative to a country's total population[note 1]](data/media/images/350px-World_map_of_share_of_people_who_received_all_doses_prescribed_by_the_initial_COVID-19_vaccination_protocol.png)


.jpg)

