.jpg)
During the COVID-19 pandemic, face masks, such as surgical masks and cloth masks, were employed as a public and personal health control measures against the spread of SARS-CoV-2. In community and healthcare settings, their use is intended as source control to limit transmission of the virus and also for personal protection to prevent infection.[1] Properly worn masks both limit the respiratory droplets and aerosols spread by infected individuals and help protect healthy individuals from infection.[2]
Masking has proven effective in reducing the transmission of COVID-19.[3][4][5][6] Masks vary in how well they work, with N95 and surgical masks outperforming cloth masks, which are more common due to supply shortages,[7] but even cloth masks, with their variability in fabric type and mask fit, provide wearers with substantial protection from particles carrying COVID-19.[8] Among readily available fabrics, double-layered cotton, hybrid masks, and cotton flannel perform best[8] and filtration effectiveness generally improves with thread count.[7] Healthcare workers, given their exposure, are recommended against using cloth masks.[8] Observational studies have shown evidence that masks reduce the community spread of COVID-19.[7] Randomized controlled population trials are uncommon due to ethical and logistical issues.[7] Clinical studies had not evaluated the efficacy of cloth masks in COVID-19 transmission by the end of 2021.[8] A number of observational studies, including four reviewed in a Lancet meta-analysis, have found that masks offer statistically significant protection from infection, although the level of protection varies according to the mask type and setting.[9]
Governments have widely recommended and mandated mask-wearing. According to the advocacy group Masks4All, 177 out of 198 national governments currently recommend using face masks. Prominent national and intergovernmental health agencies and their leaders have recommended the use of masks to reduce transmission, including the WHO, American, European and Chinese Centers for Disease Control and Prevention, and American immunologist and NIAID Director Anthony Fauci.[10]
Masks have been extensively adopted across the world. In March 2021, an estimated 129 billion face masks were used per month.[11]
Types of masks[edit | edit source]
| Part of a series on the |
| COVID-19 pandemic |
|---|
|
In the COVID-19 pandemic, governments recommend using face masks to avoid the transmission of COVID-19 from infected people to others. Masks with exhalation valves are not recommended because they expel the wearer's breath outwards, and an infected wearer would transmit the viruses through the valve. A second purpose of the face masks is to protect each wearer from environments that can infect them, which can be achieved by many models of masks.[12]
Between the different types of face masks that have been recommended throughout the COVID-19 pandemic, with higher or lower affectivity, it is possible to include:[citation needed]
- cloth face masks
- surgical masks (medical masks)
- certified face-covering masks, considered respirators, with certifications such as N95 and N99, and FFP
- filtering respirators with certifications such as N95 and N99, and FFP
- other respirators, including elastomeric respirators, some of which may also be considered filtering masks
There are some other types of personal protective equipment (PPE), as face shields and medical goggles, that are sometimes used in conjunction with face masks but are not recommended as a replacement.[13] Other kinds of PPE include gloves, aprons, gowns, shoe covers and hair covers.[14]
There have been shortages of masks, which has led to the use of uncertified masks, with a worse performance.[15]
Cloth masks[edit | edit source]
A cloth face mask is worn over the mouth and nose and made of common textiles such as cotton. Masks vary widely in effectiveness, depending on factors such as material, fit and seal, and number of layers. They are usually less effective at filtering than surgical masks and offer much less protection.[16][17] Unlike disposable masks, there are no required standards for cloth masks.[18]
One 2020 study found that a cloth mask was better than nothing, but not as good as a soft electret-filter surgical mask for protecting healthcare workers while simulating treatment of an artificially infected patient.[18] Research on commonly available fabrics used in cloth masks found that cloth masks can provide significant protection against the transmission of particles in the aerosol size range, with enhanced performance across the nanoscale and microscale when masks utilize both mechanical and electrostatic-based filtration, but that leakage due to improper fit can degrade performance.[19] A review of available research published in January 2021 concludes that cloth masks are not considered adequate to protect healthcare practitioners in a clinical setting.[20]
A 2013 study had volunteers wear masks they made themselves from cotton T-shirts, following the pattern of a standard tie behind the head surgical mask,[21] and found the number of microscopic particles that leaked to the inside of the homemade masks was twice that of commercial masks. Wearing homemade masks also leaked a median average of three times as many microorganisms as commercial masks. But another 2020 study found that masks made of at least two layers of T-shirt fabric could be as protective against virus droplets as medical masks, and as breathable.[22]

A 2020 peer-reviewed summary of published literature on the filtration properties of cloth and cloth masks recommends two to four layers of plain-weave cotton or flannel of at least 100 threads per inch.[24] There is a trade-off in that increasing the number of layers increases the filtration of the material but decreases how easy it is for a person to breath through the mask.
As of May 2020, there was no research on decontaminating and reusing cloth masks.[18] The CDC recommends removing a mask by handling only the ear loops or ties, placing it directly in a washing machine, and immediately washing hands in soap and water for at least twenty seconds. Cold water is considered as effective as warm water for decontamination.[25] The CDC also recommends washing hands before putting on the mask and again immediately after touching it.[26]
There is no information on reusing an interlayer filter. Disposing of filters after a single use may be desirable.[18] A narrative review of the literature on the filtration properties of cloth and other household materials did not find support for using a filter. A layer of cloth, if tolerated, was suggested instead,[24] or a PM2.5 filter, as a third layer.[27]
A United States Environmental Protection Agency (EPA) Study published on April 5, 2021, showed extremely varied performance across cotton masks. The results of the EPA study found that "a three-layer knitted cotton mask blocked an average of 26.5 percent of particles in the chamber, while a washed, two-layer woven nylon mask with a filter insert and metal nose bridge blocked 79 percent of particles on average."[28] Ultimately, the researchers found that fabric and fit are the two of the most vital factors when recommending masks to the public and further research is being conducted on variables such as facial hair and face shape on mask fit.[28]
Surgical masks[edit | edit source]

A surgical mask is a loose-fitting, disposable mask that creates a physical barrier separating the mouth and nose of the wearer from potential contaminants in the immediate environment. If worn properly, a surgical mask is meant to help block large-particle droplets, splashes, sprays, or splatter that may contain viruses and bacteria, keeping them from reaching the wearer's mouth and nose. Surgical masks may also help reduce exposure of others to the wearer's saliva and respiratory secretions.[29][30]
Certified medical masks are made of non-woven material, and they are mostly multi-layer. Filters may be made of microfibers with an electrostatic charge; that is, the fibers are electrets. An electret filter increases the chances that smaller particles will veer and hit a fiber, rather than going straight through (electrostatic capture).[31][32][33][better source needed][medical citation needed] While there is some development work on making electret filtering materials that can be washed and reused,[34] current commercially produced electret filters are ruined by many forms of disinfection, including washing with soap and water or alcohol, which destroys the electric charge.[35] During the COVID-19 pandemic, public health authorities issued guidelines on how to save, disinfect and reuse electret-filter masks without damaging the filtration efficiency.[35][36] Standard disposable surgical masks are not designed to be washed. Surgical masks may be labeled as surgical, isolation, dental, or medical procedure masks.[29] The material surgical masks are made from is much poorer at filtering very small particles (in range a tenth of a micrometer to a micrometer across) than that of filtering respirators (for example N95, FFP2) and the fit is much poorer.[29] Surgical masks are made of a non-woven fabric created using a melt blowing process.[37][38] Random control studies of respiratory infections like influenza find little difference in protection between surgical masks and respirators (such as N95 or FFP masks).[39] However, the filtering performance of correctly worn N95/FFP2 type filtering respirators is clearly superior to surgical and to cloth masks[17] and for influenza, work by the UK Health and Safety executive[40] found that live virus penetrated all surgical masks tested but properly fitted respirators reduced the viral dose by a factor of at least a hundred.
Surgical masks made to different standards in different parts of the world have different ranges of particles which they filter. For example, the People's Republic of China regulates two types of such masks: single-use medical masks (Chinese standard YY/T 0969) and surgical masks (YY 0469). The latter ones are required to filter bacteria-sized particles (BFE ≥ 95%) and some virus-sized particles (PFE ≥ 30%), while the former ones are required to only filter bacteria-sized particles.[41][42][43]
Modifications[edit | edit source]
The effectiveness of surgical masks in limiting particle transmission is a function of material and fit.[44] Since the start of the pandemic, scientists have evaluated various modifications to ear loop surgical masks aimed at improving mask efficacy by reducing or eliminating gaps between the mask and face.[45] The CDC evaluated and recommends two such modifications to ear loop masks to minimize the transmission of SARS-CoV-2. Under regular use, the CDC found that a surgical mask worn by a coughing individual blocked 41.3% of simulated cough aerosols (0.1–7.0 μm particle size) from reaching a second individual six feet away. However, by applying a knot and tuck technique,[lower-alpha 1] 62.9% of particles were blocked. When the surgical mask was covered with a larger cloth mask, 82% of particles were blocked. When both the source and recipient wore masks, 84% of particles were blocked. The number increased to more than 95% when both parties either wore double masks (surgical mask with larger cloth mask) or used the knot and tuck technique.[46]
Another type of modifications was aimed to improve the comfort of the wearers. Early on in the pandemic, healthcare workers were required to continue wearing surgical masks for 12 or more hours a day. This caused the ear loops of the masks to chafe the back of their ears. Ear savers, plastic straps and hooks that go around wearer's heads, were invented to move the ear loops away from the wearer's ears. They could be made on demand by using 3D printing process.[47]
Filtering respirators[edit | edit source]
An N95 mask is a particulate-filtering facepiece respirator that meets the N95 air filtration rating of the US National Institute for Occupational Safety and Health, meaning it filters at least 95 percent of airborne particles, while not resistant to oil like the P95. It is the most common particulate-filtering facepiece respirator.[48] It is an example of a mechanical filter respirator, which provides protection against particulates, but not gases or vapors.[49] Like the middle layer of[50] surgical masks, the N95 mask is made of four layers[18] of melt-blown nonwoven polypropylene fabric.[51][52][unreliable medical source?] The corresponding face mask used in the European Union is the FFP2 respirator.[53][54]
Hard electret-filter masks like N95 and FFP masks must fit the face to provide full protection. Untrained users often get a reasonable fit, but fewer than one in four gets a perfect fit. Fit testing is thus standard. A line of petroleum jelly on the edge of the mask[55] has been shown to reduce edge leakage[18] in lab tests using mannequins that simulate breathing.[55]
Some N95 series respirators, especially those intended for industrial use, have an exhalation valve to improve comfort, making exhalation easier and reducing leakage on exhalation and steaming-up of glasses. But those respirators are not reliable for the control of infected people (source control) in respiratory diseases such as COVID-19, because infected users (asymptomatic or not) would transmit the virus to others through the valve.[56]
During the COVID-19 pandemic, there were shortages of filtering facepiece respirators, and they had to be used for extended periods, and/or disinfected and reused. At the time, public health authorities issued guidelines on how to save, disinfect and reuse masks, as some disinfection methods damaged their filtration efficiency.[35][36] Some hospitals stockpiled used masks as a precaution,[57] and some had to sanitize and reuse masks.
Face shields and eye protection[edit | edit source]

The US Centers for Disease Control and Prevention (CDC) does not recommend the use of face shields as a substitute for masks to help slow the spread of COVID-19.[58] In a study by Lindsley et al. (7 January 2021) funded by the National Institute for Occupational Safety and Health, part of the CDC, face shields were found to block very few cough aerosols in contrast to face coverings – such as cloth masks, procedure masks, and N95 respirators – indicating that face shields are not effective as source control devices for small respiratory aerosols and that face coverings are more effective than face shields as source control devices to reduce the community transmission of SARS-CoV-2.[59]
In a scoping review, Godoy et al. (5 May 2020) said face shields are used for barrier protection against splash and splatter contamination, but should not be used as primary protection against respiratory disease transmission due to the lack of a peripheral seal rather than as an adjunct to other facial protection.[18] They remarked that face shields have been used like this alongside medical-grade masks during the COVID-19 pandemic.[18] They cited a cough simulation study by Lindsley et al. (2014) in which face shields were shown to reduce the risk of inhalation exposure up to 95% immediately following aerosol production, but the protection was decreased with smaller aerosol particles and persistent airborne particles around the sides.[60]
There is weak evidence that the use of eye protection including face shields is associated with less infection.[9]
Elastomeric respirators[edit | edit source]

Elastomeric respirators are reusable personal protective equipment comprising a tight-fitting half-facepiece or full-facepiece respirator with exchangeable filters such as cartridge filters.[61] They provide an alternative respiratory protection option to filtering facepiece respirators such as N95 masks. Some healthcare workers have used them during times of short supply caused by the pandemic, as they can be reused over an extended period in healthcare settings.[61][62] However, most elastomeric respirators have an unfiltered exhalation vent which would allow the virus to spread from the wearer.[62]
For the COVID-19 response when supplies are short, the US CDC says contingency and crisis strategies should be followed: Each elastomeric respirator is issued for the exclusive use of an individual healthcare provider but must be cleaned and disinfected as often as necessary to remain unspoiled and sanitary. If there is no other option than to share a respirator between healthcare providers, the respirator must be cleaned and disinfected before it is worn by a different individual. Filters (except for unprotected disc types) may be used for an extended period, but the filter housing of cartridge types must be disinfected after each patient interaction.[61]
Powered air-purifying respirators[edit | edit source]
A powered air-purifying respirator (PAPR) is a personal protective equipment in which a device with a filter and fan creates a highly filtered airflow towards the headpiece and a positive outflow of air from the headpiece.[63]
There is an increased risk for healthcare workers to become exposed to SARS-CoV-2 when they conduct aerosol-generating procedures on COVID-19 patients, which is why it is argued that such situations may require enhanced personal protective equipment (i.e., higher than N95) such as PAPRs for healthcare workers.[63][64]
In a systematic review, Licina, Silvers, and Stuart (8 August 2020) said field studies indicate that there was equivalent rates of infection between healthcare workers, who performed airway procedures on critical COVID-19 patients, utilizing PAPRs or other appropriate respiratory equipment (such as N95 or FFP2), but remarked that there is a need to further collect field data about optimal respiratory protection during highly virulent pandemics.[65]
Face masks with exhalation valves[edit | edit source]
Some masks include an exhalation valve to expel the breath outwards, but that current of air is not filtered. Certification (as N95 or FFP2) is about the mask itself and does not warrant any safety about the air that is exhaled. Putting tape over the exhalation valve can make a mask or respirator as effective as one without a valve.[67]
Scientists have visualized droplet dispersal for masks with exhalation valves and face shields, and concluded that they can be ineffective against COVID-19 spread (e.g., after a cough) and recommended alternatives.[68][69]
Recommendations[edit | edit source]
The use of face masks or coverings by the general public has been recommended by health officials to minimize the risk of transmissions, with authorities either requiring their use in certain settings, such as on public transport and in shops, or universally in public.
Health officials had advised that medical-grade face masks, such as respirators, should be prioritized for use by healthcare workers in view of critical shortages, so they used to generally first and foremost recommend cloth masks for the general public.[70][71] However, recommendations have changed as the body of scientific knowledge evolved.[72] Scientists now recommend having a triple-layered surgical mask and a respirator.[73]
According to #Masks4All, about 95% of the world population lives in countries where the government and leading disease experts recommend or require the use of masks in public places to limit the spread of COVID-19.[74]
World Health Organization[edit | edit source]
Early in 2020, the WHO had only recommended medical masks for people with suspected infection and respiratory symptoms, their caregivers and those sharing living space, and healthcare workers.[75][76][77] In April 2020, the WHO acknowledged that wearing a medical mask can limit the spread of certain respiratory viral diseases including COVID-19, but claimed that medical masks would create a false sense of security and neglect of other necessary measures, such as hand hygiene.[77]
The early WHO advice on limited mask usage was scrutinized for several reasons. First, experts and researchers pointed out the asymptomatic transmission of the virus.[78][79][80][81][82] Second, according to Marteau et al. (27 July 2020), available evidence does not support the notion that masking adversely affects hand hygiene:[83] Dame Theresa Marteau, one of the researchers, remarked that "The concept of risk compensation, rather than risk compensation itself, seems the greater threat to public health through delaying potentially effective interventions that can help prevent the spread of disease."[84]
The WHO revised its mask guidance in June 2020, with its officials acknowledging that studies indicated asymptomatic or pre-symptomatic spread.[85] The updated advice recommended that the general public should wear non-medical fabric masks where there is known or suspected widespread transmission and where physical distancing is not possible, and that vulnerable people (60 and over, or with underlying health risks) and people with any symptoms suggestive of COVID-19 as well as caregivers and healthcare workers should wear surgical or procedure masks.[71] They stated that the purpose of mask usage is to prevent the wearer transmitting the virus to others (source control) and to offer protection to healthy wearers against infection (prevention).[71]
The WHO advises that non-medical fabric masks should comprise a minimum of three layers,[71] suggesting an inner layer made of absorbent material (such as cotton), a middle layer made of non-woven material (such as polypropylene) which may enhance filtration or retain droplets, and an outer layer made of non-absorbent material (such as polyester or its blends) which may limit external contamination from penetration.[86]
On 21 August 2020, the WHO and UNICEF released an annex guidance for children.[87] For children five and younger, they advise that masks should not be required in consideration to a child's developmental milestones, compliance challenges, and autonomy required to use a mask properly, but recognized that the evidence supporting their cut-off age is limited and countries may hold a different and lower age of cut-off.[87] For children 6–11, they advise that mask usage should be decided in consideration of several factors including the intensity of local viral transmission, (the latest evidence about) the risk of infection for the age group, the social and cultural environment (which influences social interactions in communities and populations), the capacity to comply with appropriate mask usage, the availability of appropriate adult supervision, and the potential impact on learning and psychosocial development, as well as additional factors involving specific settings or circumstances (such as disabilities, underlying diseases, elderly people, sport activities, and schools).[87] For children 12 and older, they advise that masks should be worn under the same conditions for adults in accordance to WHO guidance or national guidelines.[87]
Regarding the use of non-medical fabric masks in the general population, the WHO has stated that high-quality evidence for its widespread use is limited, but advises governments to encourage its use as physical distancing may not be possible in some settings, there is some evidence for asymptomatic transmission, and masks could be helpful to provide a barrier to limit the spread of potentially infectious droplets.[88]
United States Centers for Disease Control and Prevention[edit | edit source]

Early in 2020, the United States Centers for Disease Control and Prevention (CDC) said it did not recommend the use of face masks for the general public.[90][91] However, on 3 April 2020, the CDC changed its advice to recommend that people wear cloth face coverings "in public settings when around people outside their household, especially when social distancing measures are difficult to maintain".[92][93] In response to a media inquiry by National Public Radio, the CDC said that this change in guidelines was due to the increasing and widespread transmission of the virus, citing studies published in February and March showing pre-symptomatic and asymptomatic transmission.[94] In a subsequent interview and JAMA editorial, the CDC director Robert R. Redfield explained that the CDC's early guidance had been premised on an initial absence of evidence of disease transmission from pre- and asymptomatic individuals.[95][96][97]

Since 28 June, the "CDC recommends that people wear cloth face coverings in public settings and when around people who don't live in your household, especially when other social distancing measures are difficult to maintain. Cloth face coverings may help prevent people who have COVID-19 from spreading the virus to others. Cloth face coverings are most likely to reduce the spread of COVID-19 when they are widely used by people in public settings."[99] The CDC provides the caveat that cloth face coverings should not be worn by children under the age of two, people who have trouble breathing, or people who are unconscious, incapacitated, or otherwise unable to remove the mask without assistance.[99] In August 2020, the CDC added that exhalation valves or vents in masks do not help prevent the person wearing the mask from spreading COVID-19 to others.[58][100]
In a November 2020 scientific brief, the CDC reiterated their recommendation for the community use of masks and specifically non-valved multi-layer cloth masks to prevent transmission of SARS-CoV-2.[101] They say the community's use of masks serves two primary purposes: to reduce the emission of virus-laden droplets from exhalation into the environment (source control), which is especially relevant for asymptomatic or pre-symptomatic infected wearers who feel well and may be unaware of their infectiousness to others, and to reduce inhalation of these droplets through filtration for the wearer (personal protection).[101] For filtration, the CDC says some fabrics (such as silk) may hydrophobically repel moist droplets, whereas other fabrics (such as polyester or polypropylene) may electrostatically capture droplets.[101] They concluded that the benefit of masking for SARS-CoV-2 control is derived from the combination of source control and personal protection, which is likely complementary and possibly synergistic, so that individual benefit increases with increasing community mask use.[101]
The CDC said healthcare personnel should wear a NIOSH-approved N95 (or equivalent or higher-level) respirator or a face mask (if a respirator is not available) with a face shield or goggles as part of their personal protective equipment, while patients with suspected or confirmed SARS-CoV-2 infection should wear a face mask or cloth face covering during transport.[102] As crisis strategy for known shortages of N95 respirators in healthcare settings, among other sequential measures, the CDC suggests use of respirators beyond the manufacturer-designated shelf life, use of respirators approved under standards used in other countries that are similar to NIOSH-approved respirators, limited re-use of respirators, use of additional respirators beyond the manufacturer-designated shelf life that have not been evaluated by NIOSH, and prioritizing the use of respirators and face masks by activity type.[103]
In late July 2021, the CDC changed guidelines to recommend people, including those who are vaccinated, to continue masking in public indoor settings in areas with substantial and high transmission—as there are indications that the coronavirus such as the Delta variant may infect even vaccinated people in rare occasions—to help prevent transmission to other people.[104][105] Previously, the CDC updated public guidance from May 2021 stated that those who are fully vaccinated can "resume activities without wearing masks or physically distancing, except where required by federal, state, local, tribal, or territorial laws, rules and regulations, including local business and workplace guidance."[106] However, critics posited that it was predicated on a key social factor, namely whether people can be trusted to wear a mask if they are not fully vaccinated.[107][108][109]
On February 25, 2022, the CDC changed their guidelines to suggest that 70% of Americans need no longer wear masks, and no longer need to social distance or avoid crowded spaces.[110] Under the new guidance, Americans in counties designated as medium-to-low-risk can go indoors without masks. In accordance with these new CDC guidelines, a number of US states ended their mask mandates for indoor spaces. However, federal officials emphasized that regardless of local conditions, individuals with COVID-19 or COVID-19 symptoms, as well as individuals who consider themselves to be high-risk, should continue to wear facial coverings. In addition to this, the CDC also dropped its recommendation for universal school mask mandates.[111] These new recommendations assessed COVID-19 hospitalizations as well as the proportion of beds occupied by COVID-19 patients in certain areas.
Criticism of guidance[edit | edit source]
Larry Gostin, a professor of public health law, said initial CDC and WHO guidance had given the public the wrong impression that masks do not work, even though scientific evidence to the contrary was already available.[94] The confusing changing advice from discouraging to recommending public masking has led to decreasing public trust in the CDC.[80][112] In June 2020 Anthony Fauci, a leading infectious disease expert for the United States government, stated that the delay in recommending general mask use was motivated by a desire to conserve dwindling supplies for medical professionals.[113]
China and Asia[edit | edit source]
In March 2020, when asked about the mistakes that other countries were making in the pandemic, the Chinese Center for Disease Control and Prevention director-general George Fu Gao said:
"The big mistake in the U.S. and Europe, in my opinion, is that people aren't wearing masks. This virus is transmitted by droplets and close contact. Droplets play a very important role – you've got to wear a mask, because when you speak, there are always droplets coming out of your mouth. Many people have asymptomatic or pre-symptomatic infections. If they are wearing face masks, it can prevent droplets that carry the virus from escaping and infecting others."[114]
Europe[edit | edit source]
Most countries in Europe have introduced mandatory face mask rules for public places.[115][116] On 8 April 2020, the European Centre for Disease Prevention and Control (ECDC) published its masking recommendations, saying that the "use of face masks in the community could be considered, especially when visiting busy, closed spaces".[117][70] On 15 February 2021, ECDC updated the recommendation stating "Although the evidence for the use of medical face masks in the community to prevent COVID-19 is limited, face masks should be considered as a non-pharmaceutical intervention in combination with other measures as part of efforts to control the COVID-19 pandemic."[118]
The Nordic countries and the Netherlands have been a notable exception to supporting the use of face masks,[116][119] but eventually started to recommend masks. For example, due to the COVID-19 pandemic in the Netherlands, wearing a mouth/nose mask was made mandatory on public transportation per 1 June 2020.[120] The main reasoning against masks recommendations given by officials in the Nordic countries was that public masking is deemed an unnecessary precaution when infection levels remain low.[121] In June 2020, the Norwegian Institute of Public Health said asymptomatic individuals wearing face masks was not to be recommended due to the low prevalence of COVID-19 in the country, but noted that it should be reconsidered if cases rise.[122] Similarly, on 30 July 2020, the Danish Health Authority director Søren Brostrøm said face covers did not make sense in the current situation with low infection levels, but that they needed to evaluate whether it could make sense in the long term.[123][124] From 29 October, face masks are mandatory inside in any building in Denmark that has public access – from supermarkets and kiosks to hospitals and schools.[125] In many Norwegian local municipalities, face masks are mandatory on public transport where a social distance of one metre is impossible to maintain.[126]
Sweden in particular stands out as a country where face masks have not been recommended to the general public and the State Epidemiologist of Sweden, Anders Tegnell, has been an opponent to face masks among the general population, although he has said that face masks might be suitable on work places where people are one to two meter from each other's for more than fifteen minutes, something which some Swedish and foreign media have interpreted as a recommendation.[127][128] This position was slightly reversed when Prime Minister of Sweden, Stefan Löfven, announced that they were recommending face masks on 18 December 2020.[129] The Public Health Agency of Sweden later clarified on their website that the recommendation would include citizens born before 2004 to wear masks during rush hour on public transportation throughout the country from 7 January 2021 onward.[130] On 20 December 2020, two days after the announcement was made, Prime Minister Löfven was paparazzied in a shopping mall in central Stockholm without wearing a face mask.[131] By 22 January 2021 the Stockholm Public Transport estimated that about half of all passengers on trains and busses wore face masks during rush hour.[132] Among those who chose not to follow the recommendation were Johan Carlson, the Director-General of the Public Health Agency, and Anders Tegnell, the state epidemiologist.[133][134]
Rationale for wearing masks[edit | edit source]
Masks are used to limit the transmission of SARS-CoV-2 by respiratory droplets and aerosols, which are thought to be the major pathways of infection, exhaled from infected individuals during breathing, speaking, coughing, and sneezing.[1][136][137] Properly worn masks are effective in both limiting the spread of the virus by an infected individual and protecting an uninfected individual from infection.[2]
The National Health Commission of China cited the following reasons for the wearing of masks by the public, including healthy individuals:
- Asymptomatic transmission. Many people can be infected without symptoms or only with mild symptoms.[138]
- Difficulty or impossibility of appropriate social distancing in many public places at all times.[138]
- Cost-benefit mismatch. If only infected individuals wear masks, they would possibly have a negative incentive to do so. An infected individual might get nothing positive, but only bear the costs such as inconvenience, purchasing expenses, and even prejudice.[138]
- There is no shortage of masks in China. The country has the production capacity to meet the demand on masks.[138]
In a comment to The Lancet, Kar Keung Cheng, Tai Hing Lam, and Chi Chiu Leung argued that a public health rationale for mass masking is source control to protect others from respiratory droplets and underscored the importance of this approach due to asymptomatic transmission.[139] Wang Linfa, an infectious disease expert who heads a joint Duke University and National University of Singapore research team, said masking is about "preventing the spread of disease rather than preventing getting the disease", remarking that the point is to cover the faces of people who are infected but do not know it, so it is imperative for everyone to wear one in public.[79] The US CDC also highlighted the use of masks for source control, pointing out that asymptomatic and pre-symptomatic cases are estimated to account for over 50% of the transmissions.[140]
Yuen Kwok-yung, a microbiologist from the University of Hong Kong, states a high amount of virus strands in saliva of infected people and transmission by asymptomatic carriers as the reasons why even seemingly healthy individuals should wear a mask.[141] Kelvin Kai-Wang To et al. (February 2020) detected live SARS-CoV-2 in the saliva of infected patients, which indicated that the virus may be transmitted directly or indirectly through saliva with or without respiratory symptoms, and stated that the findings reinforced the use of surgical masks as a control measure.[142]
Monica Gandhi, a medical professor at the University of California, San Francisco, says viral shedding at high quantities from the upper respiratory tract, characterized by unusually high levels of viral particles, means universal mask wearing is one of the best ways to limit the asymptomatic spread of the virus.[143] Yixuan Hou et al. (July 2020) found that the nasal cavity is seemingly the dominant initial site for SARS-CoV-2 infection with subsequent aspiration-mediated virus seeding into the lungs; the authors note that these findings argue for the widespread use of masks to prevent exposure to the nasal passages.[144]
In a perspective, Monica Gandhi, Chris Beyrer, and Eric Goosby posit that masking reduces the dose of the virus for the wearer and thus helps lower the severity of infection.[145] They highlighted that the proportion of asymptomatic and mild infection increased in settings adopting population-level masking.[145] One example involved a comparison of outbreaks on cruise ships: the Diamond Princess had 18% asymptomatic cases among all the infected people, but this was 81% in the Greg Mortimer where masks were given to passengers and staff members.[145]
Trisha Greenhalgh et al. argue for the precautionary principle as a reason to adopt policies encouraging the wearing of face masks in public, given that there's much to gain and little to lose from adopting masks considering the seriousness of the outbreak.[146] Others agreed, based on the evidence-based principle that the likely benefits outweighed the likely harms.[147][148]
Leonardo Setti et al. argue that face masks should be used to complement social distancing of six feet or two meters, because this inter-personal distance is more effective if people are masked as studies indicate that SARS-CoV-2 could be transmitted over greater distances.[149] Chi Chiu Leung et al. also argue that face masks complement social distancing, as a high degree of compliance for distancing is necessary to achieve the greatest impact but is not always achievable.[150] For instance, even if social distancing is rigorously practiced, there are necessary person-to-person contacts (such as going to the supermarket and other necessary activities to sustain livelihoods), so masks would help in situations when social distancing is not feasible and maximize the effect of social distancing.[150]
According to Stephen Griffin, a virologist at the University of Leeds, "Wearing a mask can reduce the propensity for people to touch their faces, which is a major source of infection without proper hand hygiene."[151] Ka Hung Chan and Kwok-Yung Yuen argue that face masks can reduce fomite transmission (in addition to transmission through droplets or aerosol) of the virus, as masks can prevent people from spreading body fluids by touching their noses or mouths (such as trying to cover up a sneeze or cough).[152]
A paper by Miyu Moriyama et al. (September 2020), which links seasonality of respiratory viral diseases to decreased air humidity due to indoor heating, argues that mask wearing helps limiting respiratory virus transmission in winter, because masks keep the nose warm and moist.[153]
Social media claims that masks could reduce the oxygen levels in older people were refuted by a small study of SpO2 levels, the results of which were published by JAMA.[154]
Efficacy[edit | edit source]
A systemic review and meta-analysis of the effectiveness of masks published in the BMJ in November 2021 showed that with 95% confidence, masks reduced COVID incidence by between 25% and 71%. This result is based on six primary studies. These studies were of several different types: case control studies in Thailand and three Western countries (where cases identified whether they were wearing a mask when they had contact with a known positive patient), a randomised control study in Denmark which assessed the impact on mask wearing on the wearer, a natural experiment that compared US states that implemented mask mandates on the level of COVID, a cross sectional comparative study in China which surveyed whether a mask protected the wearer, and a retrospective cohort study in China which assessed the impact of masks worn by infected and uninfected family members. Another five studies were not included because they were not directly comparable. They assessed the impact of mask mandates across countries on mortality (finding a 45.7% reduction), of mask mandates in the US on R (finding a 29% reduction), a comparative incidence of COVID associated with mask wearing comparing HK and South Korea (finding a significant reduction), a natural experiment across US states finding a significant effect on case rates, and a cross sectional study assessing a 10% increase in mask wearing led to a 71% reduction in the risk to others. A lot of other papers had to be rejected because of a risk of confounding.[3]
There is consistent evidence that mask wearing is effective in reducing the spread of the SARS-CoV-2 virus.[155] Population-wide masking has proven significant in reducing the transmission of COVID-19.[7] Masks, however, are not of equal efficacy. While N95 masks outperform surgical masks in filtration, healthcare worker population studies have not shown a significant difference between the two, as of June 2021.[7] N95 and surgical masks, both designed for single-use, can be decontaminated at a loss to mask integrity and filtration efficacy.[7] Both N95 and surgical outperform cloth masks, which the general public has used based on its greater availability during mask supply shortages.[7] Cloth and fabric masks have protected wearers from COVID-19, with some variability,[8] such as fabric type, layer count, and mask fit.[156] Cloth masks are insufficient for healthcare workers and not recommended, according to two randomly controlled trials.[8]
Observational studies have shown evidence that masks reduce the community spread of COVID-19.[7] Randomized controlled population trials are uncommon due to ethical and logistical issues.[7] Clinical evidence of mask efficacy in COVID-19 transmission was limited and had become a subject of scientific debate by May 2021.[157] Clinical studies had not evaluated the efficacy of cloth masks in COVID-19 transmission by the end of 2021.[8] Evaluation of cloth mask efficacy is further complicated by the wide variation in fabric and fit, among other factors.[7] Concerning the precedent of mask efficacy in limiting transmission of respiratory viral illnesses other than COVID, a clinical trial meta-analysis in May 2021 showed no significant evidence of efficacy, though the authors noted the evidence to be of poor quality and subject to confounding factors like adherence to consistent mask usage.[157]
Community studies have shown some cloth masks to be effective at filtering respiratory droplets, which can carry SARS-CoV-2.[7] Cloth masks of cotton quilt (120 thread per inch), bonded copy paper, flannel, and chiffon or silk hybrid with cotton are over 90% effective at blocking particles the size droplets that carry SARS-CoV-2, according to an October 2021 review of 42 studies. Multilayered fabrics provided improved breathability and filtration efficacy. Among readily available fabrics, two-layered 100% cotton, two-layered cotton quilt, hybrid masks, and cotton flannel performed best.[8] Filtration effectiveness generally improves with thread count.[7]
The use of a face mask can result in a large risk reduction of infection with epidemic-causative beta coronaviruses. N95 or similar respirators account for a larger risk reduction than disposable surgical or other similar masks.[9] Masks are protective for both healthcare workers and people in communities exposed to infection; evidence supports masking in both healthcare and non-healthcare settings, with no striking differences detected in the effectiveness of masks between the settings.[9]
The CDC highlighted a number of studies in their 10 November 2020 scientific brief detailing the benefits of community masking.[140] In a study of 124 Beijing households with at least one laboratory-confirmed case of SARS-CoV-2 infection, mask use by the index patient and family contacts before the index patient developed symptoms reduced secondary transmission within the households by 79%.[158] A retrospective case-control study from Thailand documented that, among more than 1,000 people interviewed as part of contact tracing investigations, those who reported having always worn a mask during high-risk exposures experienced a greater than 70% reduced risk of acquiring infection compared with people who did not wear masks under these circumstances.[159] A similar study in three Western countries also came up with a 70% risk reduction.[160] A case study from July 2020 detailed that 139 clients exposed to two symptomatic hair stylists with confirmed COVID-19 (both the clients and the stylists wore face coverings) resulted in no symptomatic cases reported among all clients and no positive tests among the 67 people who volunteered to be tested.[161] A study of an outbreak aboard the USS Theodore Roosevelt, an environment notable for congregate living quarters and close working environments, found that use of face coverings on-board was associated with a 70% reduced risk.[162] Investigations involving infected passengers aboard flights longer than ten hours strongly suggest that masking prevented in-flight transmissions, as demonstrated by the absence of infection developing in other passengers and crew in the 14 days following exposure.[163] In addition, the CDC said the benefit of universal masking, including reductions in infections and mortality, has been demonstrated in community-level analyses by a set of studies involving the Massachusetts hospital system, the German city Jena, the American state Arizona, a panel of 15 American states and Washington, D.C., Canada nationally, and the United States nationally.[140]
In addition to studying the impact of mask wearing on transmission in a community, direct studies can be done on whether or not a mask filters out virus-carrying particles from the air. In August 2021, a study of the fabric of masks worn in the community found that they filtered out between half and three-quarters of the viral RNA.[164] Respirators made to a standard such as N95 or FFP2 when properly fitted should filter out at least 95% of the virus.
In December 2021, a study in PNAS found that when two people wear surgical masks, while the infectious is speaking, the risk of infection remains below 30% after one hour, but when both wear a well-fitting FFP2 mask, it is 0.4%.[165]
In February 2022, a study by the Centers for Disease Control and Prevention (CDC) found that surgical masks worn at indoor public venues can reduce the chances of testing positive for COVID-19 by 66%, while tightfitting N95 and KN95 masks can reduce the odds of infection by 83%.[166][167]
Optimal face mask designs and use[edit | edit source]
A scientific review of research about the overall efficacy of face masks in terms of product design (such as thermal comfort and flow resistance) and ways of usage found that fluid dynamics and fabrication techniques have a significant impact on performance. According to the review, studies showed that cotton and surgical masks had a microorganism filtration efficiency of 86.4% and 99.9% respectively, while the surgical mask was three times more effective in blocking transmission than the cotton mask and could lead to a decrease of the effective reproduction number to below 1 – which could halt epidemic spread in a region where 70% of residents use them consistently in public.[168][169]
By January 2021 several lines of research recommended double-masking (wearing a cloth mask over a surgical mask, along with using a mask filter, or wearing a nylon covering over a mask) as being efficacious.[170]
Correct handling and wearing of masks[edit | edit source]
As masking became widespread during the pandemic, it gave rise to the issue that many individuals of the public are not correctly handling and wearing their masks.[172][173][174] Suzanne Willard, a clinical professor at Rutgers School of Nursing, remarked that the general public is not used to wearing masks and lay people are asked to use a tool health care professionals are trained to use.[175]
A commonly-seen issue is that people are wearing masks pulled down below the nose, which is an incorrect way to wear a mask.[176][177] Zane Saul, the chief of infectious disease at Bridgeport Hospital, remarked that "I really have observed people not covering their noses and just covering their mouths. It's just as important to cover your nose."[176] Daniel Gottschall, the vice president of medical affairs for the Fairfield region of Hartford HealthCare and St. Vincent's Medical Center in Bridgeport, explained that "By wearing a mask you're keeping a lot of those secretions inside of you. If you wear it just over your nose or just over your mouth and you're not diligent (about keeping it in place), you're exposing the secretions that come out of that part of the body to other people."[176]
Zeynep Tufekci, a professor of information science, remarked that messaging on masking should have been used to provide proper instructions to the public (as was done for hand washing) rather than used to discourage people from masking because of the possibility that they would wear them improperly, as had happened early in the pandemic.[80] The European Centre for Disease Prevention and Control highlighted that appropriate use of face masks in communities could be improved through education campaigns and is key for its effectiveness as a measure.[70] Health institutions such as the World Health Organization have provided public guidance on the do's and don'ts on masking.[23]
Shortages of face masks[edit | edit source]
Early epidemic in mainland China[edit | edit source]
As the epidemic accelerated, the mainland market in China saw a shortage of face masks due to increased public demand.[178] Face masks were quickly sold out in stores throughout China.[179] Hoarding and price gouging drove up prices, so the market regulator said it would crack down on such acts.[180][181] In January 2020, price controls were imposed on all face masks on Taobao and Tmall.[182] Other Chinese e-commerce platforms – JD.com,[183] Suning.com,[184] Pinduoduo[185] – did likewise; third-party vendors would be subject to price caps, with violators subject to sanctions.[citation needed]
By March, China had quadrupled its production capacity to a hundred million masks per day.[138]
National stocks and shortages[edit | edit source]
At the beginning of the COVID-19 outbreak in the United States, the U.S.'s Strategic National Stockpile contained just twelve million N95 respirators, far fewer than estimates of the amount required.[186] Millions of N95s and other supplies were purchased from 2005 to 2007 using congressional supplemental funding, but 85 million N95s were distributed to combat the 2009 swine flu pandemic, and Congress did not make the necessary appropriations to replenish stocks.[186] The Stockpile's primary focus has also primarily been on biodefense (defense against a terrorist or weapon of mass destruction attack) and response to natural disaster, with infectious disease a secondary focus.[186] By 1 April 2020, the Stockpile was nearly emptied of protective gear.[187] In January and February 2020, U.S. manufacturers, with the encouragement of the Trump administration, shipped millions of face masks and other personal protective equipment to the PRC, a decision that subsequently prompted criticism given the mask shortage that the U.S. faced during the pandemic.[188]
In France, 2009 H1N1-related spending rose to €382 million, mainly on supplies and vaccines, which was later criticized.[189][190] It was decided in 2011 to not replenish its stocks and rely more on supply from China and just-in-time logistics.[189] In 2010, its stock included a billion surgical masks and 600 million FFP2 masks; in early 2020, it was 150 million and zero respectively.[189] While stocks were progressively reduced, a 2013 rationale stated the aim to reduce costs of acquisition and storage, now distributing this effort to all private enterprises as an optional best practice to ensure their workers' protection.[189] This was especially relevant to FFP2 masks, more costly to acquire and store.[189][191] As the COVID-19 pandemic in France took an increasing toll on medical supplies, masks and PPE supplies ran low, causing national outrage. France needs forty million masks per week, according to French president Emmanuel Macron.[192] France instructed its few remaining mask-producing factories to work 24/7 shifts, and to ramp up national production to forty million masks per month.[192] French lawmakers opened an inquiry on the past management of these strategic stocks.[193] The mask shortage has been called a "scandal d'État" (State scandal).[194] Thousands of French individuals and companies teamed up during the outbreak to form a decentralized network of Fab labs and ad-hoc retooled production facilities, producing more than a million face shields, masks and other kinds of PPE during the height of the pandemic.[195]
In late March and early April 2020, as Western countries were in turn dependent on China for supplies of masks and other equipment, China was seen as making soft-power play to influence world opinion.[196][197] However, a batch of masks purchased by the Netherlands was reportedly rejected as being sub-standard. The Dutch health ministry issued a recall of 600,000 face masks from a Chinese supplier on 21 March which did not fit properly and whose filters did not work as intended despite them having a quality certificate.[196][197] The Chinese Ministry of Foreign Affairs responded that the customer should "double-check the instructions to make sure that you ordered, paid for and distributed the right ones. Do not use non-surgical masks for surgical purposes."[197] Eight million of eleven million masks delivered to Canada in May also failed to meet standards.[198][199]
Theft[edit | edit source]
Thefts of face masks and other personal protective equipment have been reported at hospitals in the United States and other countries.[200] The Naval Medical Center San Diego began mandatory random bag checks for staff members, after several incidents of theft.[201] Hospitals in Canada reported that theft of PPE had become so commonplace that face masks had to be locked away. According to hospital staff, the policy of locking up PPE often resulted in staff requests for PPE being denied.[202] Thefts of N95 masks were reported from a locked hospital office in South Carolina and off loading docks at the University of Washington.[203]
Two thousand surgical masks were stolen from a hospital in Marseille, France during the early months of the COVID-19 outbreak, in March. The masks were stolen from an area of the hospital that could only be accessed by surgery patients and staff.[204] A hospital employee in Cooperstown, New York was charged with misdemeanor larceny for a similar incident.[205] Hospital employees in West Java, Indonesia were arrested for stealing hundreds of boxes of face masks and selling them on the black market.[206]
One month later an Indiana hospital pharmacy reported a theft to the Drug Enforcement Administration. Along with morphine, with a street value estimated at $3000, the thieves, one of whom was an employee of the hospital and had an access card, had stolen masks and other in-demand goods. In the criminal complaint, filed in Indiana federal court, a DEA task force officer said:[200]
"Based on my training and experience, I know these items are highly sought after in the secondary market due to shortages resulting from the Coronavirus pandemic and that these types of items are being sold on the secondary market at an increased price well over fair market value."
A former hospital employee in Georgia was arrested on allegations of stealing masks and gloves from the hospital on five separate occasions after he was fired.[207] Also in April, an employee of the Charlie Norwood VA Medical Center was charged with a misdemeanor for stealing disposable gowns and surgical masks from the hospital.[208] PPE, including masks, were reported stolen by a member of the housekeeping staff at a hospital in Arizona and a physician's assistant in Florida.[209][210]
According to a BBC News report from August 2020, hospital staff in Ghana were selling PPE on the black market.[211]
Two government workers from the Federal Law Enforcement training Center in North Charleston, South Carolina, were charged in October for conspiracy to steal PPE, obstruction of justice and lying to the FBI.[212]
Destruction in wars[edit | edit source]
During the Tigray War that started in November 2020, looting of the means of survival led not only to emergency conditions of acute food insecurity but also to concerns about management of the COVID-19 pandemic. As of January 2021, only five out of forty hospitals were "physically accessible" and most hospitals outside of the Tigrayan capital Mekelle had been looted or destroyed.[213]
N95 and FFP masks[edit | edit source]
N95 and FFP masks were in short supply and high demand during the COVID-19 pandemic.[214][189] Production of N95 masks was limited due to constraints on the supply of nonwoven polypropylene fabric (which is used as the primary filter), as well as the cessation of exports from China.[51][215] China controls fifty percent of global production of masks, and facing its own coronavirus epidemic, dedicated all its production for domestic use, only allowing exports through government-allocated humanitarian assistance.[51]
United States[edit | edit source]
In March 2020, US President Donald Trump applied the Defense Production Act against the American company 3M, which allows the Federal Emergency Management Agency to obtain N95 respirators from 3M.[216][217] White House trade adviser Peter Navarro said there were concerns that 3M products were not making their way to the US.[216] 3M replied that it has not changed the prices it charges, and was unable to control the prices its dealers or retailers charge.[216]
Jared Moskowitz, the head of the Florida Division of Emergency Management, accused 3M of selling N95 masks directly to foreign countries for cash, instead of to the US. Moskowitz said 3M agreed to authorized distributors and brokers to represent they were selling the masks to Florida, but instead his team for the last several weeks "get to warehouses that are completely empty". He then said the 3M-authorized US distributors later told him the masks Florida contracted for never showed up because the company instead prioritized orders that came in later, for higher prices, from foreign countries (including Germany, Russia, and France).[218][219][220]
Forbes reported that "roughly 280 million masks from warehouses around the US had been purchased by foreign buyers [on 30 March 2020] and were earmarked to leave the country, according to the broker – and that was in one day," causing massive critical shortages of masks in the US.[221][222]
Masks were still in short supply in late September, eight months into the pandemic. The Defense Production Act powers that averted a ventilator shortage were not used as extensively to increase N95 production, despite outcry from healthcare workers. Even though 3M has increased domestic production from 20 million to 95 million masks a month, they say "the demand is more than we, and the entire industry, can supply for the foreseeable future."[223][224] N95 manufacturers and other companies have been reluctant to invest more in domestic mask production because manufacturing in the United States is not profitable for them. There are some American companies who can shift production temporarily to meet the demand for masks but most of them have not received any funding through the DPA. Some have taken the initiative but there were problems with the fit of the masks and obtaining regulatory approvals. 3M and other N95 manufacturers have not entered into any corporate partnerships to share intellectual property or increase N95 production.[223]
Trump gave Rear Admiral John Polowczyk the responsibility for the logistics of PPE. Polowczyk said he believed "hospital systems are making management decisions that might lead to an appearance that we still don't have masks, which is the farthest from the truth."[223]
By February 2021, suppliers had increased production but not enough to meet demand. Companies cited concerns about post-pandemic demand as a reason for not entering the market. Hospitals increased supplies, but even at well-funded hospitals, healthcare workers could be expected to wear their masks for up to a month. Counterfeits continued to pose problems for purchasers.[225] Numerous calls by public health experts had been made to provide high-filtration masks such as N95s or their equivalents to the general public in high-risk settings.[226][227]
On 19 January 2022, the Biden Administration is reported to begin freely providing 400 million N95 masks in the United States.[228]
Germany[edit | edit source]
In early April 2020, the Berlin politician Andreas Geisel alleged that a shipment of 200,000 N95 masks it had ordered from American producer 3M's China facility were intercepted in Bangkok, Thailand and diverted to the United States. 3M said they had no knowledge of the shipment, stating "We know nothing of an order from the Berlin police for 3M masks that come from China." The US government denied any confiscation and said they use appropriate channels for all their purchases.[229][230] Berlin police later confirmed that the shipment was not seized by US authorities.[citation needed]
This revelation outraged the Berlin opposition, whose CDU parliamentary group leader Burkard Dregger accused Geisel of "deliberately misleading Berliners" in order "to cover up its own inability to obtain protective equipment". FDP interior expert Marcel Luthe also criticized Geisel.[231] Politico Europe reported that "the Berliners are taking a page straight out of the Trump playbook and not letting facts get in the way of a good story."[232] The Guardian also reported that "There is no solid proof Trump [nor any other American official] approved the [German] heist."[233]
German citizens decided to contribute to solving the supply crisis by making their own masks and other types of PPE like face shields that gave masks additional protection; the largest group of makers measured 6,800 individuals, collectively producing more than 100,000 pieces of protective equipment.[234]
Canada[edit | edit source]
As more and more countries restricted the export of N95 masks, Novo Textiles in British Columbia announced plans to start producing N95 masks in Canada.[235] AMD Medicom in Quebec had long been the main Canadian company producing N95s, but China, France, the Republic of China (Taiwan) and the United States all banned exports of medical equipment, barring Medicom's factories there from exporting the masks to Canada. The Government of Canada subsequently awarded Medicom a 10-year contract to build a factory to produce masks in Montreal.[236]
Mask industry[edit | edit source]
Manufacturing[edit | edit source]
.jpg)
China[edit | edit source]
As of 2019, mainland China manufactured half the world output of masks.[237] As COVID-19 spread, enterprises in several countries quickly started or increased the production of face masks.[238] Cottage industries and volunteer groups also emerged, manufacturing cloth masks for localized use. They used various patterns, including some with a bend-to-fit nose piece insert. Individual hospitals developed and requested a library of specific patterns.[239][240][241][242]
In the first five months of 2020, 70,802 new companies registered in China to make or trade face masks, a 1,256% increase compared to 2019, and 7,296 new companies registered to make or trade melt blown fabrics, a key component of face masks, a 2,277% rise from 2019.[243]
In April, however, the Chinese government stepped in with tighter regulations. 867 producers of the meltblown fabric were shut down in Yangzhong city alone. Many speculative manufacturers have been forced to quit due to changing export rules and tighter licensing requirements in China and weaker demand for lower quality products globally.[243]
Open Source and Do It Yourself Masks[edit | edit source]
Open Source Medical Supplies coordinated and shared open-source mask designs.[244]
Distribution[edit | edit source]
Some clinical stockpiles have proved inadequate in scale, and the non-medical market demand expanded dramatically as the general public determined that masks were essential, or they began obeying public health mandates, or both.[245]
Between April and June 2020, sellers on Etsy sold 29 million cloth face masks worth an estimated $364 million. Approximately four million people (about seven percent of buyers) visited the website just to buy masks.[246]
Society and culture[edit | edit source]
Attitudes[edit | edit source]
In East Asian societies, a primary reason for mask-wearing is to protect others from oneself.[247][248] The broad assumption behind the act is that anyone, including seemingly healthy people, can be a carrier of the coronavirus.[248] The usage of masks is seen as a collective responsibility to reduce the transmission of the virus.[249] A face mask is thus seen as a symbol of solidarity in Eastern countries.[249] Elsewhere, the need for mask-wearing is still often seen from an individual perspective where masks only serve to protect oneself.[247] In April 2020, a study comparing masking-related perceptions between China and three German speaking countries (Austria, Germany, and Switzerland) also showed that Chinese had stronger pro-masking perceptions than the European participants.[250] However, over the course of the pandemic, people began promoting a new meaning of masking as an act of solidarity to each other.[251][139][252][253] In May 2020, masking was gradually shifting to become a new social norm.[254]
Existing cultural norms and social pressure may impede mask-wearing in public, which explains why masking has been avoided in the West.[256] According to Joseph Tsang, a Hong Kong doctor and infectious disease expert, the promotion of universal masking may resolve perceptions against mask-wearing, because mask-wearing is intimidating if few people wear masks due to cultural barriers, but if all people wear masks it shows a message that people are in this together.[79] A study surveying people in Spain showed that an individual's likelihood of voluntarily wearing a mask is positively correlated with the proportion of uptake in the surrounding area.[257]
Helene-Mari van der Westhuizen et al. point out that successful implementation of public masking policies, especially in communities that have no cultural traditions for such interventions, requires a reframing of social meanings and moral worth, and that public messages help to conceptualize who typically wear masks and what the moral valence of masking is.[258] They note that the earliest members who wear face coverings may be seen as deviant when the community starts to adopt masking, but that changing narratives will generate new meanings that construe those who do not mask as deviant.[258] Their argument is that public health messaging about face coverings should shift from masks as a medical intervention to masks as a social practice based on values such as social responsibility and solidarity, as a successful uptake requires face coverings to be grounded in the social and cultural realities of affected communities.[258] Clemens Eisenmann and Christian Meyer argue that the question, how the meaning of wearing face masks develops in society, depends on their practical and public uses within everyday social interactions.[259] They explain that masking has destabilized interactional infrastructures embedded in routines, revealing both taken-for-granted infrastructures of everyday life – including social inequalities (such as those of people reliant on lip reading) and moral evaluations in transcultural situations (such as those involving implicit racism in which the health instructions of essential workers belonging to certain groups are disregarded) – and new challenges on the interactional level.[259]
In the Western world, the public usage of masks still often carries a large stigma,[247][249][260] as it is seen as a sign of sickness.[260] This stigmatization is a large obstacle to overcome, because people may feel too ashamed to wear a mask in public and therefore opt to not wear one.[261] There is also a divide within the Western world, as seen in the Czech Republic and Slovakia where mass mobilization has occurred to reinforce the solidarity in mask-wearing since March 2020.[247][needs update]
Mask-wearing has been called a prosocial behavior in which one protects others within their community.[262][263][264] On social media, there has been an effort with the #masks4all campaign to encourage people to use masks.[265] Nevertheless, there have been many occurrences of violence and hostility by people who became aggressive after they were requested to wear a mask or saw people wearing masks in customer-based establishments.[266][267][268][269] Multiple people have been killed in attacks by people who refused to mask.[270] It has led to concerns about worker safety, so employees have been discouraged to actively enforce masking policies due to the potential of hostile situations, while enforcement by official authorities is severely lacking.[271]
Masking has been subjected to racial politics in Western countries.[272] For instance, it has been heavily racialized as an Asian phenomenon.[249][259] This has been reinforced in a lot of media discourses, where stories about the pandemic are often accompanied by unrelated imagery of Asian people in masks.[272][273] The focus on race has brought hostility towards Asians who are confronted with the choice to mask as precaution while they face discrimination for it.[272][274] Huang Yinxiang, a sociologist from the University of Manchester, described maskaphobia (negative prejudice, fear or bitter hatred against people wearing face masks) as making Asians in Western countries into targets for racists who want to legitimize xenophobia during the COVID-19 outbreak.[275] Likewise, people from certain groups such as Black Americans may not feel comfortable wearing masks, especially those that are not clearly medical but homemade masks, due to concerns of racial profiling.[276][277][278]

There have also been concerns that wearing masks may also further isolate disadvantaged communities. Concerns had been expressed that masks would make communication difficult for people who are deaf or hard-of-hearing.[279][280] This led to calls for wider distributions of transparent masks, which allow for lip reading.[279][280] Similar concerns over difficulty in communicating have been expressed by those who may depend on dogs for therapeutic or social reasons, as the animals depend on body language such as facial expressions.[281] Conversely, people who are exempt from wearing masks on medical grounds or due to a disability, fear they will be subjected to abuse for not wearing a mask, even if they are legally exempt from doing so.[282] For instance, in the United Kingdom, the charity Disability Rights UK received numerous reports about people being confronted on trains and buses.[282] Health organizations such as the American Lung Association commented that, even though there may be people who will seek an exemption, the individual's concerns needs to be weighed against the societal needs to limit the spread of the virus.[283][284] However, anti-maskers have called upon bogus claims about legal or medical exemptions in their refusal to mask.[283] They have, for instance, claimed that the Americans with Disabilities Act (designed to prohibit discrimination based on disabilities) allows exemption from mask requirements, but the United States Department of Justice responded that the act "does not provide a blanket exemption to people with disabilities from complying with legitimate safety requirements necessary for safe operations".[285]
There are feelings of mask fatigue among the general public, which is exacerbated by frustrations about people who are not taking the mask and other guidelines seriously as the pandemic and its intensity continues on.[286]
Trends[edit | edit source]
Among the European countries surveyed by YouGov in the first half of 2020, the likelihood for people to mask was split: In Northern Europe (e.g., Finland, Sweden, Norway, and Denmark), people were very unlikely to wear a mask.[287] In Western Europe (e.g., Italy, Spain, France, and Germany), people were initially unlikely to use a mask, but mask wearing greatly changed from low levels in March to higher levels in May.[287] A similar, if delayed, pattern was seen in some northern European countries. For example, mask usage was very low in Denmark up until the summer of 2020, but rapidly increased in the autumn as rules on their use in publicly accessible indoor places were introduced.[288] An exception was the United Kingdom where mask usage only grew gradually during in the first half of 2020,[287] but it rose very quickly after official policy changes in July mandated masking in stores.[289]
A survey among people from the United States (conducted from April to June 2020) indicates that age was a factor on whether people were likely to wear a mask, as the likelihood rose with the age group, but the reported use of face masks increased significantly across all age groups over time.[290] Furthermore, people who did not report mask use also reported engaging in significantly fewer other mitigation behaviors than those who did report mask use.[290]
Gender plays a role in the willingness to wear masks during the pandemic; men are overall less inclined to mask in public than women.[291][292][293] There are indications that men are more likely to feel negative emotions (such as shame) and stigma for wearing masks.[291][292] It is suggested that this male behavior is driven by a sense of masculinity, where the act of masking is possibly perceived to run counter to it, which leads to an increase in men not wearing masks during the pandemic.[294][295] A survey among participants recruited from Amazon Mechanical Turk about face mask perceptions found that men and women may have different reasons when they do not wear masks in public: Men were more likely to see masks as an infringement upon their independence and women were more likely to perceive masks as being uncomfortable, while perceptions on efficacy, accessibility, compensation, inconvenience, appearance, and attention did not differ.[296]
Governmental role[edit | edit source]
.png)
The pandemic has raised questions about the role of governments in mask policies, either voluntary or mandatory policies, especially in terms of the social and behavioral consequences involving the general public.[264]
The results from a study surveying people in Germany indicate that the act of wearing a mask, independent of the policy, is considered a social contract in which compliant people perceive each other more positively and noncompliance is negatively evaluated.[264] However, it also suggests that voluntary policies have the potential effect to increase polarization and thus cause more stigmatization.[264] The authors recommended that countries and communities should adopt a mandatory policy along with explicit communication of the benefits of both masking (e.g., risk reduction, mutual protection, positive social signaling) and mandatory policies (e.g., fairness, less stigmatization, higher effectiveness) to encourage the public to wear masks.[264]
World leaders as role models for masking have also received much scrutiny, as they are key to convey the critical public health message to the public.[297][298] For example, Slovakia has been cited as a country where its public figures (including President Zuzana Čaputová and her administration) set the example by wearing masks and played a crucial role to normalize masks.[299] In contrast, in the United States, President Donald Trump and his administration have come under criticism for communicating an inconsistent and confusing message about masking.[300][301] They have often been criticized for undercutting national and local public health advice to wear masks.[302][303]
Politics[edit | edit source]
.jpg)
Although authorities, especially in Asia, have been recommending people to wear face masks in public, in many other parts of the world, conflicting advice has caused much confusion among the general population.[305] Several governments and institutions, such as in the United States, initially dismissed the use of face masks by the general population, often with misleading or incomplete information about the usefulness of masks.[306][307][308] Commentators have attributed the anti-mask messaging to efforts to manage the mask shortages, as governments did not act quickly enough, remarking that the claims go beyond the science or were simply lies.[308][309][310][311] On 12 June 2020, Anthony Fauci, a key member of the White House coronavirus task force, confirmed that the American public were not told to wear masks from the beginning due to the shortages of masks and explained that masks do actually work.[312][313][314][315][316][excessive citations]
In the United States, public masking has become a political issue, as opponents argue that it inhibits personal freedom and proponents emphasize the importance of masks for public health.[317] Some people may see it as a political statement.[318] Party affiliation partly determined how likely people were to embrace the wearing of masks in public.[318][319] Democrats were more likely to wear masks than Republicans.[318][319] Masks have become an aspect of the culture war that has emerged over the course of the pandemic.[317][318][319] Commentators argue that the resistance against masks partly stems from the confusing and mixed messaging about masking.[317][320][321]
Matthew Facciani, a sociologist at Vanderbilt University, says the uncertainty from health experts during the early days of the pandemic paved the way for political leaders to become a prominent source for guidance and clarity.[322] He argues that, once mask wearing became informed by political beliefs, it is difficult to correct due to the motivation to protect one's identity in relation to a political group and the reinforcement from political echo chambers, no matter that scientists began to better understand the severity of the virus and the evidence in favor for mask wearing became clearer.[322] Moreover, how people observe the masking rules seems to be different across countries and these differences may be attributed to cultural or management factors.[250]
In April 2020, health officials from Taiwan's Central Epidemic Command Center (CECC) pushed back on school bullying of boys in pink face masks.[323] The CECC officials and Minister of Health and Welfare Chen Shih-chung wore pink masks to challenge gender norms at a press conference, while various government agencies demonstrated solidarity by changing the colors on their Facebook pages to pink.[323] The minister later tweeted "Pink is for everyone and no colour is exclusive for girls or boys. Gender Equality lies at the heart of Taiwan values."[323] The press conference was held amid reports that male students were too embarrassed to wear their pink face masks, jeopardizing their safety and the safety of others in the face of COVID-19.[323]
Opposition[edit | edit source]
In some countries, large rallies have taken place in protest against masking mandates.[324][325][326] In Canada, the anti-mask crowd has hailed their protests as the so-called "March to Unmask".[326][327] In the United Kingdom, new protests came in the wake of the official announcement that masking will be compulsory in shops.[324] After eight months since the beginning of the lockdown in the Czech Republic, mass manifestations against the restrictions imposed by the government arose.[328][329] Some anti-mask protestors have co-opted the feminist slogan "my body, my choice"[330][331][332] and the Black Lives Matter slogan "I can't breathe".[333] Businesses have also been purposely disrupted by anti-maskers (purportedly in defense of their constitutional rights).[334]
According to Moe Gelbart, executive director of the Thelma McMillen Recovery Center, anti-maskers' behaviors do not appear only from the facts they hear, but the problems also come from the meaning they give to those facts. He identifies several key psychological reasons that prompt them to not wear a mask: First, denial is seen in some people who feel worried and anxious by masks as it interferes with their belief and desire that everything is alright. Second is a sense of invulnerability, as some people and especially younger individuals believe nothing bad will happen to them and are thus prone to risk-taking behaviors. Third, behavioral drift is seen among some people who find it difficult to maintain behaviors intended for prevention rather than treatment. Fourth, some people may have issues related to authority due to mistrust of science or tribe identification with powerful figures. Fifth, the act of covering one's face has an association with "bad", such as criminals or as an intention to hide something one is ashamed of. Sixth, some people do not want to admit fear and vulnerability, which they associate with the act of wearing a mask.
In the United States, opposition to mask-wearing during the COVID-19 pandemic came during then-President Donald Trump's politicization of science[335] and more generally during decades-old period of politicization of science. American opposition to mask-wearing during pandemics is not new; during the 1918 influenza pandemic, the Anti-Mask League was established in San Francisco, California.[336]
In May 2021, Vice reported that some members of the anti-vaccine community were, promoting the use of masks and social distancing to protect themselves from those who have received vaccines, citing false claims that those vaccinated for COVID-19 "shed" spike proteins that can be harmful to people in their proximity, and discredited research scientist Judy Mikovits claimed that she had been kicked off a plane for wearing a mask lined with colloidal silver.[337]
Religion[edit | edit source]
Christian clergy from the Lutheran, Catholic, Presbyterian, Anglican, Baptist and Latter-day Saint traditions, as well as those from the Jewish, Buddhist and Unitarian religions have implored people to wear masks.[338]
Fashion[edit | edit source]
As the pandemic progressed people began making use of face masks as accessories,[339][340][341][342] matching them to their outfits and so on.[343][344] Early in the pandemic, people and businesses from the fashion industry responded to official calls for help in overcoming the shortages of protective personal equipment including face masks.[345] These masks were sheerly utilitarian as the only consideration at the time was function.[346] What began as a public health necessity however gradually evolved into a new category of accessories subject to similar design and marketing considerations as other accessories.[347] Fashion brands eventually reopened their factories for production due to the increasing demand for masks and started to manufacture masks in a wider variety of styles.[340] Smaller brands, who primarily sold their products online, found that selling masks was a good strategy to maintain sales.[348] Etsy became a major online platform where many designers sold their masks.[348] Designers started making masks that matched other pieces of clothing and accessories,[349][350] a trend which may have begun unintentionally as even fabric remnants were repurposed.[350]
The city of Vilnius in Lithuania held a "Mask Fashion Week" in May 2020, which was promoted with billboards (with no catwalks or displays) around the city featuring local people including Mayor Remigijus Simasius wearing face masks.[351]
The Walt Disney Company introduced uniform face masks for their employees at Walt Disney World and Disneyland in the United States.[352][353]
Environment[edit | edit source]
Large numbers of disposed face masks have led to an increase in plastic waste, negatively impacting the environment.[354][355][356] Moreover, the production of face masks also contributes the emission of carbon dioxide, which accelerates global warming.[357] Considering the risk of plastic pollution, researchers have focused on using biodegradable polymers to fabricate facemask with antimicrobial properties [358]
Linguistic aspects[edit | edit source]
Due to the rarity of their use in non-medical settings outside East Asia, many languages lacked commonly used terms for facemasks, especially since legal issues prevent the usage of terms which might imply medical standards the masks do not meet.[359] In languages such as Saterland Frisian public competitions were held[360] to create a neologism for the device in the language and thus not having to rely on loanwords or calques.[361][362] The Friisk Foriining held a similar competition for the North Frisian language.[363][364]
Comparison by countries and territories[edit | edit source]
| Country/territory | % |
|---|---|
| 92 | |
| 90 | |
| 88 | |
| 86 | |
| 86 | |
| 85 | |
| 85 | |
| 84 | |
| 83 | |
| 82 | |
| 81 | |
| 80 | |
| 80 | |
| 79 | |
| 79 | |
| 75 | |
| 75 | |
| 74 | |
| 71 | |
| 67 | |
| 65 | |
| 41 | |
| 23 | |
| 19 | |
| 10 | |
| 8 | |
| 7 | |
| 6 | |
| 5 | |
| 4 |
 Argentina: After the appearance of three asymptomatic cases, the capital Buenos Aires introduced compulsory masking since 14 April 2020. Wearing a mask was made obligatory for everyone on public transit, entering a market and everyone who contacts with the public in their position. Violators can face a fine. Authorities also prohibited the sale of N95 face masks to non-medical workers, suggesting the general public to use home-made masks instead.[366]
Argentina: After the appearance of three asymptomatic cases, the capital Buenos Aires introduced compulsory masking since 14 April 2020. Wearing a mask was made obligatory for everyone on public transit, entering a market and everyone who contacts with the public in their position. Violators can face a fine. Authorities also prohibited the sale of N95 face masks to non-medical workers, suggesting the general public to use home-made masks instead.[366].svg.png) Australia: The federal Department of Health does not recommend the wearing of face masks by the general public when you are well, but in regions where there is community transmission people may choose to, or be required to, wear a mask. However, all states and territories mandate masks in some or all settings as of September 2021.[367] In places where there is community transmission and it is difficult to keep a distance, properly-worn masks are recognized as an important protective measure.[368] First in the state of Victoria, face coverings became compulsory on 22 July 2020 in the metropolitan Melbourne or Mitchell Shire areas when outside of one's home.[369] This was later extended to all of Victoria from 3 August. All states and territories have since then mandated masks at some point in time, depending on the outbreak situation at the location. The federal Department of Health have mandated masks at airports and on domestic flights.[370]
Australia: The federal Department of Health does not recommend the wearing of face masks by the general public when you are well, but in regions where there is community transmission people may choose to, or be required to, wear a mask. However, all states and territories mandate masks in some or all settings as of September 2021.[367] In places where there is community transmission and it is difficult to keep a distance, properly-worn masks are recognized as an important protective measure.[368] First in the state of Victoria, face coverings became compulsory on 22 July 2020 in the metropolitan Melbourne or Mitchell Shire areas when outside of one's home.[369] This was later extended to all of Victoria from 3 August. All states and territories have since then mandated masks at some point in time, depending on the outbreak situation at the location. The federal Department of Health have mandated masks at airports and on domestic flights.[370] Austria: Everyone entering a supermarket, a grocery store, or a drug store or using public transportation must wear a face mask, mandatory since 14 April 2020.[371][372][373]
Austria: Everyone entering a supermarket, a grocery store, or a drug store or using public transportation must wear a face mask, mandatory since 14 April 2020.[371][372][373] Bahamas: On 19 April 2020, the prime minister announced that wearing a mask or covering one's face with clothing is mandatory in public. Employers must provide their employees who are serving the general public with masks.[374]
Bahamas: On 19 April 2020, the prime minister announced that wearing a mask or covering one's face with clothing is mandatory in public. Employers must provide their employees who are serving the general public with masks.[374] Bahrain: The Kingdom made wearing face masks in public areas compulsory for citizens and residents as well as shop workers.[375]
Bahrain: The Kingdom made wearing face masks in public areas compulsory for citizens and residents as well as shop workers.[375] Benin: From 8 April 2020, Benin's authorities began enforcing the mandatory wearing of face masks to halt the coronavirus.[376]
Benin: From 8 April 2020, Benin's authorities began enforcing the mandatory wearing of face masks to halt the coronavirus.[376] Bosnia and Herzegovina: Wearing a face mask is compulsory.[377][378]
Bosnia and Herzegovina: Wearing a face mask is compulsory.[377][378] Bulgaria: Bulgaria's government passed an order imposing an obligation to wear face masks on 30 March 2020. The order was cancelled the next day and changed into a recommendation, due to legal complaints.[379]
Bulgaria: Bulgaria's government passed an order imposing an obligation to wear face masks on 30 March 2020. The order was cancelled the next day and changed into a recommendation, due to legal complaints.[379] Cambodia: Businesses started to require customers to wear masks.[380]
Cambodia: Businesses started to require customers to wear masks.[380] Cameroon: On 6 April, mayor of Douala announced that wearing a mask will be mandatory to slow the spread of coronavirus.[381]
Cameroon: On 6 April, mayor of Douala announced that wearing a mask will be mandatory to slow the spread of coronavirus.[381].svg.png) Canada: Since April 6, 2020, health officials recommend wearing non-medical masks in situations where physical distancing from others is difficult (like buying groceries, or public transit).[382] The use of face masks indoor is mandatory in all of the country except Alberta (excluding Edmonton) and Saskatchewan as of March 1, 2022.[383][384]
Canada: Since April 6, 2020, health officials recommend wearing non-medical masks in situations where physical distancing from others is difficult (like buying groceries, or public transit).[382] The use of face masks indoor is mandatory in all of the country except Alberta (excluding Edmonton) and Saskatchewan as of March 1, 2022.[383][384] Chile: From 8 April 2020, Chilean Health Minister announced wearing a mask is mandatory in public transit.[385]
Chile: From 8 April 2020, Chilean Health Minister announced wearing a mask is mandatory in public transit.[385] China: Healthy individuals are advised to wear disposable medical masks in public places.[386][387] Some local governments require wearing masks when going outside. Shanghai makes wearing masks mandatory in public places.[388] Wearing masks is also mandatory during the entire journey if taking the public transport.
China: Healthy individuals are advised to wear disposable medical masks in public places.[386][387] Some local governments require wearing masks when going outside. Shanghai makes wearing masks mandatory in public places.[388] Wearing masks is also mandatory during the entire journey if taking the public transport.
 Hong Kong: Masks were made mandatory for public transport and public places since June 2020.[389] In the 2019–20 Hong Kong protests, some protestors wore surgical masks amongst other types of mask to avoid recognition, and the government tried to ban such use.[390]
Hong Kong: Masks were made mandatory for public transport and public places since June 2020.[389] In the 2019–20 Hong Kong protests, some protestors wore surgical masks amongst other types of mask to avoid recognition, and the government tried to ban such use.[390]
 Colombia: In response to recommendations from the WHO, Colombia changed its policy on the use of masks and made it mandatory throughout the country for the use of public transport during the coronavirus emergency.[391]
Colombia: In response to recommendations from the WHO, Colombia changed its policy on the use of masks and made it mandatory throughout the country for the use of public transport during the coronavirus emergency.[391] Croatia: Since 8 July 2020, everyone entering any enclosed place, like shops and other buildings, must wear a face mask.[392]
Croatia: Since 8 July 2020, everyone entering any enclosed place, like shops and other buildings, must wear a face mask.[392] Cuba: On 11 March 2020, the government urged citizens to make their own masks, while the textile industry was drafted to fabricate them. People were advised to carry several cloth masks with them, depending on how many hours they plan to spend in public areas.[393] Later, wearing a mask was made mandatory.[394]
Cuba: On 11 March 2020, the government urged citizens to make their own masks, while the textile industry was drafted to fabricate them. People were advised to carry several cloth masks with them, depending on how many hours they plan to spend in public areas.[393] Later, wearing a mask was made mandatory.[394] Czech Republic: From mid-March it was forbidden to go out in public without wearing a mask, or covering one's nose and mouth until 25 May 2020.[395] Wearing face masks has been required again since 10 September 2020 in public indoor places, including public transportation,[396] and since 21 October 2020 in outdoor public places and cars.[397] While in the spring 2020 the obligation applied unconditionally, even if one was alone in nature or alone in a car (which has been criticized), the autumn measure includes an exception for the case where distances of at least two meters are maintained between people (in outdoor) and for the cases where only members of the same household are nearby.
Czech Republic: From mid-March it was forbidden to go out in public without wearing a mask, or covering one's nose and mouth until 25 May 2020.[395] Wearing face masks has been required again since 10 September 2020 in public indoor places, including public transportation,[396] and since 21 October 2020 in outdoor public places and cars.[397] While in the spring 2020 the obligation applied unconditionally, even if one was alone in nature or alone in a car (which has been criticized), the autumn measure includes an exception for the case where distances of at least two meters are maintained between people (in outdoor) and for the cases where only members of the same household are nearby. Dominican Republic: Since 16 April 2020, the use of face masks is mandatory in all public spaces and in the workplace.[398]
Dominican Republic: Since 16 April 2020, the use of face masks is mandatory in all public spaces and in the workplace.[398] DR Congo: Since 20 April 2020, wearing masks in the capital of Kinshasa is mandatory.[399]
DR Congo: Since 20 April 2020, wearing masks in the capital of Kinshasa is mandatory.[399] Denmark: Except in the first peak of cases in spring 2020, Danish authorities have generally required masks in publicly accessible indoor places during periods with clearly rising or high levels of COVID-19 in the country. On 22 August 2020, as cases had started rising, the use of face masks was made mandatory in public transport.[400] On 29 October 2020, the executive order was extended to include all publicly accessible indoor areas.[125] The requirement was gradually outphased from 14 June to 1 September 2021,[401] but reintroduced 28–29 November as the Omicron variant began spreading.[402][403] In general, Danes have closely followed the recommendations of the national health authorities, with low rates of mask use when not required and high rates of compliance in periods where required.[288][404]
Denmark: Except in the first peak of cases in spring 2020, Danish authorities have generally required masks in publicly accessible indoor places during periods with clearly rising or high levels of COVID-19 in the country. On 22 August 2020, as cases had started rising, the use of face masks was made mandatory in public transport.[400] On 29 October 2020, the executive order was extended to include all publicly accessible indoor areas.[125] The requirement was gradually outphased from 14 June to 1 September 2021,[401] but reintroduced 28–29 November as the Omicron variant began spreading.[402][403] In general, Danes have closely followed the recommendations of the national health authorities, with low rates of mask use when not required and high rates of compliance in periods where required.[288][404] Ecuador: On 8 April 2020, the Emergency Operations Committee (COE) decided to make face masks obligatory in public spaces.[405]
Ecuador: On 8 April 2020, the Emergency Operations Committee (COE) decided to make face masks obligatory in public spaces.[405] Egypt: On 30 May 2020, the wearing of face masks in public places and on public transportation became mandatory; failure to comply can result in fines of up to EGP4,000 (US$247).[406]
Egypt: On 30 May 2020, the wearing of face masks in public places and on public transportation became mandatory; failure to comply can result in fines of up to EGP4,000 (US$247).[406] Ethiopia: The Council of Ministers approved a regulation that outlaws handshakes, and obligates the use of face masks in public places.[407]
Ethiopia: The Council of Ministers approved a regulation that outlaws handshakes, and obligates the use of face masks in public places.[407] Finland: Initially the Government did not recommend face masks to be used by the general public, but said that they can be used in situations where it is not possible to keep a distance. If someone chooses to wear a mask, the Finnish Institute for Health and Welfare notes that it is important that it is used correctly, and that general distancing and hygiene guidelines should still be followed. On 13 August 2020, an official recommendation was given to use face masks in public transportation in hospital districts that have had new COVID-19 cases within the previous 14 days.[408]
Finland: Initially the Government did not recommend face masks to be used by the general public, but said that they can be used in situations where it is not possible to keep a distance. If someone chooses to wear a mask, the Finnish Institute for Health and Welfare notes that it is important that it is used correctly, and that general distancing and hygiene guidelines should still be followed. On 13 August 2020, an official recommendation was given to use face masks in public transportation in hospital districts that have had new COVID-19 cases within the previous 14 days.[408] France: On 3 March 2020, the government issued a degree announcing requisition of stocks of FFP2 and anti-splash masks until 31 May 2020.[409] On 8 May 2020, the government announced that 200 million masks per week will be available starting on 11 May 2020: 100 million for medical workers and 100 million for the general public.[410] From July 2020, France made it compulsory for people to wear masks in shops and other enclosed public spaces.[411]
France: On 3 March 2020, the government issued a degree announcing requisition of stocks of FFP2 and anti-splash masks until 31 May 2020.[409] On 8 May 2020, the government announced that 200 million masks per week will be available starting on 11 May 2020: 100 million for medical workers and 100 million for the general public.[410] From July 2020, France made it compulsory for people to wear masks in shops and other enclosed public spaces.[411] Gabon: On 10 April 2020, the Gabonese government announced individuals in all parts of the country are required to wear masks in public to limit the spread of COVID-19.[412]
Gabon: On 10 April 2020, the Gabonese government announced individuals in all parts of the country are required to wear masks in public to limit the spread of COVID-19.[412] Germany: On 31 March 2020, city-county Jena, Thuringia, was the first large German city to introduce an obligation to wear masks, or makeshift masks including scarves, in supermarkets, public transport, and buildings with public traffic, from 6 April 2020. On 2 April, the Robert Koch Institute, the federal epidemic authority, changed its previous recommendation that only people with symptoms should wear masks to also include people without symptoms.[413][414] Later in April, Germany made the wearing of cloth face masks mandatory on public transport, as well as for shopping in most German states.[415] Some German states expanded the regulations to include outdoor markets.[416]
Germany: On 31 March 2020, city-county Jena, Thuringia, was the first large German city to introduce an obligation to wear masks, or makeshift masks including scarves, in supermarkets, public transport, and buildings with public traffic, from 6 April 2020. On 2 April, the Robert Koch Institute, the federal epidemic authority, changed its previous recommendation that only people with symptoms should wear masks to also include people without symptoms.[413][414] Later in April, Germany made the wearing of cloth face masks mandatory on public transport, as well as for shopping in most German states.[415] Some German states expanded the regulations to include outdoor markets.[416] Ghana: Use of face masks would be made mandatory in public spaces including public transport. However, surveys show about 22% of public transport vehicles would have fewer than three people without masks, with the vast majority having only partial or non-compliance to the policy on face masks.[417]
Ghana: Use of face masks would be made mandatory in public spaces including public transport. However, surveys show about 22% of public transport vehicles would have fewer than three people without masks, with the vast majority having only partial or non-compliance to the policy on face masks.[417] Guatemala: From 8 April 2020, Guatemalan president Alejandro Giammattei makes it mandatory to wear a face mask in public.[418]
Guatemala: From 8 April 2020, Guatemalan president Alejandro Giammattei makes it mandatory to wear a face mask in public.[418] Guinea: Guinean President Alpha Conde decided to make wearing masks compulsory.[419]
Guinea: Guinean President Alpha Conde decided to make wearing masks compulsory.[419] Honduras: From 7 April 2020, Honduras President announced all citizens will now be required to cover their mouths when they are outside.[420]
Honduras: From 7 April 2020, Honduras President announced all citizens will now be required to cover their mouths when they are outside.[420] Hungary: Masks became mandatory indoors on April 23, 2020. Later on, the mandate was expanded to all outdoor areas.[421]
Hungary: Masks became mandatory indoors on April 23, 2020. Later on, the mandate was expanded to all outdoor areas.[421] Iceland: Masks are not widely worn and are not recommended by the authorities.[422]
Iceland: Masks are not widely worn and are not recommended by the authorities.[422] India: On 3 April 2020, the Office of the Principal Scientific Adviser to the Government of India issued an advisory and manual, asking healthy people to wear handmade reusable face covers when stepping out of their homes, especially for those in densely populated areas.[423][424] Some individual states, like Odisha, West Bengal, Maharashtra and Uttar Pradesh made wearing of masks compulsory in public places.[425][426][427]
India: On 3 April 2020, the Office of the Principal Scientific Adviser to the Government of India issued an advisory and manual, asking healthy people to wear handmade reusable face covers when stepping out of their homes, especially for those in densely populated areas.[423][424] Some individual states, like Odisha, West Bengal, Maharashtra and Uttar Pradesh made wearing of masks compulsory in public places.[425][426][427] Indonesia: Citizens were ordered to wear face masks when they leave the house.[428]
Indonesia: Citizens were ordered to wear face masks when they leave the house.[428] Ireland: Since 10 August 2020, masks were made mandatory on public transport and within retail and public realms, non-compliance is subject to fines of €80 to one month imprisonment. Additionally, masks were recommended in busy outdoor areas and workplace offices.[429][430]
Ireland: Since 10 August 2020, masks were made mandatory on public transport and within retail and public realms, non-compliance is subject to fines of €80 to one month imprisonment. Additionally, masks were recommended in busy outdoor areas and workplace offices.[429][430] Israel: All residents are asked to wear face masks when in public.[431]
Israel: All residents are asked to wear face masks when in public.[431] Italy: Regions of Lombardy and Tuscany made wearing a face mask compulsory before going out in early April 2020.[432] As of 8 October 2020, a national-level mask mandate requires people to wear masks outside as well as indoors[433]
Italy: Regions of Lombardy and Tuscany made wearing a face mask compulsory before going out in early April 2020.[432] As of 8 October 2020, a national-level mask mandate requires people to wear masks outside as well as indoors[433] Ivory Coast: From April 2020, 26 masks have become compulsory to enter shopping malls or supermarkets in the Southern suburb of Abidjan, Marcory.[434]
Ivory Coast: From April 2020, 26 masks have become compulsory to enter shopping malls or supermarkets in the Southern suburb of Abidjan, Marcory.[434] Japan: Masks have been widely used by healthy individuals despite absence of official advice to do so.[435] On 1 March 2020, prime minister Shinzo Abe enacted a policy in Hokkaido instructing manufacturers to sell face masks directly to the government, which would then deliver them to residents.[436]
Japan: Masks have been widely used by healthy individuals despite absence of official advice to do so.[435] On 1 March 2020, prime minister Shinzo Abe enacted a policy in Hokkaido instructing manufacturers to sell face masks directly to the government, which would then deliver them to residents.[436] Kenya: Wearing a face mask is compulsory since 4 April 2020. The government has Kenyans to strictly observe social distancing, which has been proved to one of the most efficient ways of preventing infection risks.[437]
Kenya: Wearing a face mask is compulsory since 4 April 2020. The government has Kenyans to strictly observe social distancing, which has been proved to one of the most efficient ways of preventing infection risks.[437] Liberia: From 21 April 2020, it is now compulsory to wear a face mask or covering in public.[438]
Liberia: From 21 April 2020, it is now compulsory to wear a face mask or covering in public.[438] Lithuania: Wearing a face mask or any other means of covering one's nose and mouth in public places is compulsory since 10 April 2020.
Lithuania: Wearing a face mask or any other means of covering one's nose and mouth in public places is compulsory since 10 April 2020. Luxembourg: From 20 April 2020, wearing a mask is mandatory in places where it is not possible to keep enough distance to others such as supermarkets or on public transport.[439]
Luxembourg: From 20 April 2020, wearing a mask is mandatory in places where it is not possible to keep enough distance to others such as supermarkets or on public transport.[439] Malaysia: On 17 March 2020, Malaysia banned exports of medical and surgical masks, to meet local demand.[440] The government has announced that masks are made mandatory in public transport and all public places from 1 August 2020, adding that those who did not comply could be given a RM1,000 (US$235) fine under the nation's Prevention and Control of Infectious Diseases Act. From 1 April 2022, mask wearing is relaxed outdoors such as villages and countryside areas, although mask wearing is still needed at indoor and crowded areas such as Melaka and Johor Bahru.[441][442][443]
Malaysia: On 17 March 2020, Malaysia banned exports of medical and surgical masks, to meet local demand.[440] The government has announced that masks are made mandatory in public transport and all public places from 1 August 2020, adding that those who did not comply could be given a RM1,000 (US$235) fine under the nation's Prevention and Control of Infectious Diseases Act. From 1 April 2022, mask wearing is relaxed outdoors such as villages and countryside areas, although mask wearing is still needed at indoor and crowded areas such as Melaka and Johor Bahru.[441][442][443]
 Selangor: On 22 July 2020, in an interview with Astro Awani, head of the Selangor COVID-19 task force and former Minister of Health Dr. Dzulkefly Ahmad stressed that face coverings should be worn at all public places, except in one's own residence or car.[444]
Selangor: On 22 July 2020, in an interview with Astro Awani, head of the Selangor COVID-19 task force and former Minister of Health Dr. Dzulkefly Ahmad stressed that face coverings should be worn at all public places, except in one's own residence or car.[444]
 Mexico: From 17 April 2020, all Mexico City Metro passengers must wear masks while inside stations and on trains, Mayor Claudia Sheinbaum announced on 15 April 2020.[445]
Mexico: From 17 April 2020, all Mexico City Metro passengers must wear masks while inside stations and on trains, Mayor Claudia Sheinbaum announced on 15 April 2020.[445] Mongolia: Wearing a mask is now mandatory while riding public transportation in Ulaanbaatar. Public officials and news broadcasters had even adopted to wearing masks through press conferences and news broadcasts.[446]
Mongolia: Wearing a mask is now mandatory while riding public transportation in Ulaanbaatar. Public officials and news broadcasters had even adopted to wearing masks through press conferences and news broadcasts.[446] Morocco: Wearing a face mask is compulsory.[447]
Morocco: Wearing a face mask is compulsory.[447] Mozambique: The Mozambican government announced on 8 April 2020 that wearing face masks is now compulsory on all forms of passenger transport, and wherever groups of people are gathered.[448]
Mozambique: The Mozambican government announced on 8 April 2020 that wearing face masks is now compulsory on all forms of passenger transport, and wherever groups of people are gathered.[448] Netherlands: Facemasks became mandatory in Dutch public transport on 1 June 2020[449] and were mandatory in parts of the busy inner cities of Amsterdam and Rotterdam between 5 and 31 August 2020.[450][451] In other places face masks were not mandatory but on 30 September 2020 the government for the first time encouraged people to wear face masks in public indoor places.[452][453] Between 1 December 2020 and 26 June 2021, face masks were mandatory in public indoor places such as shops.[454][455]
Netherlands: Facemasks became mandatory in Dutch public transport on 1 June 2020[449] and were mandatory in parts of the busy inner cities of Amsterdam and Rotterdam between 5 and 31 August 2020.[450][451] In other places face masks were not mandatory but on 30 September 2020 the government for the first time encouraged people to wear face masks in public indoor places.[452][453] Between 1 December 2020 and 26 June 2021, face masks were mandatory in public indoor places such as shops.[454][455] New Zealand: At alert level 1 face masks are not mandatory, but are encouraged on public transport by the Ministry of Health. Community transmission rates in New Zealand are low, but an increase in alert level will instate different advice around the types and use of face masks.[456] However, face masks have become mandatory now due to alert level 4.[1] Archived 30 August 2021 at the Wayback Machine
New Zealand: At alert level 1 face masks are not mandatory, but are encouraged on public transport by the Ministry of Health. Community transmission rates in New Zealand are low, but an increase in alert level will instate different advice around the types and use of face masks.[456] However, face masks have become mandatory now due to alert level 4.[1] Archived 30 August 2021 at the Wayback Machine North Korea: Wearing face masks became obligatory in February, 2020
North Korea: Wearing face masks became obligatory in February, 2020 North Macedonia: As of 22 April 2020, citizens of Kumanovo, Tetovo, and Prilep must wear protective masks and gloves outside their homes, at public places, outdoor and indoor areas, markets, and shops announced the government.[457]
North Macedonia: As of 22 April 2020, citizens of Kumanovo, Tetovo, and Prilep must wear protective masks and gloves outside their homes, at public places, outdoor and indoor areas, markets, and shops announced the government.[457] Norway: The Norwegian Institute of Public Health does not recommend the wearing of face masks by the general public. Levels of the virus in Norway are low, but if there is an increase in virus transmission, the authorities will review the guidelines again.[458]
Norway: The Norwegian Institute of Public Health does not recommend the wearing of face masks by the general public. Levels of the virus in Norway are low, but if there is an increase in virus transmission, the authorities will review the guidelines again.[458] Pakistan: The Balochistan government on 18 April 2020 told citizens to wear face masks when going outside. According to provincial government spokesperson Liaquat Shahwani, citizens have been urged to wear masks or to cover their faces with any cloth in the wake of the COVID-19 outbreak.[459]
Pakistan: The Balochistan government on 18 April 2020 told citizens to wear face masks when going outside. According to provincial government spokesperson Liaquat Shahwani, citizens have been urged to wear masks or to cover their faces with any cloth in the wake of the COVID-19 outbreak.[459] Panama: Panama has made it mandatory to wear a face mask whenever going outside, while also recommending the manufacture of a homemade cloth face mask to those who cannot purchase face masks.[460]
Panama: Panama has made it mandatory to wear a face mask whenever going outside, while also recommending the manufacture of a homemade cloth face mask to those who cannot purchase face masks.[460] Peru: From 7 April 2020, the Peruvian government started distributing free masks after decreeing their mandatory use in the streets to chase away the new coronavirus, said President Martin Vizcarra.[461]
Peru: From 7 April 2020, the Peruvian government started distributing free masks after decreeing their mandatory use in the streets to chase away the new coronavirus, said President Martin Vizcarra.[461] Philippines: From 2 April 2020, the government required all those living in areas under enhanced community quarantine, as well as more relaxed community quarantine levels, to wear face masks.[462] From 15 December 2020, the government also started to mandate the wearing of full face shield aside from face mask.[463] Previously, face shield was required in enclosed public areas and several localities.[464]
Philippines: From 2 April 2020, the government required all those living in areas under enhanced community quarantine, as well as more relaxed community quarantine levels, to wear face masks.[462] From 15 December 2020, the government also started to mandate the wearing of full face shield aside from face mask.[463] Previously, face shield was required in enclosed public areas and several localities.[464] Poland: Since 16 April 2020, covering lips and nose was compulsory before leaving one's house (e.g., disposable mask, cloth mask, or scarf).[465] After 30 May 2020, covering lips and nose was obligatory only on public transport and public indoor areas (e.g. shopping centre, medical facilities, libraries.). Since 10 October 2020 masks are obligatory again in every public place excluding parks, fields, forests, beaches.;[466] such mandate was removed outdoor since 15 May 2021.[467]
Poland: Since 16 April 2020, covering lips and nose was compulsory before leaving one's house (e.g., disposable mask, cloth mask, or scarf).[465] After 30 May 2020, covering lips and nose was obligatory only on public transport and public indoor areas (e.g. shopping centre, medical facilities, libraries.). Since 10 October 2020 masks are obligatory again in every public place excluding parks, fields, forests, beaches.;[466] such mandate was removed outdoor since 15 May 2021.[467] Russia: Khabarovsk has made the wearing of face masks obligatory to fight the spike in respiratory diseases and prevent the spread of the coronavirus.[468]
Russia: Khabarovsk has made the wearing of face masks obligatory to fight the spike in respiratory diseases and prevent the spread of the coronavirus.[468] Rwanda: On 20 April 2020, Cabinet Minister of Health Daniel Ngamije said the latest guidelines require everyone to wear a mask in public, and at home during the lockdown and thereafter.[399]
Rwanda: On 20 April 2020, Cabinet Minister of Health Daniel Ngamije said the latest guidelines require everyone to wear a mask in public, and at home during the lockdown and thereafter.[399] Serbia: Wearing face masks has been required since 29 June 2020 in public indoor places, including public transportation.[469]
Serbia: Wearing face masks has been required since 29 June 2020 in public indoor places, including public transportation.[469] Singapore: Masks were made mandatory from 14 April 2020 in both public transport and all public places, except for people seated in a restaurant or food court with consumption of food and drink. A conviction of this law can lead to a maximum fine of $10,000 and up to one year imprisonment. Subsequent convictions constitute a fine of up to $20,000 and up to five year imprisonment. Prior to that, there was an increase of number of people wearing masks despite being voluntary during COVID-19 pandemic. From 29 March 2022, mask wearing is no longer required outdoors, but is still mandated indoors.
Singapore: Masks were made mandatory from 14 April 2020 in both public transport and all public places, except for people seated in a restaurant or food court with consumption of food and drink. A conviction of this law can lead to a maximum fine of $10,000 and up to one year imprisonment. Subsequent convictions constitute a fine of up to $20,000 and up to five year imprisonment. Prior to that, there was an increase of number of people wearing masks despite being voluntary during COVID-19 pandemic. From 29 March 2022, mask wearing is no longer required outdoors, but is still mandated indoors. Slovakia: Face masks were compulsory in public transport and shops since 15 March 2020.[470] On 25 March 2020, it became forbidden to go out in public without wearing a mask or covering one's nose and mouth.[471] Since 20 May 2020, face masks are no longer mandatory when distance between people is at least five meters.[472]
Slovakia: Face masks were compulsory in public transport and shops since 15 March 2020.[470] On 25 March 2020, it became forbidden to go out in public without wearing a mask or covering one's nose and mouth.[471] Since 20 May 2020, face masks are no longer mandatory when distance between people is at least five meters.[472] Slovenia: From 29 March 2020, wearing a face mask, even one made at home, or equivalents such as scarves that cover the mouth and nose, is mandatory along with protective gloves; the decree stipulates that masks and gloves need to be worn in indoor public spaces.[473] As of 15 October 2020 face masks or equivalent face coverings are required everywhere in public spaces (including outdoors) for any of the statistical regions designated as "red" (more than 140 confirmed infected per 100k population).[474]
Slovenia: From 29 March 2020, wearing a face mask, even one made at home, or equivalents such as scarves that cover the mouth and nose, is mandatory along with protective gloves; the decree stipulates that masks and gloves need to be worn in indoor public spaces.[473] As of 15 October 2020 face masks or equivalent face coverings are required everywhere in public spaces (including outdoors) for any of the statistical regions designated as "red" (more than 140 confirmed infected per 100k population).[474] South Africa: On 10 April 2020, the Minister of Health recommended that the general public use cloth face masks when going out in public (in addition to hand-washing and social distancing).[475] After 1 May 2020, covering one's nose and mouth will be mandatory in public (with a cloth mask, scarf, T-shirt, etc.).[476]
South Africa: On 10 April 2020, the Minister of Health recommended that the general public use cloth face masks when going out in public (in addition to hand-washing and social distancing).[475] After 1 May 2020, covering one's nose and mouth will be mandatory in public (with a cloth mask, scarf, T-shirt, etc.).[476] South Korea: The government implemented a policy of centralized procurement and rationing of face masks, purchasing eighty percent of national production since early March.[477] On 25 May 2020, the Korean government / Central Disaster and Safety Countermeasure Headquarters required everyone to wear masks in all public transport and public places with the surge of COVID-19 cases.[478]
South Korea: The government implemented a policy of centralized procurement and rationing of face masks, purchasing eighty percent of national production since early March.[477] On 25 May 2020, the Korean government / Central Disaster and Safety Countermeasure Headquarters required everyone to wear masks in all public transport and public places with the surge of COVID-19 cases.[478] Spain: Wearing masks has been required since 4 May 2020 while on public transportation, which includes taxis, trains and buses. The government is providing masks to the majority of people riding public transportation, regardless of if they have a mask on.[479][480] On 9 June 2020, the Spanish Ministry of Health and the Ministry of Transport maintains the mandatory nature of masks on public roads, in open air spaces, and in closed spaces for public use[481]
Spain: Wearing masks has been required since 4 May 2020 while on public transportation, which includes taxis, trains and buses. The government is providing masks to the majority of people riding public transportation, regardless of if they have a mask on.[479][480] On 9 June 2020, the Spanish Ministry of Health and the Ministry of Transport maintains the mandatory nature of masks on public roads, in open air spaces, and in closed spaces for public use[481] Sweden: Sweden's Public Health Agency says the scientific evidence does not support public use of face masks, and that public use of face masks would undermine Sweden's COVID-19 response. The government has also warned that wearing them might create a false sense of security, and that public use of masks could do more harm than good.[482][483]
Sweden: Sweden's Public Health Agency says the scientific evidence does not support public use of face masks, and that public use of face masks would undermine Sweden's COVID-19 response. The government has also warned that wearing them might create a false sense of security, and that public use of masks could do more harm than good.[482][483] Taiwan: On 21 January 2020, the government announced a temporary ban on the export of face masks.[484] On 6 February 2020, the government instituted a mask rationing system.[485] The ROC has been producing ten million masks per day since mid-March 2020.[486] On 1 April 2020, passengers on trains and intercity buses were required to wear face masks,[487] unmasked riders facing a fine.[488]
Taiwan: On 21 January 2020, the government announced a temporary ban on the export of face masks.[484] On 6 February 2020, the government instituted a mask rationing system.[485] The ROC has been producing ten million masks per day since mid-March 2020.[486] On 1 April 2020, passengers on trains and intercity buses were required to wear face masks,[487] unmasked riders facing a fine.[488] Turkmenistan: Face masks became mandatory and not wearing one resulted in high fines.
Turkmenistan: Face masks became mandatory and not wearing one resulted in high fines. Turkey: Wearing a face mask in public is compulsory.[489][490]
Turkey: Wearing a face mask in public is compulsory.[489][490] Ukraine: Since 6 April 2020, wearing a face mask is required by the government in public places. In Kyiv, public places were clarified to include parks and streets.[491]
Ukraine: Since 6 April 2020, wearing a face mask is required by the government in public places. In Kyiv, public places were clarified to include parks and streets.[491].svg.png) United Kingdom: Health is a devolved policy in the United Kingdom, resulting in different policies across the four nations:
United Kingdom: Health is a devolved policy in the United Kingdom, resulting in different policies across the four nations:
 England: From 11 May 2020, the Prime Minister of the United Kingdom, Boris Johnson, advised that people wear face coverings in enclosed spaces where 2m social distancing was not possible and when they would come into contact with people who they wouldn't usually meet. On 15 June 2020, wearing a face covering became compulsory on public transport and in healthcare settings. On 24 July 2020, face coverings became compulsory in shops.[492][493] On 8 August the legal requirement to wear a face covering was extended to other indoor venues such as cinemas, restaurants (unless seated to eat or drink) and places of worship.[494] When the majority of Covid restrictions were ultimately lifted on 19 July 2021, face coverings ceased to be mandatory by law in most settings across England, but businesses were able to implement their own policies. The wearing of face masks continued to be compulsory on Transport for London services beyond this date. The mandate was reinstated on 30 November 2021 for public transport and retail outlets, and for "most indoor public places" excluding hospitality venues on 10 December 2021 amid concerns over the omicron variant.[495] It was lifted again on 27 January 2022.[496]
England: From 11 May 2020, the Prime Minister of the United Kingdom, Boris Johnson, advised that people wear face coverings in enclosed spaces where 2m social distancing was not possible and when they would come into contact with people who they wouldn't usually meet. On 15 June 2020, wearing a face covering became compulsory on public transport and in healthcare settings. On 24 July 2020, face coverings became compulsory in shops.[492][493] On 8 August the legal requirement to wear a face covering was extended to other indoor venues such as cinemas, restaurants (unless seated to eat or drink) and places of worship.[494] When the majority of Covid restrictions were ultimately lifted on 19 July 2021, face coverings ceased to be mandatory by law in most settings across England, but businesses were able to implement their own policies. The wearing of face masks continued to be compulsory on Transport for London services beyond this date. The mandate was reinstated on 30 November 2021 for public transport and retail outlets, and for "most indoor public places" excluding hospitality venues on 10 December 2021 amid concerns over the omicron variant.[495] It was lifted again on 27 January 2022.[496]- Northern Ireland: The wearing of face masks on public transport was compulsory from 10 July.[497] A voluntary request to use face masks in retail stores was introduced on 1 August 2020 but Deputy First Minister Michelle O'Neill advised this may become mandatory, if sufficient number of people were not wearing them by 20 August.[498] On 24 May 2021 the requirement to use face coverings was extended to all indoor public areas having already been in place in shops.[499]
 Scotland: On 28 April 2020, the First Minister for Scotland Nicola Sturgeon advised the voluntary use of cloth face masks in enclosed spaces such as shops and public transport (but not generally in public), while noting their limitation.[500] The use of face coverings became compulsory on public transport on 22 June 2020[501] and in shops on 10 July 2020.[502][503] As of 18 January 2021, face coverings were compulsory on public transport, in shops, and most indoor communal spaces in Scotland.[504]
Scotland: On 28 April 2020, the First Minister for Scotland Nicola Sturgeon advised the voluntary use of cloth face masks in enclosed spaces such as shops and public transport (but not generally in public), while noting their limitation.[500] The use of face coverings became compulsory on public transport on 22 June 2020[501] and in shops on 10 July 2020.[502][503] As of 18 January 2021, face coverings were compulsory on public transport, in shops, and most indoor communal spaces in Scotland.[504] Wales: Face masks became compulsory on public transport on Wales on 27 July 2020.[505] In July 2020, First Minister Mark Drakeford has warned people may be turned away from healthcare settings if they refuse to wear a mask when asked.[506] The use of face coverings became mandatory in indoor public areas including shops on 14 September 2020.[507]
Wales: Face masks became compulsory on public transport on Wales on 27 July 2020.[505] In July 2020, First Minister Mark Drakeford has warned people may be turned away from healthcare settings if they refuse to wear a mask when asked.[506] The use of face coverings became mandatory in indoor public areas including shops on 14 September 2020.[507]
 United States: In March 2020, the CDC recommended that if neither respirators nor surgical masks are available, as a last resort, it may be necessary for healthcare workers to use masks that have never been evaluated or approved by NIOSH or homemade masks, though caution should be exercised when considering this option.[508] On 6 April, the CDC recommended the wearing of non-medical cloth face coverings when in public places.[509][510] As of 4 August 34 states and the District of Columbia have implemented health orders requiring the wearing of face coverings in most public spaces.[511][512][513] On May 14, the CDC suggested that vaccinated individuals could enter indoor venues without wearing masks,[514] a number of states have lifted the mandate.[515][516]
United States: In March 2020, the CDC recommended that if neither respirators nor surgical masks are available, as a last resort, it may be necessary for healthcare workers to use masks that have never been evaluated or approved by NIOSH or homemade masks, though caution should be exercised when considering this option.[508] On 6 April, the CDC recommended the wearing of non-medical cloth face coverings when in public places.[509][510] As of 4 August 34 states and the District of Columbia have implemented health orders requiring the wearing of face coverings in most public spaces.[511][512][513] On May 14, the CDC suggested that vaccinated individuals could enter indoor venues without wearing masks,[514] a number of states have lifted the mandate.[515][516] Uzbekistan: Officials made protective masks mandatory in all major cities to prevent the spread of coronavirus. Officials on 22 March said citizens not wearing masks in public in major cities would be fined $22 for the first offense and $67 for repeat offenses.[517]
Uzbekistan: Officials made protective masks mandatory in all major cities to prevent the spread of coronavirus. Officials on 22 March said citizens not wearing masks in public in major cities would be fined $22 for the first offense and $67 for repeat offenses.[517] Venezuela: The government ordered the country's citizens to wear face masks in public in response to the arrival of the novel coronavirus.[518]
Venezuela: The government ordered the country's citizens to wear face masks in public in response to the arrival of the novel coronavirus.[518] Vietnam: Since 16 March 2020, everyone must wear a face mask when going to public places (such as grocery stores, transportation hubs, and public transport).[519]
Vietnam: Since 16 March 2020, everyone must wear a face mask when going to public places (such as grocery stores, transportation hubs, and public transport).[519] Zambia: The government made it mandatory to wear face masks to minimize the spread in the country.[520]
Zambia: The government made it mandatory to wear face masks to minimize the spread in the country.[520]
See also[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Bourouiba L (July 2021). "Fluid Dynamics of Respiratory Infectious Diseases". Annual Review of Biomedical Engineering. 23 (1): 547–577. doi:10.1146/annurev-bioeng-111820-025044. hdl:1721.1/131115. PMID 34255991. S2CID 235823756.
- ↑ 2.0 2.1 Catching, Adam; Capponi, Sara; Te Yeh, Ming; Bianco, Simone; Andino, Raul (6 August 2021). "Examining the interplay between face mask usage, asymptomatic transmission, and social distancing on the spread of COVID-19". Scientific Reports. Nature Portfolio. 11. doi:10.1038/s41598-021-94960-5. Archived from the original on 22 March 2022. Retrieved 23 April 2022.
Masks prevent the spread of droplets and aerosols generated by an infected individual, and when correctly worn surgical masks can reduce viral transmission by 95%. Uninfected individuals wearing a surgical mask are about 85% protected against infection.
- ↑ 3.0 3.1 Talic S, Shah S, Wild H, Gasevic D, Maharaj A, Ademi Z, Li X, Xu W, Mesa-Eguiagaray I, Rostron J, Theodoratou E, Zhang X, Motee A, Liew D, Ilic D (November 2021). "Effectiveness of public health measures in reducing the incidence of covid-19, SARS-CoV-2 transmission, and covid-19 mortality: systematic review and meta-analysis". BMJ. 375: e068302. doi:10.1136/bmj-2021-068302. PMID 34789505.
The results of additional studies that assessed mask wearing ... indicate a reduction in covid-19 incidence, SARS-CoV-2 transmission, and covid-19 mortality. Specifically, a natural experiment across 200 countries showed 45.7% fewer covid-19 related mortality in countries where mask wearing was mandatory. Another natural experiment study in the US reported a 29% reduction in SARS-CoV-2 transmission (measured as the time varying reproductive number Rt) (risk ratio 0.71, 95% confidence interval 0.58 to 0.75) in states where mask wearing was mandatory.A comparative study in the Hong Kong Special Administrative Region reported a statistically significant lower cumulative incidence of covid-19 associated with mask wearing than in selected countries where mask wearing was not mandatory.
- ↑ The Real-World Effectiveness Of Face Masks Against Covid-19 Archived 24 March 2022 at the Wayback Machine by John Drake, director of the Center for the Ecology of Infectious Diseases at the University of Georgia
- ↑ Science Brief: Community Use of Masks to Control the Spread of SARS-CoV-2 Archived 29 November 2021 at the Wayback Machine Experimental and epidemiologic data support community masking to reduce the spread of SARS-CoV-2, including alpha and delta variants, among adults and children. [...] Mask use has been found to be safe and is not associated with clinically significant impacts on respiration or gas exchange under most circumstances, except for intense exercise. The limited available data indicate no clear evidence that masking impairs emotional or language development in children. [I]n combination with other contextual cues, masks are unlikely to produce serious impairments of children’s social interactions. A study of 2-year-old children concluded that they were able to recognize familiar words presented without a mask and when hearing words through opaque masks. Among children with autism spectrum disorders (ASD), interventions including positive reinforcement and coaching caregivers to teach mask wearing have improved participants’ ability to wear a face mask. These findings suggest that even children who may have difficulty wearing a mask can do so effectively through targeted interventions.
- ↑ "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 29 November 2021. Retrieved 15 March 2022.
- ↑ 7.00 7.01 7.02 7.03 7.04 7.05 7.06 7.07 7.08 7.09 7.10 7.11 7.12 Ju JT, Boisvert LN, Zuo YY (June 2021). "Face masks against COVID-19: Standards, efficacy, testing and decontamination methods". Advances in Colloid and Interface Science. 292: 102435. doi:10.1016/j.cis.2021.102435. PMC 8084286. PMID 33971389.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 8.7 Ataei M, Shirazi FM, Nakhaee S, Abdollahi M, Mehrpour O (October 2021). "Assessment of cloth masks ability to limit Covid-19 particles spread: a systematic review". Environmental Science and Pollution Research International. 29 (2): 1645–1676. doi:10.1007/s11356-021-16847-2. PMC 8541808. PMID 34689269.
- ↑ 9.0 9.1 9.2 9.3 Chu DK, Akl EA, Duda S, Solo K, Yaacoub S, Schünemann HJ (June 2020). "Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis". Lancet. 395 (10242): 1973–1987. doi:10.1016/S0140-6736(20)31142-9. PMC 7263814. PMID 32497510.
- ↑ "What Dr. Fauci wants you to know about face masks and staying home as virus spreads". PBS NewsHour. 3 April 2020. Archived from the original on 9 October 2021. Retrieved 1 May 2021.
- ↑ "Face masks and the environment: Preventing the next plastic problem". ScienceDaily. Archived from the original on 10 April 2022. Retrieved 17 February 2022.
- ↑ Center for Devices and Radiological Health (15 September 2021). "N95 Respirators, Surgical Masks, Face Masks, and Barrier Face Coverings". FDA. Archived from the original on 28 November 2021. Retrieved 23 April 2022.
- ↑ CDC (11 February 2020). "Considerations for Wearing Masks". Centers for Disease Control and Prevention. Archived from the original on 8 December 2020. Retrieved 25 January 2021.
- ↑ "Personal Protective Equipments (PPE) -Prerequisites, Rationale and Challenges during COVID 19 Pandemic". ResearchGate. Archived from the original on 12 July 2021. Retrieved 17 February 2021.
- ↑ Lam SC, Suen LK, Cheung TC (August 2020). "Global risk to the community and clinical setting: Flocking of fake masks and protective gears during the COVID-19 pandemic". American Journal of Infection Control. 48 (8): 964–965. doi:10.1016/j.ajic.2020.05.008. PMC 7219383. PMID 32405127.
- ↑ Sankhyan S, Heinselman KN, Ciesielski PN, Barnes T, Himmel ME, Teed H, et al. (2021). "Filtration Performance of Layering Masks and Face Coverings and the Reusability of Cotton Masks after Repeated Washing and Drying". Aerosol and Air Quality Research. 21 (11): 210117. doi:10.4209/aaqr.210117. ISSN 2071-1409. S2CID 237538485. Archived from the original on 24 November 2021. Retrieved 23 April 2022.
- ↑ 17.0 17.1 Zangmeister CD, Radney JG, Vicenzi EP, Weaver JL (July 2020). "Filtration Efficiencies of Nanoscale Aerosol by Cloth Mask Materials Used to Slow the Spread of SARS-CoV-2". ACS Nano. 14 (7): 9188–9200. doi:10.1021/acsnano.0c05025. PMC 7341689. PMID 32584542.
- ↑ 18.0 18.1 18.2 18.3 18.4 18.5 18.6 18.7 Garcia Godoy LR, Jones AE, Anderson TN, Fisher CL, Seeley KM, Beeson EA, et al. (May 2020). "Facial protection for healthcare workers during pandemics: a scoping review". BMJ Global Health. 5 (5): e002553. doi:10.1136/bmjgh-2020-002553. PMC 7228486. PMID 32371574.
- ↑ Konda A, Prakash A, Moss GA, Schmoldt M, Grant GD, Guha S (May 2020). "Aerosol Filtration Efficiency of Common Fabrics Used in Respiratory Cloth Masks". ACS Nano. 14 (5): 6339–6347. doi:10.1021/acsnano.0c03252. PMC 7185834. PMID 32329337.
- ↑ Daoud AK, Hall JK, Petrick H, Strong A, Piggott C (1 January 2021). "The Potential for Cloth Masks to Protect Health Care Clinicians From SARS-CoV-2: A Rapid Review". Annals of Family Medicine. 19 (1): 55–62. doi:10.1370/afm.2640. PMC 7800735. PMID 33431393.
- ↑ Davies A, Thompson KA, Giri K, Kafatos G, Walker J, Bennett A (August 2013). "Testing the efficacy of homemade masks: would they protect in an influenza pandemic?". Disaster Medicine and Public Health Preparedness. 7 (4): 413–418. doi:10.1017/dmp.2013.43. PMC 7108646. PMID 24229526.
- ↑ Aydin O, Emon B, Cheng S, Hong L, Chamorro LP, Saif MT (October 2020). "Performance of fabrics for home-made masks against the spread of COVID-19 through droplets: A quantitative mechanistic study". Extreme Mechanics Letters. 40: 100924. doi:10.1016/j.eml.2020.100924. PMC 7417273. PMID 32835043.
- ↑ 23.0 23.1 23.2 23.3 23.4 "Coronavirus disease (COVID-19) advice for the public: When and how to use masks". World Health Organization. 20 October 2020. Archived from the original on 29 October 2020.
- ↑ 24.0 24.1 Clase CM, Fu EL, Ashur A, Beale RC, Clase IA, Dolovich MB, et al. (October 2020). "Forgotten Technology in the COVID-19 Pandemic: Filtration Properties of Cloth and Cloth Masks-A Narrative Review". Mayo Clinic Proceedings. 95 (10): 2204–2224. doi:10.1016/j.mayocp.2020.07.020. PMC 7834536. PMID 33012350.
- ↑ "Frequent Questions About Hand Hygiene: Handwashing". www.cdc.gov. 14 October 2020. Archived from the original on 9 October 2021. Retrieved 7 November 2020.
- ↑ "How to Safely Wear and Take Off a Cloth Face Covering" (PDF). CDC. Archived (PDF) from the original on 2 November 2021. Retrieved 23 April 2022.
- ↑ "Does a PM 2.5 filter help with coronavirus? - UAB Medicine News - UAB Medicine". www.uabmedicine.org. Archived from the original on 9 October 2021. Retrieved 7 November 2020.
- ↑ 28.0 28.1 "EPA Researchers Test Effectiveness of Face Masks, Disinfection Methods Against COVID-19". 5 April 2021. Archived from the original on 24 February 2022. Retrieved 23 April 2022.
- ↑ 29.0 29.1 29.2 "N95 Respirators and Surgical Masks (Face Masks)". U.S. Food and Drug Administration. 11 March 2020. Archived from the original on 28 March 2020. Retrieved 28 March 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "COVID-19 Q&A with Dr. Roy Kirkpatrick: Wearing masks". Huntsville Doppler. 21 May 2020. Archived from the original on 13 March 2022. Retrieved 13 March 2022.
- ↑ Wei NK (6 May 2019). "What is PM0.3 and Why Is It Important?". Smart Air Filters. Archived from the original on 9 October 2021. Retrieved 23 April 2022.
- ↑ US 5496507, "Method Of Charging Electret Filter Media"
- ↑ "Properties of Different Types of Masks" (PDF). Government of New South Wales Clinical Excellence Commission. February 2020. Archived from the original (PDF) on 31 March 2020.
- ↑ Jung J (17 March 2020). "KAIST Researchers Develop Highly Reusable Mask Filter". KoreaTechToday. Archived from the original on 9 October 2021. Retrieved 23 April 2022.
- ↑ 35.0 35.1 35.2 "Recommended Guidance for Extended Use and Limited Reuse of N95 Filtering Facepiece Respirators in Healthcare Settings". cdc.gov. NIOSH Workplace Safety and Health Topic. CDC. 27 March 2020. Archived from the original on 23 July 2020. Retrieved 23 April 2022.
- ↑ 36.0 36.1 "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 26 July 2020. Retrieved 23 April 2022.
- ↑ "Not Enough Face Masks Are Made In America To Deal With Coronavirus". NPR. 5 March 2020. Archived from the original on 10 November 2021. Retrieved 10 April 2020.
- ↑ "Chinese mask makers use loopholes to speed up regulatory approval". Financial Times. 1 April 2020. Archived from the original on 31 March 2020. Retrieved 10 April 2020.
- ↑ Long Y, Hu T, Liu L, Chen R, Guo Q, Yang L, et al. (May 2020). "Effectiveness of N95 respirators versus surgical masks against influenza: A systematic review and meta-analysis". Journal of Evidence-Based Medicine. 13 (2): 93–101. doi:10.1111/jebm.12381. PMC 7228345. PMID 32167245.
- ↑ Gawn J (2008). "Evaluating the protection afforded by surgical masks against influenza bioaerosols" (PDF). UK's Health and Safety Executive. Archived (PDF) from the original on 3 November 2021. Retrieved 23 April 2022.
- ↑ Robertson P (15 March 2020). "Comparison of Mask Standards, Ratings, and Filtration Effectiveness". Smart Air Filters. Archived from the original on 11 July 2020. Retrieved 23 April 2022.
- ↑ 中华人民共和国医药行业标准:YY 0469–2011 医用外科口罩(Surgical mask) Archived 9 October 2021 at the Wayback Machine (in Chinese)
- ↑ 中华人民共和国医药行业标准:YY/T 0969–2013 一次性使用医用口罩(Single-use medical face mask) Archived 25 February 2021 at the Wayback Machine (in Chinese)
- ↑ Mueller AV, Eden MJ, Oakes JM, Bellini C, Fernandez LA (September 2020). "Quantitative Method for Comparative Assessment of Particle Removal Efficiency of Fabric Masks as Alternatives to Standard Surgical Masks for PPE". Matter. 3 (3): 950–962. doi:10.1016/j.matt.2020.07.006. PMC 7346791. PMID 32838296.
- ↑ 45.0 45.1 Clapp PW, Sickbert-Bennett EE, Samet JM, Berntsen J, Zeman KL, Anderson DJ, et al. (April 2021). "Evaluation of Cloth Masks and Modified Procedure Masks as Personal Protective Equipment for the Public During the COVID-19 Pandemic". JAMA Internal Medicine. 181 (4): 463–469. doi:10.1001/jamainternmed.2020.8168. PMC 7729588. PMID 33300948.
- ↑ Brooks JT, Beezhold DH, Noti JD, Coyle JP, Derk RC, Blachere FM, Lindsley WG (February 2021). "Maximizing Fit for Cloth and Medical Procedure Masks to Improve Performance and Reduce SARS-CoV-2 Transmission and Exposure, 2021". MMWR. Morbidity and Mortality Weekly Report. 70 (7): 254–257. doi:10.15585/mmwr.mm7007e1. PMC 7891692. PMID 33600386.
- ↑ Cavalcanti G, Cocciole C, Cole C, Forgues A, Jaqua V, Jones-Davis D, Merlo S (2021). Design, Make, Protect: A report on the Open Source Maker and Manufacturer Response to the COVID-19 PPE Crisis (PDF). Open Source Medical Supplies & Nation of Makers. pp. 22, 46. Archived (PDF) from the original on 9 October 2021. Retrieved 17 June 2021.
- ↑ "NIOSH-Approved N95 Particulate Filtering Facepiece Respirators – A Suppliers List". U.S. National Institute for Occupational Safety and Health. 19 March 2020. Archived from the original on 16 July 2020. Retrieved 27 March 2020.
- ↑ "Respirator Trusted-Source: Selection FAQs". U.S. National Institute for Occupational Safety and Health. 12 March 2020. Archived from the original on 15 July 2020. Retrieved 28 March 2020.
- ↑ 51.0 51.1 51.2 Zie J (19 March 2020). "World Depends on China for Face Masks But Can Country Deliver?". Voice of America. Archived from the original on 25 July 2020. Retrieved 23 April 2022.
- ↑ Feng E (16 March 2020). "COVID-19 Has Caused A Shortage Of Face Masks. But They're Surprisingly Hard To Make". NPR. Archived from the original on 6 July 2020. Retrieved 23 April 2022.
- ↑ "Comparison of FFP2, KN95, and N95 and Other Filtering Facepiece Respirator Classes" (PDF). 3M Technical Data Bulletin. 1 January 2020. Archived (PDF) from the original on 14 April 2020. Retrieved 28 March 2020.
- ↑ "Strategies for Optimizing the Supply of N95 Respirators: Crisis/Alternate Strategies". U.S. Centers for Disease Control and Prevention. 17 March 2020. Archived from the original on 25 May 2020. Retrieved 28 March 2020.
- ↑ 55.0 55.1 Patel RB, Skaria SD, Mansour MM, Smaldone GC (July 2016). "Respiratory source control using a surgical mask: An in vitro study". Journal of Occupational and Environmental Hygiene. 13 (7): 569–576. doi:10.1080/15459624.2015.1043050. PMC 4873718. PMID 26225807.
- ↑ "Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings". Centers for Disease Control and Prevention (CDC). 18 May 2020. Archived from the original on 23 July 2020. Retrieved 8 June 2020.
- ↑ Mills S (10 April 2020). "Researchers looking at innovative ways to sterilize single-use masks". Canadian Broadcasting Corporation. Archived from the original on 9 October 2021. Retrieved 23 April 2022.
- ↑ 58.0 58.1 58.2 "Considerations for Wearing Masks". Centers for Disease Control and Prevention. 7 August 2020. Archived from the original on 7 August 2020.
- ↑ Lindsley WG, Blachere FM, Law BF, Beezhold DH, Noti JD (7 January 2021). "Efficacy of face masks, neck gaiters and face shields for reducing the expulsion of simulated cough-generated aerosols". Aerosol Science and Technology. 55 (4): 449–457. Bibcode:2021AerST..55..449L. doi:10.1080/02786826.2020.1862409.
- ↑ Lindsley WG, Noti JD, Blachere FM, Szalajda JV, Beezhold DH (3 August 2014). "Efficacy of face shields against cough aerosol droplets from a cough simulator". Journal of Occupational and Environmental Hygiene. 11 (8): 509–518. doi:10.1080/15459624.2013.877591. PMC 4734356. PMID 24467190. Cited in Garcia Godoy LR, Jones AE, Anderson TN, Fisher CL, Seeley KM, Beeson EA, et al. (May 2020). "Facial protection for healthcare workers during pandemics: a scoping review". BMJ Global Health. 5 (5): e002553. doi:10.1136/bmjgh-2020-002553. PMC 7228486. PMID 32371574.
- ↑ 61.0 61.1 61.2 "Elastomeric Respirators: Strategies During Conventional and Surge Demand Situations". Centers for Disease Control and Prevention. 13 October 2020. Archived from the original on 16 October 2020.
- ↑ 62.0 62.1 Chiang J, Hanna A, Lebowitz D, Ganti L (July 2020). "Elastomeric respirators are safer and more sustainable alternatives to disposable N95 masks during the coronavirus outbreak". International Journal of Emergency Medicine. 13 (1): 39. doi:10.1186/s12245-020-00296-8. PMC 7369563. PMID 32689926.
- ↑ 63.0 63.1 Howard BE (July 2020). "High-Risk Aerosol-Generating Procedures in COVID-19: Respiratory Protective Equipment Considerations". Otolaryngology–Head and Neck Surgery. 163 (1): 98–103. doi:10.1177/0194599820927335. PMID 32396451.
- ↑ Mick P, Murphy R (May 2020). "Aerosol-generating otolaryngology procedures and the need for enhanced PPE during the COVID-19 pandemic: a literature review". Journal of Otolaryngology - Head & Neck Surgery. 49 (1): 29. doi:10.1186/s40463-020-00424-7. PMC 7212733. PMID 32393346.
- ↑ Licina A, Silvers A, Stuart RL (August 2020). "Use of powered air-purifying respirator (PAPR) by healthcare workers for preventing highly infectious viral diseases-a systematic review of evidence". Systematic Reviews. 9 (1): 173. doi:10.1186/s13643-020-01431-5. PMC 7414632. PMID 32771035.
- ↑ Staymates M (November 2020). "Flow visualization of an N95 respirator with and without an exhalation valve using schlieren imaging and light scattering". Physics of Fluids. 32 (11): 111703. Bibcode:2020PhFl...32k1703S. doi:10.1063/5.0031996. PMC 7684679. PMID 33244212.
 Available under CC BY 4.0 Archived 16 October 2017 at the Wayback Machine.
Available under CC BY 4.0 Archived 16 October 2017 at the Wayback Machine.
- ↑ "Filtering Facepiece Respirators with an Exhalation Valve: Measurements of Filtration Efficiency to Evaluate Their Potential for Source Control". NIOSH Publications. 9 December 2020. doi:10.26616/NIOSHPUB2021107. Archived from the original on 30 October 2021. Retrieved 23 April 2022.
- ↑ "Face shields, masks with valves ineffective against COVID-19 spread: study". phys.org. Archived from the original on 17 November 2021. Retrieved 8 October 2020.
- ↑ Verma S, Dhanak M, Frankenfield J (September 2020). "Visualizing droplet dispersal for face shields and masks with exhalation valves". Physics of Fluids. 32 (9): 091701. arXiv:2008.00125. Bibcode:2020PhFl...32i1701V. doi:10.1063/5.0022968. PMC 7497716. PMID 32952381.
- ↑ 70.0 70.1 70.2 "Using face masks in the community - Reducing COVID-19 transmission from potentially asymptomatic or pre-symptomatic people through the use of face masks". European Centre for Disease Prevention and Control. 8 April 2020. Archived from the original on 8 April 2020.
- ↑ 71.0 71.1 71.2 71.3 "Advice on the use of masks in the context of COVID-19". World Health Organization. 5 June 2020. Archived from the original on 27 November 2021. Retrieved 23 April 2022.
- ↑ Ting V (4 April 2020). "To mask or not to mask: WHO makes U-turn while US, Singapore abandon pandemic advice and tell citizens to start wearing masks". South China Morning Post. Archived from the original on 18 May 2020. Retrieved 23 April 2022.
- ↑ Wong-Shing K. "N95, KN95, KF94: The best masks to help avoid COVID now". CNET. Archived from the original on 12 January 2022. Retrieved 13 January 2022.
- ↑ "Cloth masks can help stop the spread of COVID-19, save lives and restore jobs". #Masks4All. Archived from the original on 25 September 2020. Retrieved 27 September 2020.
The leading disease experts and governments representing 95% of the world's population (including the U.S. CDC) agree with the science and require/recommend masks because cloth (non-medical) masks are shown to limit the spread of COVID-19.
- ↑ Advice on the use of masks in the community, during home care and in health care settings in the context of the novel coronavirus (2019-nCoV) outbreak: interim guidance, 29 January 2020 (Report). World Health Organization. 29 January 2020. hdl:10665/330987.
- ↑ Advice on the use of masks in the community, during home care, and in health care settings in the context of COVID-19: interim guidance, 19 March 2020 (Report). World Health Organization. 19 March 2020. hdl:10665/331493.
- ↑ 77.0 77.1 Advice on the use of masks in the context of COVID-19: interim guidance, 6 April 2020 (Report). World Health Organization. 6 April 2020. hdl:10665/331693.
- ↑ Keshtkar-Jahromi M, Sulkowski M, Holakouie-Naieni K (June 2020). "Public Masking: An Urgent Need to Revise Global Policies to Protect against COVID-19". The American Journal of Tropical Medicine and Hygiene. 102 (6): 1160–1161. doi:10.4269/ajtmh.20-0305. PMC 7253086. PMID 32323645.
- ↑ 79.0 79.1 79.2 Winn P (1 April 2020). "Will the US ever mimic Asia's culture of 'universal masking'?". Public Radio International. Archived from the original on 9 October 2021. Retrieved 23 April 2022.
- ↑ 80.0 80.1 80.2 Tufekci Z (17 March 2020). "Why Telling People They Don't Need Masks Backfired". The New York Times. Archived from the original on 11 March 2021. Retrieved 12 April 2020.
- ↑ Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ (May 2020). "Rational use of face masks in the COVID-19 pandemic". The Lancet. Respiratory Medicine. 8 (5): 434–436. doi:10.1016/S2213-2600(20)30134-X. PMC 7118603. PMID 32203710.
- ↑ Flaskerud JH (September 2020). "Masks, Politics, Culture and Health". Issues in Mental Health Nursing. 41 (9): 846–849. doi:10.1080/01612840.2020.1779883. PMID 32644832.
- ↑ Mantzari E, Rubin GJ, Marteau TM (July 2020). "Is risk compensation threatening public health in the covid-19 pandemic?". BMJ. 370: m2913. doi:10.1136/bmj.m2913. PMID 32713835.
- ↑ Hunt K (27 July 2020). "Face mask wearers don't get lax about washing hands, study suggests". CNN. Archived from the original on 9 October 2021. Retrieved 23 April 2022.
- ↑ Feuer W, Higgins-Dunn N (8 June 2020). "Asymptomatic spread of coronavirus is 'very rare', WHO says". CNBC. Archived from the original on 26 November 2021. Retrieved 23 April 2022.
- ↑ "Q&A: Masks and COVID-19". World Health Organization. 7 June 2020. Archived from the original on 27 July 2020. For more details on fabrics, see also "Advice on the use of masks in the context of COVID-19". World Health Organization. 5 June 2020. Archived from the original on 27 November 2021. Retrieved 23 April 2022.
- ↑ 87.0 87.1 87.2 87.3 "Advice on the use of masks for children in the community in the context of COVID-19". World Health Organization. 21 August 2020. Archived from the original on 18 November 2021. Retrieved 23 April 2022. For an overview, see "Q&A: Children and masks related to COVID-19". World Health Organization. 21 August 2020. Archived from the original on 7 November 2021. Retrieved 23 April 2022.
- ↑ "Q&A: Masks and COVID-19". World Health Organization. 7 June 2020. Archived from the original on 27 July 2020.
- ↑ "Use of cloth face coverings to help slow the spread of COVID-19". Centers for Disease Control and Prevention. 3 April 2020. Archived from the original on 9 October 2021. Retrieved 23 April 2022.
- ↑ López C. "Celebrities like Gwyneth Paltrow and Kate Hudson were criticized for wearing face masks early in the pandemic. Here's what changed". Business Insider. Archived from the original on 12 July 2021. Retrieved 23 April 2022.
- ↑ "Transcript for CDC Telebriefing: CDC Update on Novel Coronavirus". Centers for Disease Control and Prevention. 12 February 2020. Archived from the original on 8 November 2021. Retrieved 23 April 2022.
- ↑ "Fact check: Medical discharge document includes outdated CDC guidance on face masks". Reuters. 3 July 2020. Archived from the original on 9 October 2021. Retrieved 23 April 2022.
- ↑ Fisher KA, Barile JP, Guerin RJ, Vanden Esschert KL, Jeffers A, Tian LH, et al. (July 2020). "Factors Associated with Cloth Face Covering Use Among Adults During the COVID-19 Pandemic - United States, April and May 2020". MMWR. Morbidity and Mortality Weekly Report. 69 (28): 933–937. doi:10.15585/mmwr.mm6928e3. PMID 32673303. S2CID 220606747.
- ↑ 94.0 94.1 Jingnan H (10 April 2020). "Why There Are So Many Different Guidelines For Face Masks For The Public". NPR. Archived from the original on 12 March 2021. Retrieved 23 April 2022.
- ↑ Mills R (29 July 2020). "CDC director: Face masks "our most powerful tool" to fight COVID-19". 102.3 KRMG. Archived from the original on 9 October 2021. Retrieved 23 April 2022.
- ↑ Brooks JT, Butler JC, Redfield RR (August 2020). "Universal Masking to Prevent SARS-CoV-2 Transmission-The Time Is Now". JAMA. 324 (7): 635–637. doi:10.1001/jama.2020.13107. PMC 8607819. PMID 32663243.
- ↑ Henry TA (17 July 2020). "CDC's Dr. Redfield: This is why everyone should be wearing masks". American Medical Association. Archived from the original on 19 November 2020. Retrieved 23 April 2022.
- ↑ "Personal Protective Equipment: Questions and Answers". Centers for Disease Control and Prevention. 8 August 2020. Archived from the original on 10 August 2020.
- ↑ 99.0 99.1 "Considerations for wearing cloth face coverings : help slow the spread of COVID-19". Centers for Disease Control and Prevention. 28 June 2020. Archived from the original on 9 October 2021. Retrieved 23 April 2022.
- ↑ Miller SG (13 August 2020). "Does your mask have a valve on it? It won't stop the spread of coronavirus, CDC says". NBC News. Archived from the original on 9 October 2021. Retrieved 23 April 2022.
- ↑ 101.0 101.1 101.2 101.3 "Scientific Brief: Community Use of Cloth Masks to Control the Spread of SARS-CoV-2". Centers for Disease Control and Prevention. 10 November 2020. Archived from the original on 10 November 2020. Retrieved 23 April 2022.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Interim Infection Prevention and Control Recommendations for Healthcare Personnel During the Coronavirus Disease 2019 (COVID-19) Pandemic". Centers for Disease Control and Prevention. 15 July 2020. Archived from the original on 30 July 2020.
- ↑ "Strategies for Optimizing the Supply of N95 Respirators". Centers for Disease Control and Prevention. 28 June 2020. Archived from the original on 28 July 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "When You've Been Fully Vaccinated". Centers for Disease Control and Prevention. 27 July 2021. Archived from the original on 28 July 2021.
- ↑ Aubrey A (27 July 2021). "CDC Urges Vaccinated People To Mask Up Indoors In Places With High Virus Transmission". NPR. Archived from the original on 19 November 2021. Retrieved 23 April 2022.
- ↑ "Interim Public Health Recommendations for Fully Vaccinated People". Centers for Disease Control and Prevention. 13 May 2021. Archived from the original on 14 May 2021.
- ↑ Noguchi Y (20 May 2021). "The CDC Is Gambling On Relaxed Mask Rules To Get More People Vaccinated". NPR. Archived from the original on 21 November 2021. Retrieved 23 April 2022.
- ↑ Bosman J, Mervosh S (18 May 2021). "New Honor System on Masks: 'Am I to Trust These People?'". The New York Times. Archived from the original on 29 October 2021. Retrieved 23 April 2022.
- ↑ Iati M (15 May 2021). "The new mask guidance relies on an honor system. Do we trust each other enough to make it work?". The Washington Post. Archived from the original on 3 August 2021. Retrieved 23 April 2022.
- ↑ Mandavilli, Apoorva (25 February 2022). "The C.D.C. releases new guidance that will allow localities to ease masking and social distancing". The New York Times. ISSN 0362-4331. Archived from the original on 28 February 2022. Retrieved 28 February 2022.
- ↑ "CDC says Americans can now go unmasked in many parts of the country". NPR.org. Archived from the original on 1 March 2022. Retrieved 28 February 2022.
- ↑ Wetsman N (3 April 2020). "Masks may be good, but the messaging around them has been very bad". The Verge. Archived from the original on 13 October 2021. Retrieved 23 April 2022.
- ↑ Jankowicz M (1 June 2020). "Fauci said US government held off promoting face masks because it knew shortages were so bad that even doctors couldn't get enough". Business Insider. Archived from the original on 16 September 2020. Retrieved 23 April 2022.
- ↑ Cohen J (27 March 2020). "Not wearing masks to protect against coronavirus is a 'big mistake'". Science. Archived from the original on 28 March 2020. Retrieved 23 April 2022.
- ↑ "Mandatory mask-wearing now the norm in Europe as COVID-19 cases rise". euronews. 24 July 2020. Archived from the original on 7 May 2021. Retrieved 23 April 2022.
- ↑ 116.0 116.1 "Norway Makes First Face Mask Recommendation Since Pandemic Began". VOA News. 14 August 2020. Archived from the original on 2 July 2021. Retrieved 23 April 2022.
- ↑ Vogel G (6 October 2020). "'It's been so, so surreal.' Critics of Sweden's lax pandemic policies face fierce backlash". Science. doi:10.1126/science.abf1247. S2CID 225148153.
- ↑ "Using face masks in the community: first update - Effectiveness in reducing transmission of COVID-19". European Centre for Disease Prevention and Control. 15 February 2021. Archived from the original on 17 February 2021.
- ↑ "Hoe iets 'wat geen bescherming biedt' toch landelijk geadviseerd werd" [How something 'that offers no protection' was nevertheless advised nationally]. nos.nl (in Nederlands). Archived from the original on 12 July 2021. Retrieved 24 February 2021.
- ↑ "Face Masks to Be Compulsory on Public Transport in the Netherlands". Archived from the original on 19 July 2021. Retrieved 23 April 2022.
- ↑ "Why are the Nordic countries still not recommending face masks?". The Local dk. 30 July 2020. Archived from the original on 26 January 2021. Retrieved 23 April 2022.
- ↑ Stoltenberg C (June 2020), "Should individuals in the community without respiratory symptoms wear facemasks to reduce the spread of COVID-19? – a rapid review" (PDF), Norwegian Institute of Public Health, archived (PDF) from the original on 8 November 2021, retrieved 23 April 2022
- ↑ "Denmark Recommends Face Masks On Public Transport". Barron's. 31 July 2020. Archived from the original on 2 November 2020. Retrieved 23 April 2022.
- ↑ "No country for face masks: Nordics brush off mouth covers". medicalxpress. 30 July 2020. Archived from the original on 2 November 2020. Retrieved 23 April 2022.
- ↑ 125.0 125.1 "The Copenhagen Post". 23 October 2020. Archived from the original on 13 April 2019. Retrieved 23 April 2022.
- ↑ "Norwegian municipalities introduce local coronavirus rules: Here's what applies in your area". 2 October 2020. Archived from the original on 3 November 2021. Retrieved 23 April 2022.
- ↑ "Tegnells vändning: Lämpligt med munskydd (om man är nära varandra)". Breakit (in svenska). Archived from the original on 25 November 2020. Retrieved 13 May 2021.
- ↑ Lönnroth V (25 November 2020). "Tegnell: Då ska du bära munskydd på jobbet". gp.se (in svenska). Archived from the original on 12 July 2021. Retrieved 13 May 2021.
- ↑ "Sweden does U-turn on face masks to fight virus". France 24. 18 December 2020. Archived from the original on 14 April 2021. Retrieved 23 April 2022.
- ↑ "Munskydd i kollektivtrafiken från den 7 januari". Folkhalsomyndigheten. 30 December 2020. Archived from the original on 9 November 2021. Retrieved 23 April 2022.
- ↑ "Statsminister Löfven besökte galleria fyra dagar före jul". Archived from the original on 30 January 2021. Retrieved 23 April 2022.
- ↑ Razooq N (22 January 2021). "Hälften av resenärerna använder munskydd under rusningstid enligt SL". SVT Nyheter. Archived from the original on 8 March 2021. Retrieved 23 April 2022.
- ↑ Pan E, Lindberg J (28 January 2021). "FHM:s generaldirektör åkte kollektivtrafik utan munskydd: "Genant"". SVT Nyheter (in svenska). Archived from the original on 24 June 2021. Retrieved 23 April 2022.
- ↑ "Nyheter24 avslöjar: Här åker Anders Tegnell tåg i rusningstrafik – utan munskydd". 4 February 2021. Archived from the original on 15 February 2021. Retrieved 23 April 2022.
- ↑ Tang JW, Nicolle AD, Pantelic J, Jiang M, Sekhr C, Cheong DK, Tham KW (22 June 2011). "Qualitative real-time schlieren and shadowgraph imaging of human exhaled airflows: an aid to aerosol infection control". PLOS ONE. 6 (6): e21392. Bibcode:2011PLoSO...621392T. doi:10.1371/journal.pone.0021392. PMC 3120871. PMID 21731730.
- ↑ Verma S, Dhanak M, Frankenfield J (June 2020). "Visualizing the effectiveness of face masks in obstructing respiratory jets". Physics of Fluids. 32 (6): 061708. Bibcode:2020PhFl...32f1708V. doi:10.1063/5.0016018. PMC 7327717. PMID 32624649.
- ↑ Prather KA, Wang CC, Schooley RT (June 2020). "Reducing transmission of SARS-CoV-2". Science. 368 (6498): 1422–1424. Bibcode:2020Sci...368.1422P. doi:10.1126/science.abc6197. PMID 32461212.
- ↑ 138.0 138.1 138.2 138.3 138.4 "Why healthy Chinese wearing face masks outdoors?". NHC.gov.cn. National Health Commission. 23 March 2020. Archived from the original on 10 April 2020. Retrieved 12 April 2020.
- ↑ 139.0 139.1 Cheng KK, Lam TH, Leung CC (April 2020). "Wearing face masks in the community during the COVID-19 pandemic: altruism and solidarity". Lancet: S0140673620309181. doi:10.1016/S0140-6736(20)30918-1. PMC 7162638. PMID 32305074.
- ↑ 140.0 140.1 140.2 "Scientific Brief: Community Use of Cloth Masks to Control the Spread of SARS-CoV-2". Centers for Disease Control and Prevention. 10 November 2020. Archived from the original on 10 November 2020. Retrieved 23 April 2022.
- ↑ Li I, Zuoyan Z (10 March 2020). "Q&A with HK microbiologist Yuen Kwok-yung who helped confirm coronavirus' human spread". The Straits Times. Archived from the original on 23 October 2021. Retrieved 23 April 2022.
- ↑ To KK, Tsang OT, Yip CC, Chan KH, Wu TC, Chan JM, et al. (July 2020). "Consistent Detection of 2019 Novel Coronavirus in Saliva". Clinical Infectious Diseases. Oxford University Press. 71 (15): 841–843. doi:10.1093/cid/ciaa149. PMC 7108139. PMID 32047895.
- ↑ Gandhi M (23 June 2020). "Can people spread the coronavirus if they don't have symptoms? Five questions answered about asymptomatic COVID-19". The Conversation. Archived from the original on 17 November 2021. Retrieved 23 April 2022.
- ↑ Hou YJ, Okuda K, Edwards CE, Martinez DR, Asakura T, Dinnon KH, et al. (July 2020). "SARS-CoV-2 Reverse Genetics Reveals a Variable Infection Gradient in the Respiratory Tract". Cell. 182 (2): 429–446.e14. doi:10.1016/j.cell.2020.05.042. PMC 7250779. PMID 32526206.
- ↑ 145.0 145.1 145.2 Gandhi M, Beyrer C, Goosby E (October 2020). "Masks Do More Than Protect Others During COVID-19: Reducing the Inoculum of SARS-CoV-2 to Protect the Wearer". Journal of General Internal Medicine. 35 (10): 3063–3066. doi:10.1007/s11606-020-06067-8. PMC 7393808. PMID 32737790.
- ↑ Greenhalgh T, Schmid MB, Czypionka T, Bassler D, Gruer L (April 2020). "Face masks for the public during the covid-19 crisis". BMJ. 369: m1435. doi:10.1136/bmj.m1435. PMID 32273267.
- ↑ Javid, B., M. P. Weekes, and N. J. Matheson. 2020. 'Covid-19: should the public wear face masks?', BMJ, 369: m1442. PMID 32273278
- ↑ Clase, C.M., R.C.L. Beale, M.B. Dolovich, E.L.F. Fu, M.J. Jardine, M. Joseph, J.F.E. Mann, R. Pecoits-Filho, W. C. Winkelmayer, and J. J. Carrero. 2020. 'Cloth masks may prevent transmission of COVID-19: an evidence-based, risk-based approach', Accessed 18 July 2020. PMID 32441991
- ↑ Setti L, Passarini F, De Gennaro G, Barbieri P, Perrone MG, Borelli M, et al. (April 2020). "Airborne Transmission Route of COVID-19: Why 2 Meters/6 Feet of Inter-Personal Distance Could Not Be Enough". International Journal of Environmental Research and Public Health. 17 (8): 2932. doi:10.3390/ijerph17082932. PMC 7215485. PMID 32340347.
- ↑ 150.0 150.1 Leung CC, Cheng KK, Lam TH, Migliori GB (June 2020). "Mask wearing to complement social distancing and save lives during COVID-19". The International Journal of Tuberculosis and Lung Disease. 24 (6): 556–558. doi:10.5588/ijtld.20.0244. PMID 32553007. S2CID 219967740.
- ↑ "How to avoid touching your face so much". BBC News. 18 March 2020. Archived from the original on 8 May 2021. Retrieved 23 April 2022.
- ↑ Chan KH, Yuen KY (August 2020). "COVID-19 epidemic: disentangling the re-emerging controversy about medical facemasks from an epidemiological perspective". International Journal of Epidemiology. 49 (4): 1063–1066. doi:10.1093/ije/dyaa044. PMC 7184463. PMID 32232402.
- ↑ Moriyama M, Hugentobler WJ, Iwasaki A (September 2020). "Seasonality of Respiratory Viral Infections". Annual Review of Virology. 7 (1): 83–101. doi:10.1146/annurev-virology-012420-022445. PMID 32196426.
- ↑ Chan NC, Li K, Hirsh J (December 2020). "Peripheral Oxygen Saturation in Older Persons Wearing Nonmedical Face Masks in Community Settings". JAMA. 324 (22): 2323–2324. doi:10.1001/jama.2020.21905. PMC 7600049. PMID 33125030.
- ↑ Escandón K, Rasmussen AL, Bogoch II, Murray EJ, Escandón K, Popescu SV, Kindrachuk J (July 2021). "COVID-19 false dichotomies and a comprehensive review of the evidence regarding public health, COVID-19 symptomatology, SARS-CoV-2 transmission, mask wearing, and reinfection". BMC Infect Dis (Review). 21 (1): 710. doi:10.1186/s12879-021-06357-4. PMC 8314268. PMID 34315427.
- ↑ Sharma SK, Mishra M, Mudgal SK (2020). "Efficacy of cloth face mask in prevention of novel coronavirus infection transmission: A systematic review and meta-analysis". Journal of Education and Health Promotion. 9: 192. doi:10.4103/jehp.jehp_533_20. PMC 7497125. PMID 33015206.
- ↑ 157.0 157.1 Nanda A, Hung I, Kwong A, Man VC, Roy P, Davies L, Douek M (May 2021). "Efficacy of surgical masks or cloth masks in the prevention of viral transmission: Systematic review, meta-analysis, and proposal for future trial". Journal of Evidence-Based Medicine. 14 (2): 97–111. doi:10.1111/jebm.12424. PMC 8014575. PMID 33565274.
- ↑ Wang Y, Tian H, Zhang L, Zhang M, Guo D, Wu W, et al. (May 2020). "Reduction of secondary transmission of SARS-CoV-2 in households by face mask use, disinfection and social distancing: a cohort study in Beijing, China". BMJ Global Health. 5 (5): e002794. doi:10.1136/bmjgh-2020-002794. PMC 7264640. PMID 32467353. Cited in "Scientific Brief: Community Use of Cloth Masks to Control the Spread of SARS-CoV-2". Centers for Disease Control and Prevention. 10 November 2020. Archived from the original on 10 November 2020. Retrieved 23 April 2022.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Doung-Ngern P, Suphanchaimat R, Panjangampatthana A, Janekrongtham C, Ruampoom D, Daochaeng N, et al. (November 2020). "Case-Control Study of Use of Personal Protective Measures and Risk for SARS-CoV 2 Infection, Thailand". Emerging Infectious Diseases. 26 (11): 2607–2616. doi:10.3201/eid2611.203003. PMC 7588529. PMID 32931726. Cited in "Scientific Brief: Community Use of Cloth Masks to Control the Spread of SARS-CoV-2". Centers for Disease Control and Prevention. 10 November 2020. Archived from the original on 10 November 2020. Retrieved 23 April 2022.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Lio, Chon Fu; Cheong, Hou Hon; Lei, Chin Ion; Lo, Iek Long; Yao, Lan; Lam, Chong; Leong, Iek Hou (December 2021). "Effectiveness of personal protective health behaviour against COVID-19". BMC Public Health. 21 (1): 827. doi:10.1186/s12889-021-10680-5.
- ↑ Hendrix MJ, Walde C, Findley K, Trotman R (July 2020). "Absence of Apparent Transmission of SARS-CoV-2 from Two Stylists After Exposure at a Hair Salon with a Universal Face Covering Policy - Springfield, Missouri, May 2020". MMWR. Morbidity and Mortality Weekly Report. 69 (28): 930–932. doi:10.15585/mmwr.mm6928e2. PMID 32673300.
- ↑ Payne DC, Smith-Jeffcoat SE, Nowak G, Chukwuma U, Geibe JR, Hawkins RJ, et al. (June 2020). "SARS-CoV-2 Infections and Serologic Responses from a Sample of U.S. Navy Service Members - USS Theodore Roosevelt, April 2020". MMWR. Morbidity and Mortality Weekly Report. 69 (23): 714–721. doi:10.15585/mmwr.mm6923e4. PMC 7315794. PMID 32525850. Cited in "Scientific Brief: Community Use of Cloth Masks to Control the Spread of SARS-CoV-2". Centers for Disease Control and Prevention. 10 November 2020. Archived from the original on 10 November 2020. Retrieved 23 April 2022.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Schwartz KL, Murti M, Finkelstein M, Leis JA, Fitzgerald-Husek A, Bourns L, et al. (April 2020). "Lack of COVID-19 transmission on an international flight". CMAJ. 192 (15): E410. doi:10.1503/cmaj.75015. PMC 7162437. PMID 32392504. Freedman DO, Wilder-Smith A (December 2020). "In-flight transmission of SARS-CoV-2: a review of the attack rates and available data on the efficacy of face masks". Journal of Travel Medicine. 27 (8): taaa178. doi:10.1093/jtm/taaa178. PMC 7543400. PMID 32975554. Cited in "Scientific Brief: Community Use of Cloth Masks to Control the Spread of SARS-CoV-2". Centers for Disease Control and Prevention. 10 November 2020. Archived from the original on 10 November 2020. Retrieved 23 April 2022.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ Adenaiye OO, Lai J, de Mesquita PJ, Hong F, Youssefi S, German J, et al. (September 2021). "Infectious SARS-CoV-2 in Exhaled Aerosols and Efficacy of Masks During Early Mild Infection". Clinical Infectious Diseases: 2021.08.13.21261989. doi:10.1101/2021.08.13.21261989. PMC 8522431. PMID 34519774. S2CID 236994796.
- ↑ "An upper bound on one-to-one exposure to infectious human respiratory particles". PNAS. 7 December 2021. Archived from the original on 11 December 2021. Retrieved 11 December 2021.
- ↑ "N95, KN95 masks provide best protection against covid, CDC study shows". The Washington Post. 4 February 2022. Archived from the original on 5 February 2022. Retrieved 5 February 2022.
- ↑ "Effectiveness of Face Mask or Respirator Use in Indoor Public Settings for Prevention of SARS-CoV-2 Infection — California, February–December 2021". CDC. 4 February 2022. Archived from the original on 4 February 2022. Retrieved 5 February 2022.
- ↑ "Face masks slow spread of COVID-19; types of masks, length of use matter". phys.org. Archived from the original on 23 October 2021. Retrieved 9 December 2020.
- ↑ Kumar S, Lee HP (November 2020). "The perspective of fluid flow behavior of respiratory droplets and aerosols through the facemasks in context of SARS-CoV-2". Physics of Fluids. 32 (11): 111301. arXiv:2010.06385. Bibcode:2020PhFl...32k1301K. doi:10.1063/5.0029767. PMC 7713871. PMID 33281434.
- ↑ Willis K. "If you haven't been double-masking, new CDC study shows why you should". The Atlanta Journal-Constitution. Archived from the original on 15 July 2021. Retrieved 23 April 2022.
- ↑ 171.0 171.1 "How to Wear Masks". Centers for Disease Control and Prevention. 7 August 2020. Archived from the original on 27 September 2020. Retrieved 28 September 2020.
- ↑ Parker-Pope T (8 April 2020). "How NOT to Wear a Mask". The New York Times. Archived from the original on 26 October 2021. Retrieved 23 April 2022.
- ↑ Malnick E (20 June 2020). "Commuters are wearing masks incorrectly". The Daily Telegraph. Archived from the original on 15 December 2020. Retrieved 23 April 2022.
- ↑ de Courten B, de Courten M, Apostolopoulos V (12 May 2020). "Are you wearing gloves or a mask to the shops? You might be doing it wrong". The Conversation. Archived from the original on 27 August 2021. Retrieved 23 April 2022.
- ↑ Lai J (18 May 2020). "All the ways you're wearing your coronavirus face mask wrong and how to do it properly". Inquirer. Archived from the original on 4 May 2021. Retrieved 23 April 2022.
- ↑ 176.0 176.1 176.2 Cuda A (1 July 2020). "Health experts: COVID masks are only effective if worn properly". Connecticut Post. Archived from the original on 10 July 2021. Retrieved 23 April 2022.
- ↑ Breen K (29 September 2020). "Coronavirus face coverings under the nose equivalent to 'not wearing a mask': experts". Global News. Archived from the original on 22 August 2021. Retrieved 23 April 2022.
- ↑ 谢斌 张纯 (21 January 2020). "一罩难求:南都民调实测走访发现,线上线下口罩基本卖脱销". 南方都市报. Archived from the original on 2 May 2020. Retrieved 21 January 2020.
- ↑ 徐榆涵 (23 January 2020). "全球各地瘋搶口罩 專家:不必買N95". 聯合報. Archived from the original on 25 January 2020. Retrieved 25 January 2020.
- ↑ 刘灏 (21 January 2020). "广东市场监管部门:将坚决打击囤积居奇、哄抬价格等行为". 南方网. Archived from the original on 11 May 2020. Retrieved 21 January 2020.
- ↑ "市场价格行为提醒书". n.d. Archived from the original on 27 January 2020.
- ↑ 陈泽云 (22 January 2020). "口罩买不到怎么办?这些药店平台春节期间持续供应". 金羊网. Archived from the original on 22 January 2020. Retrieved 22 January 2020.
- ↑ 新京报 (22 January 2020). "京东:禁止第三方商家口罩涨价". 新京报网. Archived from the original on 27 January 2020. Retrieved 22 January 2020.
- ↑ 新京报 (22 January 2020). "苏宁易购:口罩等健康类商品禁涨价,并开展百亿补贴". 新京报网. Archived from the original on 22 January 2020. Retrieved 22 January 2020.
- ↑ 新京报 (22 January 2020). "拼多多:对口罩等产品进行监测,恶意涨价者将下架". 新京报网. Archived from the original on 22 January 2020. Retrieved 22 January 2020.
- ↑ 186.0 186.1 186.2 Olga Khazan, Why We're Running Out of Masks Archived 10 November 2021 at the Wayback Machine, The Atlantic (10 April 2020).
- ↑ Miroff N. "Protective gear in national stockpile is nearly depleted, DHS officials say". The Washington Post. Archived from the original on 1 April 2020. Retrieved 1 April 2020.
- ↑ Juliet Eilperin, Jeff Stein, Desmond Butler & Tom Hamburger, U.S. sent millions of face masks to China early this year, ignoring pandemic warning signs Archived 15 February 2021 at the Wayback Machine, The Washington Post (18 April 2020).
- ↑ 189.0 189.1 189.2 189.3 189.4 189.5 "Pénurie de masques : une responsabilité partagée par les gouvernements". Public Senat (in français). 23 March 2020. Archived from the original on 9 April 2020. Retrieved 6 April 2020.
- ↑ BFMTV. "Pénurie de masques: pourquoi la France avait décidé de ne pas renouveler ses stocks il y a neuf ans" (in français). BFMTV. Archived from the original on 6 April 2020. Retrieved 6 April 2020.
- ↑ Roy S, Barotte N (19 March 2020). "Quand l'État stratège a renoncé à renouveler ses stocks de masques". Le Figaro (in français). Archived from the original on 11 May 2020. Retrieved 6 April 2020.
- ↑ 192.0 192.1 "France to produce 40 million face masks by end of April for domestic battle against Covid-19". Radio France Internationale. 31 March 2020. Archived from the original on 6 April 2020. Retrieved 6 April 2020.
- ↑ "Covid-19: French lawmakers to investigate where one and a half billion masks sent". Radio France Internationale. 1 April 2020. Archived from the original on 6 April 2020. Retrieved 6 April 2020.
- ↑ "Pénurie de masques : les raisons d'un "scandale d'État"". Franceinter.fr. n.d. Archived from the original on 7 April 2020. Retrieved 6 April 2020.
- ↑ "National Case Study: France's Maker Response Against COVID-19". Open Source Medical Supplies. Archived from the original on 12 August 2021. Retrieved 18 March 2021.
- ↑ 196.0 196.1 "Countries reject Chinese-made equipment". BBC News. 30 March 2020. Archived from the original on 13 April 2020. Retrieved 23 April 2022.
- ↑ 197.0 197.1 197.2 Choi D (2 April 2020). "Chinese government rejects allegations that its face masks were defective, tells countries to 'double check' instructions". Business Insider France. Archived from the original on 10 May 2020. Retrieved 23 April 2022.
- ↑ "Trudeau says Canada will not pay full price for 8 million sub-standard masks". CTVNews. 9 May 2020. Archived from the original on 22 May 2021. Retrieved 23 April 2022.
- ↑ Bronskill J (8 May 2020). "Federal government rejects 8 million N95 masks from single distributor". Canadian Broadcasting Corporation. Archived from the original on 15 April 2021. Retrieved 23 April 2022.
- ↑ 200.0 200.1 Rohrlich J. "An Indiana hospital theft shows face masks and hand sanitizer are now as sought-after as drugs". Quartz. Archived from the original on 19 April 2021. Retrieved 23 April 2022.
- ↑ "Theft of masks, sanitizer at Naval Medical Center San Diego lead to bag checks for staff". San Diego Union-Tribune. 10 April 2020. Archived from the original on 12 August 2021. Retrieved 23 April 2022.
- ↑ "Thefts in hospitals lead to lockup of masks, protective gear amid COVID-19 supply shortage | CBC News". Archived from the original on 7 March 2021. Retrieved 23 April 2022.
- ↑ "Where is all the PPE?". AAMC. Archived from the original on 27 February 2021. Retrieved 23 April 2022.
- ↑ "2,000 surgical masks stolen from hospital in French city of Marseille". Al Arabiya English. 4 March 2020. Archived from the original on 27 October 2020. Retrieved 23 April 2022.
- ↑ "Upstate NY hospital worker arrested, accused of stealing face masks". syracuse. 30 March 2020. Archived from the original on 20 January 2021. Retrieved 23 April 2022.
- ↑ "West Java hospital employees arrested for allegedly stealing hundreds of boxes of masks". The Jakarta Post. Archived from the original on 28 October 2020. Retrieved 23 April 2022.
- ↑ Catoura C. "Ex-healthcare worker accused of stealing personal protective equipment arrested". CBS46 News Atlanta. Archived from the original on 3 November 2020. Retrieved 23 April 2022.
- ↑ "Charlie Norwood VA Medical Center employee arrested for stealing personal protective equipment". 10 April 2020. Archived from the original on 7 March 2021. Retrieved 23 April 2022.
- ↑ "Hospital employee steals personal protective equipment worth $1,700, police say". FOX 10 Phoenix. 4 April 2020. Archived from the original on 1 March 2021. Retrieved 23 April 2022.
- ↑ Phillips D. "Hospital worker stole personal protective equipment, cops say". sun-sentinel.com. Archived from the original on 28 June 2021. Retrieved 23 April 2022.
- ↑ "Ghana hospital workers cash in on PPE amid coronavirus". BBC News. 10 August 2020. Archived from the original on 8 November 2021. Retrieved 23 April 2022.
- ↑ Brown A. "2 SC men charged for allegedly stealing masks from federal law enforcement training center". Post and Courier. Archived from the original on 6 December 2020. Retrieved 23 April 2022.
- ↑ Cara A (8 January 2021). "UN fears 'massive' COVID transmission in Ethiopia's Tigray". Associated Press. Archived from the original on 18 April 2021. Retrieved 18 April 2021.
- ↑ Johnson M (26 March 2020). "Feds have 1.5 million expired N95 masks in storage despite CDC clearing them for use on COVID-19: report". The Hill. Archived from the original on 30 June 2020. Retrieved 12 April 2020.
- ↑ Evan M, Hufford A (7 March 2020). "Critical Component of Protective Masks in Short Supply – The epidemic has driven up demand for material in N95 filters; 'everyone thinks there is this magic factory somewhere'". The Wall Street Journal. Archived from the original on 1 April 2020. Retrieved 23 April 2022.
- ↑ 216.0 216.1 216.2 Fabian J, Clough R (2 April 2020). "Trump Attacks 3M Over Mask Production, Drawing Company Pushback". Bloomberg. Archived from the original on 22 June 2020. Retrieved 23 April 2022.
- ↑ Whalen J, Helderman RS, Hamburger T (3 April 2020). "Inside Americas Mask Crunch". The Washington Post. Archived from the original on 16 July 2020. Retrieved 23 April 2022.
- ↑ Halon Y (3 April 2020). "Florida emergency management official says 3M selling masks to foreign countries: 'We're chasing ghosts'". Fox News. Archived from the original on 17 May 2020. Retrieved 4 April 2020.
- ↑ "Interview With Jared Moskowitz, Director of Florida's Division of Emergency Management". WFOR-TV. 3 April 2020. Archived from the original on 10 May 2020. Retrieved 4 April 2020.
- ↑ Man A (5 April 2020). "Florida emergency management chief says state will have enough ICU beds and ventilators". Sun-Sentinel. Archived from the original on 4 May 2020. Retrieved 5 April 2020.
- ↑ DiSalvo D (30 March 2020). "I Spent A Day In The Coronavirus-Driven Feeding Frenzy Of N95 Mask Sellers And Buyers And This Is What I Learned". Forbes. Archived from the original on 18 May 2020. Retrieved 8 April 2020.
- ↑ Bertrand N, Orr G, Lippman D, Toosi N (31 March 2020). "Pence task force freezes coronavirus aid amid backlash". Politico. Archived from the original on 4 June 2020. Retrieved 8 April 2020.
- ↑ 223.0 223.1 223.2 "N95 masks save lives. So why are they still hard to get this far into a pandemic?". The Washington Post. Archived from the original on 8 September 2021. Retrieved 23 April 2022.
- ↑ Chase B (28 September 2020). "N95 mask shortage scares health care workers ahead of projected COVID-19 spike". Chicago Sun-Times. Archived from the original on 1 July 2021. Retrieved 23 April 2022.
- ↑ "Why the U.S. still has a shortage of N95 masks - The Washington Post". The Washington Post. Archived from the original on 12 February 2021. Retrieved 23 April 2022.
- ↑ "Everyone should be wearing N95 masks now". The Washington Post. Archived from the original on 16 July 2021. Retrieved 23 April 2022.
- ↑ Dhillon RS, Karan A, Beier D, Srikrishna D. "Perspective | The government can – and should – send high-quality masks to every American". The Washington Post. ISSN 0190-8286. Archived from the original on 21 February 2021. Retrieved 19 February 2021.
- ↑ Stolberg SG (19 January 2022). "Covid Live Updates: Biden Administration to Issue 400 Million Masks From National Stockpile - The nonsurgical N95 masks will be available free at community health centers and retail pharmacies across the United States". The New York Times. Archived from the original on 19 January 2022. Retrieved 19 January 2022.
- ↑ Betschka J, Fröhlich A (3 April 2020). "Berlins Innensenator spricht von 'moderner Piraterie'". Der Tagesspiegel (in Deutsch). Archived from the original on 23 July 2020. Retrieved 23 April 2022.
- ↑ "Schutzmasken konfisziert? Schwere Vorwürfe aus Berlin: Jetzt reagiert das Weiße Haus". t-online.de. 4 April 2020. Archived from the original on 4 April 2020. Retrieved 23 April 2022.
- ↑ Fröhlich A (4 April 2020). "200,000 respirators not confiscated: Delivery for Berlin police was bought in Thailand at a better price". Der Tagesspiegel. Archived from the original on 21 February 2021. Retrieved 23 April 2022.
- ↑ "Berlin lets mask slip on feelings for Trump's America". Politico Europe. 10 April 2020. Archived from the original on 1 May 2020. Retrieved 23 April 2022.
- ↑ Tisdall S (12 April 2020). "US's global reputation hits rock-bottom over Trump's coronavirus response". The Guardian. Archived from the original on 16 May 2020. Retrieved 23 April 2022.
- ↑ "National Case Study: Germany's Maker Response against COVID-19". Open Source Medical Supplies. Archived from the original on 13 August 2021. Retrieved 18 March 2021.
- ↑ "COVID-19: Coquitlam company retools, will be first in Canada to produce N95 respirators". 6 April 2020. Archived from the original on 6 July 2020. Retrieved 6 April 2020.
- ↑ "As imports hit roadblock, when can Canada make its own N95 masks?". Toronto Star. 23 May 2020. Archived from the original on 18 January 2021. Retrieved 23 April 2022.
- ↑ Bradsher K, Alderman L (2 April 2020). "The World Needs Masks. China Makes Them, but Has Been Hoarding Them". The New York Times. Archived from the original on 23 March 2020. Retrieved 7 May 2020.
China made half the world's masks before the coronavirus emerged there, and it has expanded production nearly 12-fold since then.
- ↑ For example:
"Face mask production shows no sign of stopping". PAhomepage. Nexstar Broadcasting, Inc. 22 April 2020. Archived from the original on 8 March 2021. Retrieved 7 May 2020.
[...] Martz Technologies in Berwick [in Pennsylvania] [...] turned their warehouse into a face mask factory.
- ↑ Enrich D, Abrams R, Kurutz S (25 March 2020). "A Sewing Army, Making Masks for America". The New York Times. Archived from the original on 28 November 2021. Retrieved 23 April 2022.
- ↑ Levy J (4 May 2020). "Need for masks spawns cottage industry". Republican-American. Waterbury CT: Republican American. Archived from the original on 2 November 2020. Retrieved 7 May 2020.
Production of face masks is becoming a cottage industry of sorts with some hybrid operations that both donate and sell the sought-after coverings.
- ↑ Bhanoo S. "Which DIY mask pattern should you use? Even experts can't pick one to recommend". The Washington Post. Archived from the original on 1 April 2020. Retrieved 23 April 2022.
- ↑ "Master Maskmaking Guide". Makemasks. Archived from the original on 14 August 2020. Retrieved 9 May 2020.
well-known patterns such as the Deaconess, A.B. mask (For a nurse, by a nurse), We Can Sew It, the Cynthia, and the Erin ... Full Pattern Library
- ↑ 243.0 243.1 Cissy Z (12 June 2020). "Coronavirus: wheels come off China's mask-making gravy train, as low-end manufacturers count their losses". South China Morning Post. Archived from the original on 27 November 2021. Retrieved 23 April 2022.
- ↑ "Makers Are 3D Printing Ventilator Gear and Sewing Masks to Fight the Coronavirus". Time. Archived from the original on 14 December 2021. Retrieved 29 December 2021.
- ↑
For example:
Blanchard B (1 April 2020). "Taiwan to spend $35 billion fighting virus, to donate 10 million masks". Reuters. Archived from the original on 3 April 2020. Retrieved 7 May 2020.
Taiwan [...] said it would donate ten million face masks to the most needy countries. [...] The Foreign Ministry said seven million masks would be sent to Europe, including Spain, Italy and Britain, while two million would go to the United States, and the rest to the small band of countries which maintain formal diplomatic ties with Taiwan [...].
- ↑ Kavilanz P (7 August 2020). "Etsy's on fire as reusable face mask sales surge". CNN. Archived from the original on 24 June 2021. Retrieved 25 August 2020.
- ↑ 247.0 247.1 247.2 247.3 Onishi N, Méheut C (9 April 2020). "Mask-Wearing Is a Very New Fashion in Paris (and a Lot of Other Places)". The New York Times. Archived from the original on 13 November 2021. Retrieved 23 April 2022.
- ↑ 248.0 248.1 Wong T (31 March 2020). "Why some countries wear face masks and others don't". BBC News. Archived from the original on 17 November 2021. Retrieved 23 April 2022.
- ↑ 249.0 249.1 249.2 249.3 Zheng S (14 March 2020). "Face mask culture during the coronavirus: East vs West". South China Morning Post. Archived from the original on 26 November 2021. Retrieved 23 April 2022.
- ↑ 250.0 250.1 Zhao X, Knobel P (June 2021). "Face mask wearing during the COVID-19 pandemic: comparing perceptions in China and three European countries". Translational Behavioral Medicine. 11 (6): 1199–1204. doi:10.1093/tbm/ibab043. PMC 8240840. PMID 33963866.
- ↑ Borunda A (27 April 2020). "America's face-mask culture is changing, and their meaning changes too". National Geographic. Archived from the original on 27 January 2021. Retrieved 23 April 2022.
- ↑ Gulland A (3 August 2020). "Wearing a face mask is an act of solidarity, WHO chief says". The Daily Telegraph. Archived from the original on 1 March 2021. Retrieved 23 April 2022.
- ↑ Kolstoe S (20 May 2020). "Coronavirus: wearing a cloth face mask is less about science and more about solidarity". The Conversation. Archived from the original on 30 October 2021. Retrieved 23 April 2022.
- ↑ Denworth L (14 May 2020). "Masks Reveal New Social Norms: What a Difference a Plague Makes". Scientific American. Archived from the original on 20 October 2021. Retrieved 23 April 2022.
- ↑ "Lessons From Slovakia – Where Leaders Wear Masks". The Atlantic. 13 May 2020. Archived from the original on 24 May 2020. Retrieved 23 April 2022.
- ↑ Leung H (12 March 2020). "Why Face Masks Are Encouraged in Asia, but Shunned in the U.S." Time. Archived from the original on 25 November 2021. Retrieved 23 April 2022.
- ↑ Barceló J, Sheen GC (6 May 2020). "Voluntary adoption of social welfare-enhancing behavior: Mask-wearing in Spain during the COVID-19 outbreak". PLOS ONE. 15 (12): e0242764. Bibcode:2020PLoSO..1542764B. doi:10.1371/journal.pone.0242764. PMC 7707551. PMID 33259531.
- ↑ 258.0 258.1 258.2 van der Westhuizen HM, Kotze K, Tonkin-Crine S, Gobat N, Greenhalgh T (August 2020). "Face coverings for covid-19: from medical intervention to social practice". BMJ. 370: m3021. doi:10.1136/bmj.m3021. PMID 32816815.
- ↑ 259.0 259.1 259.2 Eisenmann C, Meyer C (2020). "Wearing a Face Mask in Everyday Life – About Recalibrations in the Interactional Infrastructure of Global Cooperation". Global Cooperation Research - A Quarterly Magazine. 2 (2). ISSN 2629-3080. Archived from the original on 26 October 2020. Retrieved 23 April 2022.
- ↑ 260.0 260.1 Tett G (1 April 2020). "Why wearing masks may be the way forward". Financial Times. Archived from the original on 9 March 2021. Retrieved 23 April 2022.
- ↑ Friedman U (2 April 2020). "Face Masks Are In". The Atlantic. Archived from the original on 4 November 2021. Retrieved 23 April 2022.
- ↑ Howard J (28 March 2020). "Simple DIY masks could help flatten the curve. We should all wear them in public". The Washington Post. Archived from the original on 13 October 2021. Retrieved 23 April 2022.
- ↑ "New local website aims to promote mask wearing to help flatten the curve". News24. 7 April 2020. Archived from the original on 14 April 2020. Retrieved 23 April 2020.
- ↑ 264.0 264.1 264.2 264.3 264.4 Betsch C, Korn L, Sprengholz P, Felgendreff L, Eitze S, Schmid P, Böhm R (September 2020). "Social and behavioral consequences of mask policies during the COVID-19 pandemic". Proceedings of the National Academy of Sciences of the United States of America. 117 (36): 21851–21853. doi:10.1073/pnas.2011674117. PMC 7486713. PMID 32820078.
- ↑ "Coronavirus: To Mask Or Not To Mask? #Masks4All Seeks Everyone To Cover Their Mouths". CBS New York. 31 March 2020. Archived from the original on 24 February 2021. Retrieved 23 April 2022.
- ↑ Bhattarai A (8 July 2020). "Retail workers are being pulled into the latest culture war: Getting customers to wear masks". The Washington Post. Archived from the original on 13 February 2021. Retrieved 23 April 2022.
- ↑ Wolford B (30 June 2020). "Customers 'aggressive' over face mask policies force fed-up restaurants to close". Miami Herald. Archived from the original on 25 January 2021. Retrieved 23 April 2022.
- ↑ Norfleet N (1 July 2020). "As COVID-19 mask debate rages on, retailers reluctantly take brunt of enforcement". Star Tribune. Archived from the original on 27 June 2021. Retrieved 23 April 2022.
- ↑ Taylor K, Moné B (21 May 2020). "Workers at chains like Kroger, Costco, and Waffle House are on the front lines of an increasingly violent war between mask supporters and opponents". Business Insider. Archived from the original on 3 November 2021. Retrieved 23 April 2022.
- ↑ "Man dies after being shoved to the ground in New York mask altercation". The Guardian. 6 October 2020. Archived from the original on 11 May 2021. Retrieved 23 April 2022.
- ↑ Gibson K (23 July 2020). "U.S. retailers badly want shoppers to wear masks. Getting them to comply is another story". CBS News. Archived from the original on 14 August 2020. Retrieved 23 April 2022.
- ↑ 272.0 272.1 272.2 Zine J. "Unmasking the racial politics of the coronavirus pandemic". The Conversation. Archived from the original on 6 March 2021. Retrieved 23 April 2022.
- ↑ Burton N (6 March 2020). "Why Asians in masks should not be the "face" of the coronavirus". Vox. Archived from the original on 22 October 2021. Retrieved 23 April 2022.
- ↑ Nabong P (30 March 2020). "Wearing a mask while Asian". Chicago Reader. Archived from the original on 8 March 2021. Retrieved 23 April 2022.
- ↑ Young I (13 May 2020). "Coronavirus: Asian women in Canada are abused, punched and spat on. Is it racist maskaphobia?". South China Morning Post. Archived from the original on 15 May 2020. Retrieved 3 June 2020.
- ↑ Taylor DB (14 April 2020). "For Black Men, Fear That Masks Will Invite Racial Profiling". The New York Times. Archived from the original on 12 November 2021. Retrieved 23 April 2022.
- ↑ de la Garza A (16 April 2020). "For Black Men, Homemade Masks May Be a Risk All Their Own". Time. Archived from the original on 2 August 2021. Retrieved 23 April 2022.
- ↑ Alfonso III F (7 April 2020). "Why some people of color say they won't wear homemade masks". CNN. Archived from the original on 31 October 2021. Retrieved 23 April 2022.
- ↑ 279.0 279.1 Roffe E (15 July 2020). "Face masks: 'Impact on the deaf community will be vast'". Bedford Independent. Archived from the original on 15 September 2021. Retrieved 24 July 2020.
- ↑ 280.0 280.1 Taylor-Coleman J (26 May 2020). "Call for clear face masks to be 'the norm'". BBC News. Archived from the original on 18 April 2021. Retrieved 23 April 2022.
- ↑ Wright S (9 June 2020). "Five easy steps to get your dog used to face masks". Your Dog Magazine. Archived from the original on 31 October 2020. Retrieved 24 July 2020.
- ↑ 282.0 282.1 Courtney-Guy S (24 July 2020). "People with disabilities fear abuse for not wearing face masks in public". Metro. Archived from the original on 29 August 2020. Retrieved 24 July 2020.
- ↑ 283.0 283.1 Dwyer D (30 July 2020). "Few medical reasons for not wearing a face mask". ABC News. Archived from the original on 13 March 2021. Retrieved 23 April 2022.
- ↑ "American College of Chest Physicians, American Lung Association, American Thoracic Society and COPD Foundation Statement on Importance of Patients with Chronic Lung Disease Wearing Facial Coverings". American Lung Association. 16 July 2020. Archived from the original on 29 November 2021. Retrieved 23 April 2022.
- ↑ Brown M (16 July 2020). "Fact check: ADA does not provide blanket exemption from face mask requirements". USA Today. Archived from the original on 9 March 2021. Retrieved 23 April 2022.
- ↑ "Health Experts Stress Need To Fight 'Mask Exhaustion', Continue To Follow COVID Safety Guidelines". CBS New York. 12 November 2020. Archived from the original on 20 October 2021. Retrieved 23 April 2022.
- ↑ 287.0 287.1 287.2 Beswick E (14 July 2020). "Coronavirus: How the wearing of masks has exposed a divided Europe". euronews. Archived from the original on 11 October 2021. Retrieved 23 April 2022. See also Smith M (27 July 2020). "Face mask use surges after becoming compulsory in shops". YouGov. Archived from the original on 5 July 2021. Retrieved 23 April 2022.
- ↑ 288.0 288.1 Petersen MB, Lindholt MF, Jørgensen F. "Håndteringen af Coronaepidemien og Borgernes Adfærd, Tillid og Trivsel" (PDF). fm.dk (Danish Ministry of Finance). Institut for Statskundskab, Aarhus University. Archived (PDF) from the original on 16 September 2021. Retrieved 28 August 2021.
- ↑ Ibbetson C (31 July 2020). "Should supermarkets challenge those shopping without masks?". YouGov. Archived from the original on 17 May 2021. Retrieved 23 April 2022.
- ↑ 290.0 290.1 Hutchins HJ, Wolff B, Leeb R, Ko JY, Odom E, Willey J, et al. (October 2020). "COVID-19 Mitigation Behaviors by Age Group - United States, April-June 2020". MMWR. Morbidity and Mortality Weekly Report. 69 (43): 1584–1590. doi:10.15585/mmwr.mm6943e4. PMC 7641002. PMID 33119562.
- ↑ 291.0 291.1 Tschorn A (22 June 2020). "Mask shaming men won't work. Here's what will". Los Angeles Times. Archived from the original on 28 November 2021. Retrieved 23 April 2022.
- ↑ 292.0 292.1 Srikanth A (14 May 2020). "Men less likely to wear face masks because they're 'not cool' and 'a sign of weakness' says study". The Hill. Archived from the original on 13 September 2021. Retrieved 23 April 2022.
- ↑ Okten IO, Gollwitzer A, Oettingen G (2020). "Gender differences in preventing the spread of coronavirus". Behavioral Science & Policy. 6 (2): 109–122. doi:10.1353/bsp.2020.0022. S2CID 238608499. Archived from the original on 6 October 2021. Retrieved 23 April 2022.
- ↑ Willingham E (29 June 2020). "The Condoms of the Face: Why Some Men Refuse to Wear Masks". Scientific American. Archived from the original on 10 October 2021. Retrieved 23 April 2022.
- ↑ Wong B (23 July 2020). "The Psychology Behind Why Men Refuse To Wear Masks". HuffPost. Archived from the original on 30 October 2020. Retrieved 23 April 2022.
- ↑ Howard MC (February 2021). "Gender, face mask perceptions, and face mask wearing: Are men being dangerous during the COVID-19 pandemic?". Personality and Individual Differences. 170: 110417. doi:10.1016/j.paid.2020.110417. PMC 7543707. PMID 33052155.
- ↑ Pagliari C (17 June 2020). "What do world leaders really mean by refusing to wear face masks?". The University of Edinburgh. Archived from the original on 4 March 2021. Retrieved 23 April 2022.
- ↑ Le Roux M (8 May 2020). "To mask or not to mask? World leaders scrutinised over face coverings". Agence France-Presse. Archived from the original on 15 June 2020. Retrieved 23 April 2022 – via Yahoo! News.
- ↑ Serhan Y (13 May 2020). "Lessons From Slovakia – Where Leaders Wear Masks". The Atlantic. Archived from the original on 24 May 2020. Retrieved 23 April 2022.
- ↑ Smith S (10 August 2020). "Unmasked: How Trump's mixed messaging on face-coverings hurt U.S. coronavirus response". NBC News. Archived from the original on 22 October 2021. Retrieved 23 April 2022.
- ↑ Madhani A (27 June 2020). "What to wear: Feds' mixed messages on masks sow confusion". AP News. Archived from the original on 7 February 2021. Retrieved 23 April 2022.
- ↑ Blake A (27 October 2020). "GOP governors have overwhelmingly encouraged masks. Trump still resists them". The Washington Post. Archived from the original on 23 November 2020. Retrieved 23 April 2022.
- ↑ Mackey R (12 July 2020). "Trump Manages to Wear a Mask and Undercut Mask-Wearing at the Same Time". The Intercept. Archived from the original on 11 September 2021. Retrieved 14 November 2020.
- ↑ Quinn M (12 July 2020). "Surgeon general says administration "trying to correct" earlier guidance against wearing masks". CBS News. Archived from the original on 5 March 2021. Retrieved 23 April 2022.
- ↑ Griffiths J (2 April 2020). "Asia may have been right about coronavirus and face masks, and the rest of the world is coming around". CNN. Archived from the original on 2 April 2020. Retrieved 23 April 2022.
- ↑ Watterson A (17 April 2020). "Through all the misinformation, what is the truth of wearing face masks?". The National. Archived from the original on 8 March 2021. Retrieved 23 April 2022.
- ↑ Frank TA (8 April 2020). ""I Was Looking at Them in the Wrong Way": Mask Misinformation and the Failure of the Elites". Vanity Fair. Archived from the original on 19 January 2021. Retrieved 23 April 2022.
- ↑ 308.0 308.1 Huo J (10 April 2020). "Why There Are So Many Different Guidelines For Face Masks For The Public". NPR. Archived from the original on 12 March 2021. Retrieved 23 April 2022.
- ↑ "Coronavirus: Abrupt reversals on face mask policy raise new questions". France 24. 5 April 2020. Archived from the original on 12 March 2021. Retrieved 23 April 2022.
- ↑ Walther M (4 April 2020). "The noble lie about masks and coronavirus should never have been told". The Week. Archived from the original on 22 February 2021. Retrieved 23 April 2022.
- ↑ Tufekci Z (17 March 2020). "Why Telling People They Don't Need Masks Backfired". The New York Times. Archived from the original on 11 March 2021. Retrieved 23 April 2022.
- ↑ Jankowicz M (15 June 2020). "Fauci said US government held off promoting face masks because it knew shortages were so bad that even doctors couldn't get enough". Business Insider. Archived from the original on 16 September 2020. Retrieved 23 April 2022.
- ↑ Ross K (12 June 2020). "Dr. Fauci Explains Why Public Wasn't Told to Wear Masks When COVID-19 Pandemic Began". TheStreet. Archived from the original on 9 March 2021. Retrieved 23 April 2022.
- ↑ Kelley A (16 June 2020). "Fauci: why the public wasn't told to wear masks when the coronavirus pandemic began". The Hill. Archived from the original on 11 March 2021. Retrieved 23 April 2022.
- ↑ McArdle M (16 June 2020). "Fauci Confirms Public-Health Experts Downplayed Efficacy of Masks to Ensure They Would Be Available to Health-care Workers". National Review. Archived from the original on 22 February 2021. Retrieved 23 April 2022.
- ↑ Novak M (17 June 2020). "Dr. Fauci Made the Coronavirus Pandemic Worse by Lying About Masks". Gizmodo. Archived from the original on 31 August 2021. Retrieved 23 April 2022.
- ↑ 317.0 317.1 317.2 Aratani L (29 June 2020). "How did face masks become a political issue in America?". The Guardian. Archived from the original on 28 November 2021. Retrieved 23 April 2022.
- ↑ 318.0 318.1 318.2 318.3 Weissert W, Lemire J (7 May 2020). "Face masks make a political statement in era of coronavirus". AP News. Archived from the original on 28 November 2021. Retrieved 23 April 2022.
- ↑ 319.0 319.1 319.2 Brewster J. "New Coronavirus Culture War: Some Republicans (Like Trump) Ditch Masks". Forbes. Archived from the original on 9 March 2021. Retrieved 3 June 2020.
- ↑ Walsh B. "Polls show politics, not public health, drive Americans' attitudes toward coronavirus masks". Axios. Archived from the original on 9 September 2021. Retrieved 23 April 2022.
- ↑ Pancevski B, Douglas J (29 June 2020). "Masks Could Help Stop Coronavirus. So Why Are They Still Controversial?". The Wall Street Journal. Archived from the original on 21 October 2021. Retrieved 23 April 2022.
- ↑ 322.0 322.1 Facciani M (9 September 2020). "Video: How did mask wearing become so politicized?". The Conversation. Archived from the original on 22 August 2021. Retrieved 23 April 2022.
- ↑ 323.0 323.1 323.2 323.3 Tu J (1 April 2020). "Taiwan challenges gender stereotypes with pink mask campaign". Women's Agenda. Archived from the original on 12 July 2021. Retrieved 3 June 2020.
- ↑ 324.0 324.1 Picheta R (20 July 2020). "Hundreds of demonstrators, some wearing masks, protest against mask-wearing in London". CNN. Archived from the original on 24 May 2021. Retrieved 23 April 2022.
- ↑ Beer T (16 July 2020). "Anti-Mask Rallies Continue In U.S. Amid Rising Coronavirus Cases And Deaths". Forbes. Archived from the original on 19 November 2021. Retrieved 23 April 2022.
- ↑ 326.0 326.1 Bogart N (20 July 2020). "Anti-mask rallies held across Canada despite increased support for mandatory masks". CTV News. Archived from the original on 27 November 2021. Retrieved 23 April 2022.
- ↑ Smyth M (21 July 2020). "Don't get smug about the U.S. – coronavirus could come back to bite Canada, too". Global News. Archived from the original on 27 February 2021. Retrieved 23 April 2022.
- ↑ Kaufman S (19 October 2020). "Violent Anti-Mask Protests Break Out In Czech Republic". Newsy. Archived from the original on 26 February 2021. Retrieved 23 April 2022.
- ↑ Jap K (18 October 2020). "After the demonstration, the Old Town Square turned into a battlefield". Novinky. Archived from the original on 10 April 2022. Retrieved 23 April 2022.
- ↑ Molteni M, Rogers A (2 July 2020). "How Masks Went From Don't-Wear to Must-Have During the Coronavirus Pandemic". Wired. Archived from the original on 26 November 2021. Retrieved 23 April 2022.
- ↑ Rinkunas S (20 April 2020). ""My Body, My Choice" Doesn't Apply to Coronavirus". Vice. Archived from the original on 23 July 2021. Retrieved 23 April 2022.
- ↑ "'My body, my choice': Sen. Chase defends maskless indoor campaign event". WTVR. 9 October 2020. Archived from the original on 6 February 2021. Retrieved 23 April 2022.
- ↑ Beer T (24 June 2020). "'I Can't Breathe' Shouts Arizona Councilman Before Removing Mask At 'Anti-Mask' Rally". Forbes. Archived from the original on 13 September 2021. Retrieved 23 April 2022.
- ↑ Parrish J (30 November 2020). "Downtown Boise businesses targeted by anti-mask protesters: A group of anti-mask protesters went into Boise businesses on Saturday to 'serve' them papers saying their mask policies were illegal". KTVB. Archived from the original on 30 January 2021. Retrieved 5 December 2020.
- ↑ Aratani L (29 June 2020). "How did face masks become a political issue in America?". The Guardian. Archived from the original on 28 November 2021. Retrieved 16 January 2021.
- ↑ Kane PL (29 April 2020). "The Anti-Mask League: lockdown protests draw parallels to 1918 pandemic". The Guardian. Archived from the original on 30 April 2020. Retrieved 8 December 2020.
- ↑ "Anti-Maskers Ready to Start Masking—to Protect Themselves From the Vaccinated". Vice. Archived from the original on 14 May 2021. Retrieved 12 May 2021.
- ↑ Steinbrecher L (25 June 2020). "Utah's faith leaders urge followers to wear masks in public". Fox News. Archived from the original on 20 April 2021. Retrieved 6 August 2020.
- ↑ Lennihan M (7 October 2020). "Faces meet fashion in New Yorkers' mask choices". AP News. Archived from the original on 21 October 2020. Retrieved 23 April 2022.
- ↑ 340.0 340.1 Sanoff R (7 April 2020). "Coronavirus couture: the rise of the $60 designer face mask". The Guardian. Archived from the original on 8 March 2021. Retrieved 23 April 2022.
- ↑ Elan P (10 September 2020). "Face masks pick perilous path from health protector to fashion accessory". The Guardian. Archived from the original on 28 July 2021. Retrieved 23 April 2022.
- ↑ Rabimov S (27 April 2020). "20 Fashion Brands Getting Most Creative With Coronavirus Face Masks". Forbes. Archived from the original on 19 October 2021. Retrieved 23 April 2022.
- ↑ Sutton S (12 October 2020). "2020's Highly-Debated Outfit Trick Is Actually Extremely Popular". InStyle. Archived from the original on 13 February 2021. Retrieved 23 April 2022.
- ↑ Williams S (16 May 2020). "Coronavirus: How face masks are becoming fashionable". BBC News. Archived from the original on 22 May 2021. Retrieved 23 April 2022.
- ↑ Holland O, Ananda P (24 March 2020). "Fashion industry answers the call for masks and personal protective equipment to fight Covid-19". CNN. Archived from the original on 13 October 2021. Retrieved 23 April 2022.
- ↑ Givhan R (5 May 2020). "Masks are here to stay. And they're quickly becoming a way to express ourselves". The Washington Post. Archived from the original on 18 September 2021. Retrieved 23 April 2022.
- ↑ Parisi D (27 July 2020). "Fashion warms up to face masks as a new product category". Glossy. Archived from the original on 15 November 2020. Retrieved 23 April 2022.
- ↑ 348.0 348.1 Jana R (20 August 2020). "Are masks helping or hindering the fashion industry?". The Daily Telegraph. Archived from the original on 2 November 2021. Retrieved 23 April 2022.
- ↑ Carreon J (10 August 2020). "Match Your Full Look to Your Face Mask, Because This Is How We Dress Now". Elle. Archived from the original on 24 February 2021. Retrieved 23 April 2022.
- ↑ 350.0 350.1 Besser R (22 May 2020). "Believe It or Not, There Is an Overarching Face Mask Trend". Vogue. Archived from the original on 25 February 2021. Retrieved 23 April 2022.
- ↑ Sytas A (6 May 2020). "Lithuanian capital holds 'Mask Fashion Week' amid coronavirus pandemic". Reuters. Archived from the original on 10 October 2020. Retrieved 23 April 2022.
- ↑ Puhak J (14 August 2020). "Disney releases uniform coronavirus face masks for theme park employees". Fox News. Archived from the original on 18 March 2021. Retrieved 23 April 2022.
- ↑ Henderson C. "Disney debuts matching pixie dust masks for theme park employees". USA Today. Archived from the original on 11 January 2021. Retrieved 23 April 2022.
- ↑ Laville S (18 November 2020). "53m discarded Covid face masks in UK 'could be polluting the sea'". The Guardian. Archived from the original on 29 August 2021. Retrieved 23 April 2022.
- ↑ Bowyer C, Roberts KP, Kolstoe S, Fletcher S (14 August 2020). "Coronavirus face masks: an environmental disaster that might last generations". The Conversation. Archived from the original on 27 November 2021. Retrieved 23 April 2022.
- ↑ Coronado L (24 October 2020). "Environmentalists Track Increase in Face Masks and Trash Since Pandemic". NBC 7 San Diego. Archived from the original on 14 October 2021. Retrieved 20 November 2020.
- ↑ Parashar N, Hait S (March 2021). "Plastics in the time of COVID-19 pandemic: Protector or polluter?". The Science of the Total Environment. 759: 144274. doi:10.1016/j.envc.2021.100039. PMC 7873601. PMID 33333331.
- ↑ Khan J, Momin SA, Mariatti M, Vilay V, Todo M (November 2021). "Recent advancements in nonwoven bio-degradable facemasks to ameliorate the post-pandemic environmental impact". Materials Research Express. 8 (11): 112001. Bibcode:2021MRE.....8k2001K. doi:10.1088/2053-1591/ac35d0.
- ↑ "BfArM - Empfehlungen des BfArM - Hinweise des BfArM zur Verwendung von Mund-Nasen-Bedeckungen, medizinischen Gesichtsmasken sowie partikelfiltrierenden Halbmasken (FFP-Masken)". Archived from the original on 16 April 2020. Retrieved 1 October 2021.
- ↑ "Wort für Mund-Nasen-Schutz auf Saterfriesisch gesucht". Archived from the original on 1 October 2021. Retrieved 23 April 2022.
- ↑ "Was heißt "Mund-Nasen-Schutz" auf Saterfriesisch?". Archived from the original on 29 October 2021. Retrieved 23 April 2022.
- ↑ "Mund-Nasen-Schutz auf saterfriesisch: "Sküüldouk"". Archived from the original on 1 October 2021. Retrieved 23 April 2022.
- ↑ "Wie heißt "Mund-Nasen-Schutz" auf Friesisch?". 14 May 2020. Archived from the original on 1 October 2021. Retrieved 23 April 2022.
- ↑ "Wie heißt "Mund-Nasen-Schutz" auf Friesisch?". Archived from the original on 1 October 2021. Retrieved 23 April 2022.
- ↑ "Personal measures taken to avoid COVID-19 | YouGov". today.yougov.com. Archived from the original on 2 December 2021. Retrieved 9 August 2020.
- ↑ "COVID-19: Face masks mandatory in Buenos Aires as of next Wednesday". The Santiago Times. 14 April 2020. Archived from the original on 2 November 2021. Retrieved 23 April 2022.
- ↑ "Face mask rules". 15 December 2021. Archived from the original on 10 October 2021. Retrieved 23 April 2022.
- ↑ "When should masks be worn in the community, in Australia?" (PDF). Department of Health. 9 June 2020. Archived (PDF) from the original on 30 March 2021. Retrieved 16 July 2020.
- ↑ "Department of Health and Human Services Victoria | Face coverings – Metropolitan Melbourne and Mitchell Shire". www.dhhs.vic.gov.au. Archived from the original on 25 July 2020. Retrieved 25 July 2020.
- ↑ "Advice on managing the health risks from COVID-19 on international flights" (PDF). Australian Department of Health. Archived (PDF) from the original on 30 November 2021. Retrieved 23 September 2021.
- ↑ Coronavirus: Expert panel to assess face mask use by public Archived 2 November 2021 at the Wayback Machine, BBC News, David Shukman, 1 April 2020.
- ↑ Bell B (6 April 2020). "Coronavirus: Why you now have to wear a mask in Austrian shops". BBC News. Archived from the original on 15 November 2021. Retrieved 11 April 2020.
- ↑ mask duty – the most important questions and answers (german), news@ORF.at, 31 March 2020 and actualized later.
- ↑ "Bahamas PM's National Press Conference: Update on COVID-19 Response". Eleutheran Newspaper. 19 April 2020. Archived from the original on 17 July 2021. Retrieved 23 April 2022.
- ↑ "Bahrain makes face masks compulsory in public, allows shops to re-open". Arab News. 9 April 2020. Archived from the original on 12 July 2021. Retrieved 22 April 2020.
- ↑ Benin Police Enforce Mask Wearing In Bid To Stop Virus Archived 8 March 2021 at the Wayback Machine, Barron's, 8 April 2020.
- ↑ Andelane L (7 April 2020). "Coronavirus: Countries where face masks are mandatory in COVID-19 fight". Newshub. Archived from the original on 24 April 2020. Retrieved 11 April 2020.
- ↑ Hinshaw DL (31 March 2020). "U.S. Reviews Guidance on Masks to Fight Coronavirus as Europe Embraces Their Use". Archived from the original on 9 March 2021. Retrieved 23 April 2022.
- ↑ Paun C, Furlong A, Mischke J (4 April 2020). "European authorities' shifting advice on face masks adds to confusion in coronavirus crisis". Archived from the original on 6 August 2021. Retrieved 23 April 2022.
- ↑ Bopha P, Khan S. "Cambodian Businesses Embrace Protective Measures Against Coronavirus". VOA Khmer. Archived from the original on 20 April 2021. Retrieved 23 April 2022.
- ↑ Cameroon City Makes Wearing Mask Mandatory in Fight Against Coronavirus Archived 17 April 2021 at the Wayback Machine, VOA News, 7 April 2020.
- ↑ Theresa Tam offers new advice: Wear a non-medical face mask when shopping or using public transit Archived 18 August 2020 at the Wayback Machine, The Globe and Mail, 6 April 2020.
- ↑ https://regina.ctvnews.ca/here-s-what-the-expiry-of-saskatchewan-s-public-health-order-means-for-you-1.5798918 Archived 1 March 2022 at the Wayback Machine[bare URL]
- ↑ https://calgary.ctvnews.ca/alberta-mask-mandates-end-at-midnight-monday-1.5800101 Archived 1 March 2022 at the Wayback Machine[bare URL]
- ↑ Chile afirma estar en una 'guerra' por los recursos contra el COVID-19 Archived 9 May 2021 at the Wayback Machine, Diario Libre, 6 April 2020.
- ↑ "For different groups of people: how to choose masks". NHC.gov.cn. National Health Commission of the People's Republic of China. 7 February 2020. Archived from the original on 5 April 2020. Retrieved 22 March 2020.
Disposable medical masks: Recommended for: · People in crowded places · Indoor working environment with a relatively dense population · People going to medical institutions · Children in kindergarten and students at school gathering to study and do other activities
- ↑ "关于印发公众科学戴口罩指引的通知引". NHC.gov.cn (in 中文). Chinese Center for Disease Control and Prevention. 18 March 2020. Archived from the original on 20 March 2020.
- ↑ Shanghai makes wearing masks mandatory in public places Archived 7 March 2021 at the Wayback Machine, Xinhuanet, 8 February 2020.
- ↑ "Prevention of Coronavirus Disease 2019 (COVID-19)" (PDF). Centre for Health Protection. Archived (PDF) from the original on 21 March 2020. Retrieved 22 March 2020.
- ↑ "Hong Kong protesters defy face mask ban — with humor". Deutsche Welle. Archived from the original on 27 October 2019. Retrieved 23 April 2022.
- ↑ "El uso de mascarillas se vuelve obligatorio en todo Colombia". Infobae (in español). Archived from the original on 8 May 2021. Retrieved 23 April 2020.
- ↑ "Slobodna Dalmacija – Danas se u Hrvatskoj uvode nove mjere? Stožeru problematična okupljanja, čak i na otvorenom, maske ćemo morati nositi u svim zatvorenim prostorima". slobodnadalmacija.hr (in hrvatski). 8 July 2020. Archived from the original on 8 March 2021. Retrieved 8 July 2020.
- ↑ "Cuba confirms 1st coronavirus cases, urges citizens to make own masks". Reuters. 11 March 2020. Archived from the original on 28 July 2020. Retrieved 11 March 2020.
- ↑ 'Pregnant' phase for Jamaica Archived 8 May 2021 at the Wayback Machine, Jamaica Observer, 6 April 2020.
- ↑ "Czechs get to work making masks after government decree". The Guardian. 30 March 2020. Archived from the original on 30 March 2020. Retrieved 23 April 2022.
- ↑ "Masks will be mandatory in all indoor premises of buildings in CZ from Thursday". Ministry of Health of the Czech Republic. 11 September 2020. Archived from the original on 28 November 2021. Retrieved 6 November 2020.
- ↑ "Face masks will be required outside and in cars in the Czech Republic from Wednesday". Expats.cz. 19 October 2020. Archived from the original on 12 July 2021. Retrieved 6 November 2020.
- ↑ Diario L (16 April 2020). "El uso de mascarillas en el país será obligatorio en espacios públicos y lugares de trabajo". listindiario.com (in español). Archived from the original on 27 February 2021. Retrieved 26 April 2020.
- ↑ 399.0 399.1 Tasamba J (19 April 2020). "Rwanda, DR Congo make mask wearing mandatory". Archived from the original on 18 April 2021. Retrieved 23 April 2022.
- ↑ "Bekendtgørelse om mundbindskrav klar". Bekendtgørelse om mundbindskrav klar (in dansk). Archived from the original on 20 January 2021. Retrieved 9 November 2020.
- ↑ "Farvel til mundbindet (næsten) alle steder: Få overblikket over ny genåbningsaftale". DR. 10 June 2021. Archived from the original on 22 December 2021. Retrieved 22 December 2021.
- ↑ "Mundbind og coronapas genindføres i dele af erhvervslivet" (in dansk). Erhvervsministeriet (Ministry of Trade and Industry). 27 November 2021. Archived from the original on 22 December 2021. Retrieved 22 December 2021.
- ↑ "Krav om mundbind i kollektiv transport og indenrigsfly" (in dansk). Transportministeriet (Ministry of Transport). 27 November 2021. Archived from the original on 22 December 2021. Retrieved 22 December 2021.
- ↑ "Mere end 99 procent af passagererne benytter mundbind eller visir". DR. 28 August 2021. Archived from the original on 22 December 2021. Retrieved 22 December 2021.
- ↑ LatAm countries turn to face masks to contain pandemic Archived 8 March 2021 at the Wayback Machine, Xinhuanet, 8 April 2020.
- ↑ Morsy A (2 June 2020). "Masks in public places: 'Even a piece of cloth will do'". Ahram Online. Archived from the original on 24 February 2021. Retrieved 10 June 2020.
- ↑ Samuel G (12 April 2020). "Ethiopia Outlaws Handshakes, Obliges Masks in Public Places". Archived from the original on 7 May 2021. Retrieved 23 April 2022.
- ↑ "Recommendation on the use of face masks for citizens". Finnish Institute for Health and Welfare. Archived from the original on 27 November 2021. Retrieved 17 August 2020.
- ↑ "Décret n° 2020-190 du 3 mars 2020 relatif aux réquisitions nécessaires dans le cadre de la lutte contre le virus covid-19". Legifrance (in français). 3 March 2020. Archived from the original on 31 July 2020. Retrieved 23 April 2022.
- ↑ "Coronavirus : le gouvernement promet 200 millions de masques par semaine dès lundi". DNA.fr (in français). 8 May 2020. Archived from the original on 8 March 2021. Retrieved 23 April 2022.
- ↑ "Macron: Wearing masks 'in enclosed public spaces' to become mandatory in France". France 24. 14 July 2020. Archived from the original on 27 October 2021. Retrieved 23 April 2022.
- ↑ "COVID-19 Information". U.S. Embassy in Gabon. Archived from the original on 25 November 2021. Retrieved 22 April 2020.
- ↑ "Plötzlich ändert das Robert-Koch-Institut seine Einschätzung zum Mundschutz". Die Welt (in Deutsch). dpa/AP. 2 April 2020. Archived from the original on 30 October 2021. Retrieved 2 April 2020.
- ↑ Rottmann K (28 April 2020). "Berlin und Mecklenburg-Vorpommern weiten Maskenpflicht aus – das gilt in Ihrem Bundesland". Die Welt (in Deutsch). Archived from the original on 19 November 2021. Retrieved 20 May 2020.
- ↑ "Coronavirus: Germans don compulsory masks as lockdown eases". BBC News. 27 April 2020. Archived from the original on 10 May 2020. Retrieved 29 April 2020.
- ↑ "Coronavirus: Germany's new face mask regulations explained". DW. 27 April 2020. Archived from the original on 28 May 2020. Retrieved 29 July 2020.
- ↑ Dzisi EK, Dei OA (September 2020). "Adherence to social distancing and wearing of masks within public transportation during the COVID 19 pandemic". Transportation Research Interdisciplinary Perspectives. 7: 100191. doi:10.1016/j.trip.2020.100191. PMC 7396893. PMID 34173465.
- ↑ "Guatemala makes it mandatory to wear face masks in public spaces (in Spanish)". 8 April 2020. Archived from the original on 21 February 2021. Retrieved 23 April 2022.
- ↑ Masilela B (14 April 2020). "Guinean president makes masks compulsory in bid to curb the spread of coronavirus". Archived from the original on 8 March 2021. Retrieved 23 April 2022., IOL
- ↑ Archeta K (7 April 2020). "Honduras makes it mandatory to wear face masks in public". Archived from the original on 21 April 2020. Retrieved 21 April 2020., COVID-19 World News
- ↑ "Archive copy". Archived from the original on 24 February 2022. Retrieved 23 April 2022.
{{cite web}}: CS1 maint: archived copy as title (link) - ↑ "How Iceland Beat the Coronavirus". The New Yorker. 1 June 2020. Archived from the original on 21 September 2021. Retrieved 16 July 2020.
- ↑ "Advisory on use of Homemade Protective Cover for Face and Mouth" (PDF). Office of the Principal Scientific Adviser to the Government of India. 3 April 2020. Archived from the original (PDF) on 16 June 2020. Retrieved 16 June 2020.
- ↑ Mohan V (1 April 2020). "Govt's scientific adviser 'differs' with ministry, pitches for home-made masks". The Times of India. Archived from the original on 8 March 2021. Retrieved 16 June 2020.
- ↑ COVID-19 In Odisha: State Govt Mandates Wearing Face Masks Archived 20 April 2021 at the Wayback Machine, Ommcom News, 6 April 2020.
- ↑ Bhandari A (12 April 2020). "West Bengal makes wearing mask mandatory in public places". Zee News. Archived from the original on 8 March 2021. Retrieved 16 June 2020.
- ↑ India TV News Desk (12 April 2020). "West Bengal joins other states in making face mask mandatory in public spaces". IndiaTV. Archived from the original on 10 March 2021. Retrieved 16 June 2020.
- ↑ Ngui Y (8 April 2020). "Malaysia to Give Out Masks to Households as Guidance Shifts". Bloomberg. Archived from the original on 3 May 2021. Retrieved 12 April 2020.
- ↑ "Face coverings during COVID-19". CSO.ie. Archived from the original on 25 November 2021. Retrieved 2 December 2020.
- ↑ "Guidance on safe use of face coverings". gov.ie. Archived from the original on 3 October 2020. Retrieved 15 May 2020.
- ↑ "Netanyahu tells Israelis to wear masks outside; gives stipends for kids, elderly". The Times of Israel. Archived from the original on 4 May 2021. Retrieved 23 April 2022.
- ↑ "Coronavirus: Lombardy, Tuscany make face masks compulsory". ANSA. 6 April 2020. Archived from the original on 11 July 2021. Retrieved 23 April 2022.
- ↑ e Fiorenza Sarzanini MG (10 July 2020). "Da oggi mascherine obbligatorie (anche in ufficio): tutte le regole per evitare la multa fino a mille euro". Corriere della Sera (in italiano). Archived from the original on 14 May 2021. Retrieved 13 November 2020.
- ↑ ""Très touchée" par le covid-19, Marcory rend le port de masques obligatoire dans les grandes surfaces". Agence Ivoirienne de Presse. 16 April 2020. Archived from the original on 20 April 2021. Retrieved 23 April 2022.
- ↑ Takahashi R. "Amid virus outbreak, Japan stores scramble to meet demand for face masks". Japan Times. Archived from the original on 1 February 2020. Retrieved 1 February 2020.
- ↑ "16th Meeting of the Novel Coronavirus Response Headquarters" Archived 31 October 2020 at the Wayback Machine. Prime Minister of Japan and His Cabinet, 1 March 2020.
- ↑ Muraya J (5 April 2020). "Kenya: Masks Now Mandatory in Public Places, Kenya Declares". All Africa. Archived from the original on 6 May 2021. Retrieved 23 April 2022.
- ↑ Senkpeni AD (21 April 2020). "Will You Wear Mask? Liberia's Lawmakers Want Compulsory Wearing of 'Protective Device' In Public". Archived from the original on 6 May 2021. Retrieved 23 April 2022., Front Page Africa
- ↑ Five stories you may have missed Archived 30 November 2020 at the Wayback Machine, Luxembourg Times, 18 April 2020.
- ↑ Lim I (17 March 2020). "Minister bans Malaysia from exporting face masks". The Malay Mail. Archived from the original on 19 March 2020. Retrieved 12 April 2020.
- ↑ "Face masks in public compulsory from Aug 1". FMT. 23 July 2020. Archived from the original on 5 October 2020. Retrieved 23 July 2020.
- ↑ "Face mask mandatory for crowded spaces, public transport from Aug 1". Malaysiakini. 23 July 2020. Archived from the original on 29 December 2020. Retrieved 23 July 2020.
- ↑ "Use of face masks compulsory in crowded public spaces from Aug 1". TheEdge. 23 July 2020. Archived from the original on 23 July 2020. Retrieved 23 July 2020.
- ↑ Pemakaian Pelitup Muka Adalah Wajib Archived 31 October 2020 at the Wayback Machine, Selangor Task Force COVID-19, 24 July 2020.
- ↑ Use of face masks declared mandatory in at least 11 states, Mexico City Archived 14 April 2021 at the Wayback Machine, Mexico News Daily, 17 April 2020.
- ↑ Wilson B (16 March 2020). "Mongolia Announces 3 New COVID-19 Cases, Totaling 4: How They Got Coronavirus Precautions Right". Archived from the original on 4 June 2020. Retrieved 23 April 2022., Forbes
- ↑ Eljechtimi A (6 April 2020). "Morocco makes face masks compulsory due to coronavirus". Reuters. Archived from the original on 8 June 2021. Retrieved 11 April 2020.
- ↑ "Mozambique: Government Orders Wearing of Masks". allAfrica.com. 9 April 2020. Archived from the original on 8 March 2021. Retrieved 22 April 2020.
- ↑ "Van Dissel heeft begrip voor mondkapjesplicht, maar blijft kritisch". nos.nl (in Nederlands). Archived from the original on 13 October 2020. Retrieved 7 May 2020.
- ↑ "Op deze plekken in Amsterdam en Rotterdam moet je nu een mondkapje op". NU.nl (in Nederlands). 5 August 2020. Archived from the original on 4 October 2020. Retrieved 8 August 2020.
- ↑ "Amsterdam and Rotterdam stop requiring face masks in busy places". DutchNews.nl. 28 August 2020. Archived from the original on 23 January 2021. Retrieved 1 September 2020.
- ↑ "Dit zijn vanaf vanavond de nieuwe coronamaatregelen". nos.nl (in Nederlands). Archived from the original on 12 July 2021. Retrieved 29 September 2020.
- ↑ du Pré R (30 September 2020). "Per direct geldt voor heel Nederland dringend advies om een mondkapje te dragen in 'publieke binnenruimte'". de Volkskrant (in Nederlands). Archived from the original on 12 July 2021. Retrieved 30 September 2020.
- ↑ "Boete van 95 euro als je geen mondkapje draagt, geen strafblad". NOS (in Nederlands). 11 November 2020. Archived from the original on 17 April 2021. Retrieved 23 April 2022.
- ↑ "Mondkapje verplicht vanaf 1 december - Nieuwsbericht - Rijksoverheid.nl". Rijksoverheid (in Nederlands). 19 November 2020. Archived from the original on 30 August 2021. Retrieved 23 April 2022.
- ↑ "COVID-19: Use of masks and face coverings in the community". Ministry of Health. 7 October 2020. Archived from the original on 4 August 2020. Retrieved 27 October 2020.
- ↑ Kolekjevski I (19 April 2020). "Citizens of Kumanovo, Tetovo and Prilep must wear protective masks and gloves as of wednesday: gov't". Archived from the original on 1 March 2021. Retrieved 22 April 2020., MIA
- ↑ "Questions and answers on novel coronavirus". Use of face masks: Norwegian Institute of Public Health. 11 June 2020. Archived from the original on 26 November 2021. Retrieved 16 July 2020.
- ↑ Balochistan govt makes face masks mandatory Archived 29 November 2020 at the Wayback Machine, Pakistan Today, 18 April 2020.
- ↑ "Es 'obligatorio' usar mascarilla si va a salir de casa, según ministra consejera de Salud". TVN. 7 April 2020. Archived from the original on 8 March 2021. Retrieved 23 April 2022.
- ↑ Mercado D. "Mascarillas gratis: Perú decreta su uso obligatorio para enfrentar el coronavirus". Infobae (in español). Archived from the original on 11 September 2021. Retrieved 22 April 2020.
- ↑ "Philippines requires people to wear masks in public". 2 April 2020. Archived from the original on 8 March 2021. Retrieved 23 April 2022.
- ↑ Ranada P (15 December 2020). "Filipinos now required to wear 'full' face shields, masks outside homes". Rappler. Archived from the original on 25 June 2021. Retrieved 23 April 2022.
- ↑ Gita-Carlos RA (21 August 2020). "Use of face shields now mandatory in commercial establishments". Philippine News Agency. Archived from the original on 12 July 2021. Retrieved 23 April 2022.
- ↑ "Wychodzisz z domu? Zasłoń usta i nos!". Gov.pl. 16 April 2020. Archived from the original on 23 November 2021. Retrieved 23 April 2022.
- ↑ "Masks made compulsory outside in Poland as coronavirus cases surge". Reuters. 8 October 2020. Archived from the original on 28 June 2021. Retrieved 27 May 2021.
- ↑ "ROZPORZĄDZENIE RADY MINISTRÓW z dnia 6 maja 2021 r. w sprawie ustanowienia określonych ograniczeń, nakazów i zakazów w związku z wystąpieniem stanu epidemii". sip.lex.pl (in Polish). 6 May 2021. Archived from the original on 12 July 2021. Retrieved 27 May 2020.
{{cite web}}: CS1 maint: unrecognized language (link) - ↑ Face masks made mandatory in Russia's Khabarovsk to prevent coronavirus spread Archived 28 February 2021 at the Wayback Machine, Tass, 7 April 2020.
- ↑ "Krizni štab: Maske obavezne, mere postepene". Nova.rs (in српски / srpski). 29 June 2020. Archived from the original on 31 July 2020. Retrieved 29 June 2020.
- ↑ "Slovensko pritvrdilo v boji s vírusom. Nosenie rúšok je povinné". spravy.pravda.sk (in slovenčina). 15 March 2020. Archived from the original on 17 March 2020. Retrieved 15 March 2020.
- ↑ "Opatrenie Úradu verejného zdravotníctva Slovenskej republiky pri ohrození verejného zdravia" [Measures taken by the Public Health Office of the Slovak Republic in case of public health threat] (PDF). uvzsr.sk (in slovenčina). Archived (PDF) from the original on 1 April 2020. Retrieved 24 March 2020.
- ↑ "Rúška už nebudú povinné všade, povolia cesty do zahraničia na krátky čas". Petit Press (in slovenčina). Archived from the original on 20 March 2021. Retrieved 20 May 2020.
- ↑ COVID-19 & Slovenia, Night 29 March: Movement Restrictions, Mandatory Masks, More Aid for Individuals Archived 21 April 2021 at the Wayback Machine, Total Slovenia News, 29 March 2020.
- ↑ Prime Minister Janez Janša has presented the latest measures to contain the spread of coronavirus infection Archived 9 May 2021 at the Wayback Machine, GOV.SI Portal, 14 October 2020.
- ↑ "Everyone should wear a face mask". COVID-19 South African online portal. 10 April 2020. Archived from the original on 11 April 2020. Retrieved 11 April 2020.
- ↑ "South Africans must wear masks after COVID-19 lockdown eases: Minister". CNA. 25 April 2020. Archived from the original on 8 March 2021. Retrieved 23 April 2022.
- ↑ Kim ET (1 April 2020). "How South Korea Solved Its Face Mask Shortage". The New York Times. Archived from the original on 22 November 2021. Retrieved 23 April 2022.
- ↑ "Face masks mandatory on public transport". The Korea Herald. 25 May 2020. Archived from the original on 25 February 2021. Retrieved 23 April 2022.
- ↑ Sawer P (11 April 2020). "Spain to hand out free face masks for commuters to help return to work". The Daily Telegraph. Archived from the original on 26 April 2020. Retrieved 21 April 2020.
- ↑ Linde EG, Sevillano P (2 May 2020). "Sánchez anuncia la obligación de llevar mascarilla en el transporte público a partir del lunes". EL PAÍS (in español). Archived from the original on 21 February 2021. Retrieved 4 May 2020.
- ↑ "Press releases The Government approves the royal decree that establishes the measures that will govern the new normal". Ministerio de Sanidad. 9 June 2020. Archived from the original on 5 December 2020. Retrieved 23 April 2022.
- ↑ "Frågor och svar om covid-19 (coronavirus)" [Questions and answers regarding Covid-19 (corona virus)]. folkhalsomyndigheten.se (in svenska). Archived from the original on 30 November 2021. Retrieved 14 May 2020.
- ↑ Cederblad J. "Munskydd eller inte? – frågan vägrar försvinna" [Face masks or not? - the question is not going away]. Ny Teknik (in svenska). Archived from the original on 11 October 2021. Retrieved 11 June 2020.
- ↑ "Coronavirus: Does China have enough face masks to meet its needs?". BBC News Online. 6 February 2020. Archived from the original on 9 February 2020. Retrieved 10 February 2020.
- ↑ Ku C, Kao E (3 February 2020). "WUHAN VIRUS/Taiwan approves new rationing system for surgical masks". Central News Agency. Archived from the original on 5 February 2020. Retrieved 25 February 2020.
- ↑ Po-wei W, Wan-lin L, Lin K (9 March 2020). "Taiwan mask output to hit 10 million per day by next week: minister". Focus Taiwan. Archived from the original on 21 March 2020. Retrieved 23 April 2022.
- ↑ Everington K (1 April 2020). "Masks mandatory on Taiwan trains, inter-city buses starting today". Taiwan News. Archived from the original on 9 October 2021. Retrieved 23 April 2022.
- ↑ Lin C (4 April 2020). "Virus Outbreak: Fines authorized for unmasked riders". Taipei Times. Archived from the original on 7 April 2020. Retrieved 4 April 2020.
- ↑ Turkey mandates mask-wearing in all public areas Archived 4 March 2021 at the Wayback Machine, Anadolu Agency, 8 September 2020.
- ↑ Turkey implements uniform TL 900 fine for not wearing mask Archived 25 July 2021 at the Wayback Machine, Daily Sabah, 21 June 2020.
- ↑ "У масках – скрізь на вулиці, на в'їзді мірятимуть температуру. Нові обмеження в Києві". BBC Ukraine (in українська). 5 April 2020. Archived from the original on 6 April 2020. Retrieved 23 April 2022.
- ↑ "Coronavirus: Face coverings to be mandatory on public transport". BBC News. 4 June 2020. Archived from the original on 2 November 2021. Retrieved 23 April 2022.
- ↑ "Face coverings to be compulsory in England's shops". BBC News. 14 July 2020. Archived from the original on 13 September 2020. Retrieved 23 April 2022.
- ↑ "Face coverings: when to wear one, exemptions, and how to make your own". GOV.UK. Archived from the original on 1 August 2020. Retrieved 23 April 2022.
- ↑ "COVID-19: How are the rules on face masks and COVID passes changing in England?". Sky News. 9 December 2021. Archived from the original on 9 December 2021. Retrieved 9 December 2021.
- ↑ "Covid passes and face mask rules end in England". BBC News. 27 January 2022. Archived from the original on 29 January 2022. Retrieved 23 April 2022.
- ↑ McClafferty E (2 July 2020). "Coronavirus: Compulsory face coverings on buses, trains and ferries". BBC News. Archived from the original on 3 August 2020. Retrieved 24 July 2020.
- ↑ "Coronavirus: Face coverings could be mandatory in NI shops by 20 August". BBC News. 23 July 2020. Archived from the original on 20 October 2021. Retrieved 24 July 2020.
- ↑ "Coronavirus (COVID-19): face coverings". NI Direct. 2 July 2020. Archived from the original on 3 November 2021. Retrieved 8 June 2021.
- ↑ "Scottish government suggests covering face in shops". BBC News. 28 April 2020. Archived from the original on 15 May 2020. Retrieved 28 April 2020.
- ↑ "Face coverings mandatory on public transport from 22 June". Scottish Government. 18 June 2020. Archived from the original on 19 July 2021. Retrieved 8 June 2021.
- ↑ "Coronavirus: Face coverings to become mandatory in Scottish shops". BBC News. 2 July 2020. Archived from the original on 6 October 2020. Retrieved 8 June 2021.
- ↑ "Coronavirus: Face coverings now compulsory in Scotland's shops". BBC News. 10 July 2020. Archived from the original on 30 October 2021. Retrieved 8 June 2021.
- ↑ "Coronavirus (COVID-19) Phase 3: staying safe and protecting others". www.gov.scot. Archived from the original on 2 November 2020. Retrieved 23 April 2022.
- ↑ "Face masks to become mandatory in taxis and on public transport in Wales". ITV News. 14 July 2020. Archived from the original on 30 June 2021. Retrieved 24 July 2020.
- ↑ Smith M (24 July 2020). "Patients may be turned away from GP surgery in Cardiff if they don't wear a face mask". WalesOnline. Archived from the original on 23 December 2020. Retrieved 24 July 2020.
- ↑ "What Wales looked like on the first day masks were made mandatory". Wales Online. 14 September 2020. Archived from the original on 20 June 2021. Retrieved 8 June 2021.
- ↑ "Strategies for Optimizing the Supply of N95 Respirators: Crisis/Alternate Strategies". U.S. Centers for Disease Control and Prevention. 17 March 2020. Archived from the original on 25 May 2020. Retrieved 28 March 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention. 11 February 2020. Archived from the original on 27 November 2021. Retrieved 9 April 2020.
- ↑ Landsverk G (7 April 2020). "The CDC released a guide on how to make a face mask without sewing skills. Materials include a bandana, a coffee filter, and hair ties". Business Insider. Archived from the original on 12 September 2021. Retrieved 12 April 2020.
- ↑ "The States Where Face Coverings Are Mandatory". Axios. Archived from the original on 19 November 2021. Retrieved 12 August 2020.
- ↑ Marinucci C, Colliver V. "California requires masks statewide in bid to slow coronavirus spread". Politico PRO. Archived from the original on 15 October 2020. Retrieved 18 June 2020.
- ↑ Higgins-Dunn N (1 June 2020). "California Gov. Gavin Newsom orders residents to wear face coverings in most public spaces". CNBC. Archived from the original on 19 June 2020. Retrieved 18 June 2020.
- ↑ Sandoval E, Taylor K, Smith M (14 May 2021). "Federal Mask Retreat Sets Off Confusing Scramble for States and Cities". The New York Times. ISSN 0362-4331. Archived from the original on 28 October 2021. Retrieved 15 May 2021.
- ↑ "Maryland lifts mask mandate, along CDC guidelines | WTOP". wtop.com. Archived from the original on 31 March 2022. Retrieved 15 May 2021.
- ↑ "Virginia, Maryland lifting mask mandates Saturday". The Washington Post. ISSN 0190-8286. Archived from the original on 16 May 2021. Retrieved 15 May 2021.
- ↑ Afghanistan reports first coronavirus fatality, Uzbekistan makes protective masks mandatory Archived 20 April 2021 at the Wayback Machine, The Times of Central Asia, 23 March 2020.
- ↑ Walderrama S (20 March 2020). "Venezuelans sew homemade face masks amid coronavirus quarantine". Reuters. Archived from the original on 5 September 2021. Retrieved 23 April 2022.
- ↑ "All in Vietnam must wear face mask in public places for coronavirus prevention". The Star. 16 March 2020. Archived from the original on 4 September 2021. Retrieved 21 March 2020.
- ↑ Zambia records four new cases of Covid-19, total active now 20 Archived 31 July 2020 at the Wayback Machine, Daily Nation, 18 April 2020.
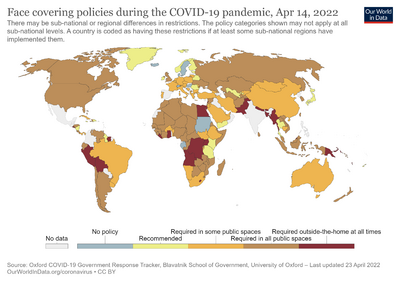

.jpg)

.jpg)

.jpg)
.jpg)
.jpg)
