| Part of a series on the |
| COVID-19 pandemic |
|---|
|
COVID-19 vaccine clinical research uses clinical research to establish the characteristics of COVID-19 vaccines. These characteristics include efficacy, effectiveness and safety. Thirty vaccines are authorized for use by national governments, including eight approved for emergency or full use by at least one WHO-recognised stringent regulatory authority; while five are in Phase IV. 204 vaccines are undergoing clinical trials that have yet to be authorized. Nine clinical trials consider heterologous vaccination courses.
Thirty vaccines are authorized by at least one national regulatory authority for public use:[1][2]
- one DNA vaccine: ZyCoV-D
- two RNA vaccines: Pfizer–BioNTech and Moderna
- eleven conventional inactivated vaccines: Chinese Academy of Medical Sciences, CoronaVac, Covaxin, CoviVac, COVIran Barekat, FAKHRAVAC, Minhai-Kangtai, QazVac, Sinopharm BIBP, WIBP, and Turkovac
- five viral vector vaccines: Sputnik Light, Sputnik V, Oxford–AstraZeneca, Convidecia, and Janssen
- eleven subunit vaccines: Abdala, Corbevax, COVAX-19, EpiVacCorona, MVC-COV1901, Novavax, Razi Cov Pars, Sinopharm CNBG, Soberana 02, Soberana Plus, and ZF2001.
As of July 2021, 330 vaccine candidates were in various stages of development, with 102 in clinical research, including 30 in Phase I trials, 30 in Phase I–II trials, 25 in Phase III trials, and 8 in Phase IV development.[1]
Formulation[edit | edit source]
As of September 2020[update], eleven of the vaccine candidates in clinical development use adjuvants to enhance immunogenicity.[3] Adjuvants are substances that elevate the immune response to a vaccine.[4] Specifically, an adjuvant may be used to boost a vaccine's efficacy.[4][5] COVID‑19 vaccine adjuvant formulation may be particularly effective for technologies using the inactivated COVID‑19 virus and recombinant protein-based or vector-based vaccines. Aluminum salts, known as "alum", were the first adjuvant added to licensed vaccines, and are the adjuvant of choice in some 80% of adjuvanted vaccines.[5] The alum adjuvant initiates diverse molecular and cellular mechanisms to enhance immunogenicity, including release of proinflammatory cytokines.[4][5]
Status[edit | edit source]
Clinical trials[edit | edit source]
The clinical trial process typically consists of three phases, each following the success of the prior phase. Trials are doubly blind in that neither the researcher nor the subject know whether they receive the vaccine or a placebo. Each phase involves randomly-selected subjects who are randomly assigned to serve either as recipients are controls:
- Phase I trials test primarily for safety and preliminary dosing in healthy subjects. Dozens of subjects.
- Phase II trials evaluate immunogenicity, dose levels (efficacy based on biomarkers) and adverse effects.[6][7] Hundreds of subjects. Sometimes Phase I and II trials are combined.[7]
- Phase III trials typically involve more participants at multiple sites, include a control group, and test effectiveness of the vaccine to prevent the disease (an "interventional" or "pivotal" trial), while monitoring for adverse effects at the selected dose.[6][7] Safety, efficacy, and clinical endpoints may vary, including the definition of side effects, infection or amount of transmission, and whether the vaccine prevents moderate or severe infection.[8][9][10]
A clinical trial design in progress may adopt an "adaptive design". If accumulating data provide insights about the treatment, the endpoints or other aspects or the trial can be adjusted.[11][12] Adaptive designs may shorten trial durations and use fewer subjects, possibly expediting decisions, avoiding duplication of research efforts, and enhancing coordination of design changes.[11][13]
List of authorized and approved vaccines[edit | edit source]
National regulatory authorities have granted emergency use authorizations for twenty-two vaccines. Eight of those have been approved for emergency or full use by at least one WHO-recognized stringent regulatory authority. Biologic License Applications for the Pfizer–BioNTech and Moderna COVID‑19 vaccines have been submitted to the US Food and Drug Administration (FDA).[14][15]
The table below shows various vaccines authorized either for full or emergency use so far, with various other details.
| COVID-19 vaccines authorized for emergency use or approved for full use |
| Template:COVID-19 vaccine authorizations |
Vaccine candidates in human trials[edit | edit source]
The table below shows various vaccine candidates and the phases which they have completes so far. Current phases are also shown along with other details.
| COVID‑19 candidate vaccines in Phase I–III trials | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
Homologous prime-boost vaccination[edit | edit source]
In July 2021, the U.S. Food and Drug Administration (FDA) and the Centers for Disease Control and Prevention (CDC) issued a joint statement reporting that a booster dose is not necessary for those who have been fully vaccinated.[314]
In August 2021, the FDA and the CDC authorized the use of an additional mRNA vaccine dose for immunocompromised individuals.[315][316] The authorization was extended to cover other specific groups in September 2021.[317][318][319]
In October 2021, the FDA and the CDC authorized the use of either homologous or heterologous vaccine booster doses.[320][321]
Heterologous prime-boost vaccination[edit | edit source]
The World Health Organization (WHO) defines heterologous prime-boost immunization as the administration of two different vectors or delivery systems expressing the same or overlapping antigenic inserts.
[322] A heterologous scheme can sometimes be more immunogenic than some homologous schemes.[323]
In October 2021, the FDA and the CDC authorized the use of either homologous or heterologous vaccine booster doses.[320][321]
Some experts believe that heterologous prime-boost vaccination courses can boost immunity, and several studies have begun to examine this effect.[324] Despite the absence of clinical data on the efficacy and safety of such heterologous combinations, Canada and several European countries have recommended a heterologous second dose for people who have received the first dose of the Oxford–AstraZeneca vaccine.[325]
In February 2021, the Oxford Vaccine Group launched the Com-COV vaccine trial to investigate heterologous prime-boost courses of different COVID-19 vaccines.[326] As of June 2021, the group is conducting two phase II studies: Com-COV and Com-COV2.[327]
In Com-COV, the two heterologous combinations of the Oxford–AstraZeneca and Pfizer–BioNTech vaccines were compared with the two homologous combinations of the same vaccines, with an interval of 28 or 84 days between doses.[328][329][unreliable medical source?]
In Com-COV2, the first dose is the Oxford–AstraZeneca vaccine or the Pfizer vaccine, and the second dose is the Moderna vaccine, the Novavax vaccine, or a homologous vaccine equal to the first dose, with an interval of 56 or 84 days between doses.[330]
A study in the UK is evaluating annual heterologous boosters by randomly combining the following vaccines: Oxford–AstraZeneca, Pfizer–BioNTech, Moderna, Novavax, VLA2001, CureVac, and Janssen.[331]
On December 16, WHO recommendations on heterologous vaccinations suggested a general trend of increased immunogenicity when one of the doses is of an mRNA vaccine, particularly as the last dose. The immunogenicity of a homologous mRNA course is roughly equivalent to a heterologous scheme involving a vector vaccine and an mRNA vaccine. However, the WHO has emphasized the need to address many evidence gaps in heterologous regimens, including duration of protection, optimal interval between doses, influence of fractional dosing, effectiveness against variants and long-term safety.[332]
| First dose | Second dose | Schedules | Current phase (participants), periods and locations |
|---|---|---|---|
| Oxford–AstraZeneca Pfizer–BioNTech |
Oxford–AstraZeneca Pfizer–BioNTech |
Days 0 and 28 Days 0 and 84 |
Phase II (820) Feb–Aug 2021, United Kingdom |
| Sputnik Light | Oxford–AstraZeneca Moderna Sinopharm BIBP |
Phase II (121) Feb–Aug 2021, Argentina | |
| Oxford–AstraZeneca Pfizer–BioNTech |
Oxford–AstraZeneca Pfizer–BioNTech Moderna Novavax |
Days 0 and 56–84 | Phase II (1,050) Mar 2021 – Sep 2022, United Kingdom |
| Convidecia | ZF2001 | Days 0 and 28 Days 0 and 56 |
Phase IV (120) Apr–Dec 2021, China |
| Oxford–AstraZeneca | Pfizer–BioNTech | Days 0 and 28 | Phase II (676) Apr 2021 – Apr 2022, Spain |
| Oxford–AstraZeneca Pfizer–BioNTech Moderna |
Pfizer–BioNTech Moderna |
Days 0 and 28 Days 0 and 112 |
Phase II (1,200) May 2021 – Mar 2023, Canada |
| Pfizer–BioNTech Moderna |
Pfizer–BioNTech Moderna |
Days 0 and 42 | Phase II (400) May 2021 – Jan 2022, France |
| Oxford–AstraZeneca | Pfizer–BioNTech | Days 0 and 28 Days 0 and 21–49 |
Phase II (3,000) May–Dec 2021, Austria |
| Janssen | Pfizer–BioNTech Janssen Moderna |
Days 0 and 84 | Phase II (432) Jun 2021 – Sep 2022, Netherlands |
| Initial course | Booster dose | Interval | Current phase (participants), periods and locations |
|---|---|---|---|
| CoronaVac (2 doses) | CoronaVac Pfizer–BioNTech Oxford–AstraZeneca |
19 weeks or more | Phase IV (2,017,878) Aug–Nov 2021, Chile |
Efficacy[edit | edit source]
<section begin=excerpt/>
Vaccine efficacy is the reduction in risk of getting the disease by vaccinated participants in a controlled trial compared with the risk of getting the disease by unvaccinated participants.[343] An efficacy of 0% means that the vaccine does not work (identical to placebo). An efficacy of 50% means that there are half as many cases of infection as in unvaccinated individuals.[citation needed]
COVID-19 vaccine efficacy may be adversely affected if the arm is held improperly or squeezed so the vaccine is injected subcutaneously instead of into the muscle.[344][345] The CDC guidance is to not repeat doses that are administered subcutaneously.[346]
It is not straightforward to compare the efficacies of the different vaccines because the trials were run with different populations, geographies, and variants of the virus.[347] In the case of COVID‑19 prior to the advent of the delta variant, it was thought that a vaccine efficacy of 67% may be enough to slow the pandemic, but the current vaccines do not confer sterilizing immunity,[348] which is necessary to prevent transmission. Vaccine efficacy reflects disease prevention, a poor indicator of transmissibility of SARS‑CoV‑2 since asymptomatic people can be highly infectious.[349] The US Food and Drug Administration (FDA) and the European Medicines Agency (EMA) set a cutoff of 50% as the efficacy required to approve a COVID‑19 vaccine, with the lower limit of the 95% confidence interval being greater than 30%.[350][351][352] Aiming for a realistic population vaccination coverage rate of 75%, and depending on the actual basic reproduction number, the necessary effectiveness of a COVID-19 vaccine is expected to need to be at least 70% to prevent an epidemic and at least 80% to extinguish it without further measures, such as social distancing.[353]<section end=excerpt/>
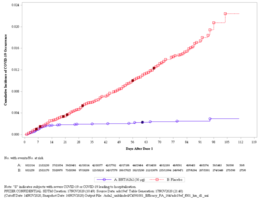
The observed substantial efficacy of certain mRNA vaccines even after partial (1-dose) immunization[354][342] indicates a non-linear dose-efficacy relation already seen in the phase I-II study[355] and suggests that personalization of the vaccine dose (regular dose to the elderly, reduced dose to the healthy young,[356] additional booster dose to the immunosuppressed[357]) might allow accelerating vaccination campaigns in settings of limited supplies, thereby shortening the pandemic, as predicted by pandemic modeling.[358]
Ranges below are 95% confidence intervals unless indicated otherwise, and all values are for all participants regardless of age, according to the references for each of the trials. By definition, the accuracy of the estimates without an associated confidence interval is unknown publicly. Efficacy against severe COVID-19 is the most important, since hospitalizations and deaths are a public health burden whose prevention is a priority.[359] Authorized and approved vaccines have shown the following efficacies:
| COVID-19 vaccine efficacy |
|
Effectiveness[edit | edit source]
As of August 2021, studies reported that the COVID-19 vaccines available in the United States are "highly protective against severe illness, hospitalization, and death due to COVID-19".[394] In comparison with fully vaccinated people, the CDC reported that unvaccinated people were 5 times more likely to be infected, 10 times more likely to be hospitalized, and 11 times more likely to die.[395][396]
Another study found that unvaccinated people were six times more likely to test positive, 37 times more likely to be hospitalized, and 67 times more likely to die, compared to those who had been vaccinated.[397]
CDC reported that vaccine effectiveness fell from 91% against Alpha to 66% against Delta.[398] One expert stated that "those who are infected following vaccination are still not getting sick and not dying like was happening before vaccination."[399] By late August 2021 the Delta variant accounted for 99 percent of U.S. cases and was found to double the risk of severe illness and hospitalization for those not yet vaccinated.[400]
On 10 December 2021, the UK Health Security Agency reported that early data indicated a 20- to 40-fold reduction in neutralizing activity for Omicron by sera from Pfizer 2-dose vaccinees relative to earlier strains. After a booster dose (usually with an mRNA vaccine),[401] vaccine effectiveness against symptomatic disease was at 70%–75%, and the effectiveness against severe disease was expected to be higher.[402]
Studies[edit | edit source]
Real-world studies of vaccine effectiveness measure the extent to which a certain vaccine prevents infection, symptoms, hospitalization and death for the vaccinated individuals in a large population under routine conditions.[403]
- In Israel, among the 715,425 individuals vaccinated by the mRNA vaccines from 20 December 2020, to 28 January 2021, starting seven days after the second shot, only 317 people (0.04%) displayed mild/moderate COVID-19 symptoms and only 16 people (0.002%) were hospitalized.[404]
- CDC reported that under real-world conditions, mRNA vaccine effectiveness was 90% against infections regardless of symptom status; while effectiveness of partial immunization was 80%.[405]
- In the UK, 15,121 health care workers from 104 hospitals who had tested negative for antibodies prior to the study, were followed by RT-PCR tests twice a week from 7 December 2020 to 5 February 2021, a study compared the positive results for the 90.7% vaccinated share of their cohort with the 9.3% unvaccinated share, and found that the Pfizer-BioNTech vaccine reduced all infections (including asymptomatic), by 72% (58–86%) three weeks after the first dose and 86% (76–97%) one week after the second dose, while Alpha was dominant.[406][needs update]
- In Israel a study conducted from 17 January to 6 March 2021, found that Pfizer/BioNTech reduced asymptomatic Alpha infections by 94% and symptomatic COVID-19 infections by 97%.[407]
- A study among pre-surgical patients across the Mayo Clinic system in the United States, showed that mRNA vaccines were 80% protective against asymptomatic infections.[408]
- A UK study found that a single dose of the Oxford–AstraZeneca COVID-19 vaccine is about 73% (27–90%) effective in people aged 70 and older.[409]
| Vaccine | Initial effectiveness by severity of COVID-19 | Study location | Refs | |||
|---|---|---|---|---|---|---|
| Asymptomatic | Symptomatic | Hospitalization | Death | |||
| Oxford–AstraZeneca | 70% (69–71%) | Not reported | 87% (85–88%) | 90% (88–92%) | Brazil | [410] |
| Not reported | 89% (78–94%)[lower-roman 1] | Not reported | Not reported | England | [412] | |
| Not reported | Not reported | Not reported | 89%[lower-roman 2] | Argentina | [413] | |
| 72% (69–74%) | Not reported | Not reported | 88% (79–94%) | Hungary | [414] | |
| Pfizer–BioNTech | 92% (91–92%) | 97% (97–97%) | 98% (97–98%) | 97% (96–97%) | Israel | [415] |
| 92% (88–95%) | 94% (87–98%) | 87% (55–100%) | 97%[lower-roman 2] | Israel | [416][417] | |
| 83% (83–84%) | Not reported | Not reported | 91% (89–92%) | Hungary | [414] | |
| Not reported | 78% (77–79%) | 98% (96–99%) | 96% (95–97%) | Uruguay | [418] | |
| 85% (74–96%) | Not reported | Not reported | England | [419] | ||
| 90% (68–97%) | Not reported | 100%[lower-roman 2][lower-roman 3] | United States | [420] | ||
| Moderna | 89% (87–90%) | Not reported | Not reported | 94% (91–96%) | Hungary | [414] |
| 90% (68–97%) | Not reported | 100%[lower-roman 2][lower-roman 3] | United States | [420] | ||
| Sinopharm BIBP | Not reported | Not reported | Not reported | 84%[lower-roman 2] | Argentina | [413] |
| 69% (67–70%) | Not reported | Not reported | 88% (86–89%) | Hungary | [414] | |
| 50% (49–52%) | Not reported | Not reported | 94% (91–96%) | Peru | [421] | |
| Sputnik V | Not reported | 98%[lower-roman 2] | Not reported | Not reported | Russia | [422][423] |
| Not reported | 98%[lower-roman 2] | 100%[lower-roman 2][lower-roman 3] | 100%[lower-roman 2][lower-roman 3] | United Arab Emirates | [424] | |
| Not reported | Not reported | Not reported | 93%[lower-roman 2] | Argentina | [413] | |
| 86% (84–87%) | Not reported | Not reported | 98% (96–99%) | Hungary | [414] | |
| CoronaVac | 54% (53–55%) | Not reported | 73% (72–74%) | 74% (73–75%) | Brazil | [410] |
| Not reported | 66% (65–67%) | 88% (87–88%) | 86% (85–88%) | Chile | [425][426] | |
| Not reported | 60% (59–61%) | 91% (89–93%) | 95% (93–96%) | Uruguay | [418] | |
| Not reported | 94%[lower-roman 2] | 96%[lower-roman 2] | 98%[lower-roman 2] | Indonesia | [427][428] | |
| Not reported | 80%[lower-roman 2] | 86%[lower-roman 2] | 95%[lower-roman 2] | Brazil | [429][430] | |
| Sputnik Light | 79% (75–82%)[lower-roman 2][lower-roman 4] | Not reported | 88% (80–92%)[lower-roman 2][lower-roman 4] | 85% (75–91%)[lower-roman 2][lower-roman 4] | Argentina | [431] |
- ↑ Data collected while the Alpha variant was already dominant.[411]
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 A confidence interval was not provided, so it is not possible to know the accuracy of this measurement.
- ↑ 3.0 3.1 3.2 3.3 No cases detected in study.
- ↑ 4.0 4.1 4.2 Participants aged 60 to 79.
| Initial course | Booster dose | Initial effectiveness by severity of COVID-19 | Study location | Refs | |||
|---|---|---|---|---|---|---|---|
| Asymptomatic | Symptomatic | Hospitalization | Death | ||||
| CoronaVac | CoronaVac | Not reported | 80%[upper-roman 1] | 88%[upper-roman 1] | Not reported | Chile | [432] |
| Pfizer–BioNTech | Not reported | 90%[upper-roman 1] | 87%[upper-roman 1] | Not reported | Chile | [432] | |
| Oxford–AstraZeneca | Not reported | 93%[upper-roman 1] | 96%[upper-roman 1] | Not reported | Chile | [432] | |
Critical coverage[edit | edit source]
While the most immediate goal of vaccination during a pandemic is to protect individuals from severe disease, a long-term goal is to eventually eradicate it. To do so, the proportion of the population that must be immunized must be greater than the critical vaccination coverage . This value can be calculated from the basic reproduction number and the vaccine effectiveness against transmission as:[433]
Assuming R0 ≈ 2.87 for SARS-CoV-2,[434] then, for example, the coverage level would have to be greater than 72.4% for a vaccine that is 90% effective against transmission. Using the same relationship, the required effectiveness against transmission can be calculated as:
Assuming the same R0 ≈ 2.87, the effectiveness against transmission would have to be greater than 86.9% for a realistic coverage level of 75%[353] or 65.2% for an impossible coverage level of 100%. Less effective vaccines would not be able to eradicate the disease.
Several post-marketing studies have already estimated the effectiveness of some vaccines against asymptomatic infection. Prevention of infection has an impact on slowing transmission (particularly asymptomatic and pre-symptomatic), but the exact extent of this effect is still under investigation.[435]
Some variants of SARS-CoV-2 are more transmissible, showing an increased effective reproduction number, indicating an increased basic reproduction number. Controlling them requires greater vaccine coverage, greater vaccine effectiveness against transmission, or a combination of both.
In July 2021, several experts expressed concern that achieving herd immunity may not currently be possible because the Delta variant is transmitted among those immunized with current vaccines.[436] The CDC published data showing that vaccinated people could transmit the Delta variant, something officials believed was not possible with other variants.[437]
Variants[edit | edit source]
The interplay between the SARS-CoV-2 virus and its human hosts was initially natural but is now being altered by the prompt availability of vaccines.[438] The potential emergence of a SARS-CoV-2 variant that is moderately or fully resistant to the antibody response elicited by the COVID-19 vaccines may necessitate modification of the vaccines.[439] The emergence of vaccine-resistant variants is more likely in a highly vaccinated population with uncontrolled transmission.[440] Trials indicate many vaccines developed for the initial strain have lower efficacy for some variants against symptomatic COVID-19.[441] As of February 2021[update], the US Food and Drug Administration believed that all FDA authorized vaccines remained effective in protecting against circulating strains of SARS-CoV-2.[439]
Alpha (lineage B.1.1.7)[edit | edit source]
Limited evidence from various preliminary studies reviewed by the WHO indicated retained efficacy/effectiveness against disease from Alpha with the Oxford–AstraZeneca vaccine, Pfizer–BioNTech and Novavax, with no data for other vaccines yet. Relevant to how vaccines can end the pandemic by preventing asymptomatic infection, they have also indicated retained antibody neutralization against Alpha with most of the widely distributed vaccines (Sputnik V, Pfizer–BioNTech, Moderna, CoronaVac, Sinopharm BIBP, Covaxin), minimal to moderate reduction with the Oxford–AstraZeneca and no data for other vaccines yet.[442]
In December 2020, a new SARS‑CoV‑2 variant, the Alpha variant or lineage B.1.1.7, was identified in the UK.[443]
Early results suggest protection to the variant from the Pfizer-BioNTech and Moderna vaccines.[444][445]
One study indicated that the Oxford–AstraZeneca COVID-19 vaccine had an efficacy of 42–89% against Alpha, versus 71–91% against other variants.[446][unreliable medical source?]
Preliminary data from a clinical trial indicates that the Novavax vaccine is ~96% effective for symptoms against the original variant and ~86% against Alpha.[447]
Beta (lineage B.1.351)[edit | edit source]
Limited evidence from various preliminary studies reviewed by the WHO have indicated reduced efficacy/effectiveness against disease from Beta with the Oxford–AstraZeneca vaccine (possibly substantial), Novavax (moderate), Pfizer–BioNTech and Janssen (minimal), with no data for other vaccines yet. Relevant to how vaccines can end the pandemic by preventing asymptomatic infection, they have also indicated possibly reduced antibody neutralization against Beta with most of the widely distributed vaccines (Oxford–AstraZeneca, Sputnik V, Janssen, Pfizer–BioNTech, Moderna, Novavax; minimal to substantial reduction) except CoronaVac and Sinopharm BIBP (minimal to modest reduction), with no data for other vaccines yet.[442]
Moderna has launched a trial of a vaccine to tackle the Beta variant or lineage B.1.351.[448] On 17 February 2021, Pfizer announced neutralization activity was reduced by two-thirds for this variant, while stating that no claims about the efficacy of the vaccine in preventing illness for this variant could yet be made.[449] Decreased neutralizing activity of sera from patients vaccinated with the Moderna and Pfizer-BioNTech vaccines against Beta was later confirmed by several studies.[445][450] On 1 April 2021, an update on a Pfizer/BioNTech South African vaccine trial stated that the vaccine was 100% effective so far (i.e., vaccinated participants saw no cases), with six of nine infections in the placebo control group being the Beta variant.[451]
In January 2021, Johnson & Johnson, which held trials for its Janssen vaccine in South Africa, reported the level of protection against moderate to severe COVID-19 infection was 72% in the United States and 57% in South Africa.[452]
On 6 February 2021, the Financial Times reported that provisional trial data from a study undertaken by South Africa's University of the Witwatersrand in conjunction with Oxford University demonstrated reduced efficacy of the Oxford–AstraZeneca COVID-19 vaccine against the variant.[453] The study found that in a sample size of 2,000 the AZD1222 vaccine afforded only "minimal protection" in all but the most severe cases of COVID-19.[454] On 7 February 2021, the Minister for Health for South Africa suspended the planned deployment of about a million doses of the vaccine whilst they examine the data and await advice on how to proceed.[454][455]
In March 2021, it was reported that the "preliminary efficacy" of the Novavax vaccine (NVX-CoV2373) against Beta for mild, moderate, or severe COVID-19[456] for HIV-negative participants is 51%.[medical citation needed]
Gamma (lineage P.1)[edit | edit source]
Limited evidence from various preliminary studies reviewed by the WHO have indicated likely retained efficacy/effectiveness against disease from Gamma with CoronaVac and Sinopharm BIBP, with no data for other vaccines yet. Relevant to how vaccines can end the pandemic by preventing asymptomatic infection, they have also indicated retained antibody neutralization against Gamma with Oxford–AstraZeneca and CoronaVac (no to minimal reduction) and slightly reduced neutralization with Pfizer–BioNTech and Moderna (minimal to moderate reduction), with no data for other vaccines yet.[442]
The Gamma variant or lineage P.1 variant (also known as 20J/501Y.V3), initially identified in Brazil, seems to partially escape vaccination with the Pfizer-BioNTech vaccine.[450]
Delta (lineage B.1.617.2)[edit | edit source]
Limited evidence from various preliminary studies reviewed by the WHO have indicated likely retained efficacy/effectiveness against disease from Delta with the Oxford–AstraZeneca vaccine and Pfizer–BioNTech, with no data for other vaccines yet. Relevant to how vaccines can end the pandemic by preventing asymptomatic infection, they have also indicated reduced antibody neutralization against Delta with single-dose Oxford–AstraZeneca (substantial reduction), Pfizer–BioNTech and Covaxin (modest to moderate reduction), with no data for other vaccines yet.[442]
In October 2020, a new variant was discovered in India, which was named lineage B.1.617. There were very few detections until January 2021, but by April it had spread to at least 20 countries in all continents except Antarctica and South America.[457][458][459] Mutations present in the spike protein in the B.1.617 lineage are associated with reduced antibody neutralization in laboratory experiments.[460][461] The variant has frequently been referred to as a 'Double mutant', even though in this respect it is not unusual.[462] the latter two of which may cause it to easily avoid antibodies.[463] In an update on 15 April 2021, PHE designated lineage B.1.617 as a 'Variant under investigation', VUI-21APR-01.[464] On 6 May 2021, Public Health England escalated lineage B.1.617.2 from a Variant Under Investigation to a Variant of Concern based on an assessment of transmissibility being at least equivalent to the Alpha variant.[465]
Effect of neutralizing antibodies[edit | edit source]
One study found that the in vitro concentration (titer) of neutralizing antibodies elicited by a COVID-19 vaccine is a strong correlate of immune protection. The relationship between protection and neutralizing activity is nonlinear. A neutralization as low as 3% (95% CI, 1–13%) of the level of convalescence results in 50% efficacy against severe disease, with 20% (14–28%) resulting in 50% efficacy against detectable infection. Protection against infection quickly decays, leaving individuals susceptible to mild infections, while protection against severe disease is largely retained and much more durable. The observed half-life of neutralizing titers was 65 days for mRNA vaccines (Pfizer–BioNTech, Moderna) during the first 4 months, increasing to 108 days over 8 months. Greater initial efficacy against infection likely results in a higher level of protection against serious disease in the long term (beyond 10 years, as seen in other vaccines such as smallpox, measles, mumps, and rubella), although the authors acknowledge that their simulations consider only protection from neutralizing antibodies and ignore other immune protection mechanisms, such as cell-mediated immunity, which may be more durable. This observation also applies to efficacy against variants and is particularly significant for vaccines with a lower initial efficacy; for example, a 5-fold reduction in neutralization would indicate a reduction in initial efficacy from 95% to 77% against a specific variant, and from a lower efficacy of 70% to 32% against that variant. For the Oxford–AstraZeneca vaccine, the observed efficacy is below the predicted 95% confidence interval. It is higher for Sputnik V and the convalescent response, and is within the predicted interval for the other vaccines evaluated (Pfizer–BioNTech, Moderna, Janssen, CoronaVac, Covaxin, Novavax).[466]
Side effects[edit | edit source]
Serious adverse events associated with vaccines are of high interest to the public.[467] All vaccines have side effects related to the mild trauma associated with the introduction of a foreign substance into the body.[468] These include soreness, redness, rash, and inflammation at the injection site. Other common side effects include fatigue, headache, myalgia (muscle pain), and arthralgia (joint pain) which generally resolve within a few days.[469] One less-frequent side effect (that generally occurs in less than 1 in 1,000 people) is hypersensitivity (allergy) to one or more of the vaccine's ingredients, which in some rare cases may cause anaphylaxis.[470][471][472][473] More serious side effects are very rare because a vaccine would not be approved even for emergency use if it had any known frequent serious adverse effects.[citation needed]
Reporting[edit | edit source]
Most countries operate some form of adverse effects reporting scheme, for example Vaccine Adverse Event Reporting System in the United States and the Yellow Card Scheme[474] in the United Kingdom. In some of these, the data is open to public scrutiny. For example, the UK publishes a weekly summary report.[475] Concerns have been raised regarding both over-[476] and under-reporting[citation needed] of adverse effects.
UK[edit | edit source]
In the UK, as of 22 September 2021, following the administering of over 48 million first vaccine doses and over 44 million second vaccine doses, there had been 347,447 suspected COVID-19 vaccine related events ('suspected adverse reactions', or 'ADRs') recorded in the Yellow Card system. The majority of these were reports of relatively minor effects (local reactions or temporary flu-like symptoms). Among more serious ADRs, the largest case load came from suspected thrombo-embolic events, of which a total of 439 were recorded, 74 of these fatal.[475] A total of 1,682 suspected fatal ADRs were recorded.[475] For comparison, at this date, the UK had had over 7,500,000 confirmed cases of COVID-19 and over 136,000 people had died within 28 days of a positive test for coronavirus.[475]
Blood lcots[edit | edit source]
Rare formation of blood clots in the blood vessels were reported following Janssen vaccine injections in combination with low levels of blood platelets known as thrombosis with thrombocytopenia syndrome (TTS) which occurred at a rate of about 7 per 1 million vaccinated women ages 18–49 years old; and less often for other populations.[477] According to the U.S. Centers for Disease Control and Prevention (CDC), cases of myocarditis and pericarditis have been reported in about 13 per million young people (mostly in males and mostly over the age of 16), in association with the mRNA vaccines.[478] According to reports, the recovery from these side effects is quick in most individuals, following treatment and rest.[479]
Blood cancers[edit | edit source]
A study on the serologic response to mRNA vaccines among patients with lymphoma, leukemia and myeloma found that one-quarter of patients did not produce measurable antibodies, varying by cancer type.[480]
References[edit | edit source]
- ↑ 1.0 1.1 "COVID-19 vaccine tracker (Refresh URL to update)". vac-lshtm.shinyapps.io. London School of Hygiene & Tropical Medicine. 12 July 2021. Retrieved 10 March 2021.
- ↑ "Approved Vaccines". COVID 19 Vaccine Tracker, McGill University. 12 July 2021.
- ↑ Le TT, Cramer JP, Chen R, Mayhew S (October 2020). "Evolution of the COVID-19 vaccine development landscape". Nature Reviews. Drug Discovery. 19 (10): 667–68. doi:10.1038/d41573-020-00151-8. PMID 32887942. S2CID 221503034.
- ↑ 4.0 4.1 4.2 Tregoning JS, Russell RF, Kinnear E (March 2018). "Adjuvanted influenza vaccines". Human Vaccines & Immunotherapeutics. 14 (3): 550–64. doi:10.1080/21645515.2017.1415684. PMC 5861793. PMID 29232151.
- ↑ 5.0 5.1 5.2 Wang J, Peng Y, Xu H, Cui Z, Williams RO (August 2020). "The COVID-19 Vaccine Race: Challenges and Opportunities in Vaccine Formulation". AAPS PharmSciTech. 21 (6): 225. doi:10.1208/s12249-020-01744-7. PMC 7405756. PMID 32761294.
- ↑ 6.0 6.1 "Vaccine Safety – Vaccines". US Department of Health and Human Services. Archived from the original on 22 April 2020. Retrieved 13 April 2020.
- ↑ 7.0 7.1 7.2 "The drug development process". U.S. Food and Drug Administration (FDA). 4 January 2018. Archived from the original on 22 February 2020. Retrieved 12 April 2020.
- ↑ Cohen J (June 2020). "Pandemic vaccines are about to face the real test". Science. 368 (6497): 1295–96. Bibcode:2020Sci...368.1295C. doi:10.1126/science.368.6497.1295. PMID 32554572.
- ↑ "How flu vaccine effectiveness and efficacy are measured". U.S. Centers for Disease Control and Prevention (CDC). 29 January 2016. Archived from the original on 7 May 2020. Retrieved 6 May 2020.
- ↑ "Principles of epidemiology, Section 8: Concepts of disease occurrence". U.S. Centers for Disease Control and Prevention (CDC). 18 May 2012. Archived from the original on 6 April 2020. Retrieved 6 May 2020.
- ↑ 11.0 11.1 Pallmann P, Bedding AW, Choodari-Oskooei B, Dimairo M, Flight L, Hampson LV, et al. (February 2018). "Adaptive designs in clinical trials: why use them, and how to run and report them". BMC Medicine. 16 (1): 29. doi:10.1186/s12916-018-1017-7. PMC 5830330. PMID 29490655.
- ↑ "Adaptive designs for clinical trials of drugs and biologics: Guidance for industry" (PDF). U.S. Food and Drug Administration (FDA). 1 November 2019. Archived from the original on 13 December 2019. Retrieved 3 April 2020.
- ↑ "An international randomised trial of candidate vaccines against COVID-19: Outline of Solidarity vaccine trial" (PDF). World Health Organization (WHO). 9 April 2020. Archived (PDF) from the original on 12 May 2020. Retrieved 9 May 2020.
- ↑ "Pfizer and BioNTech Initiate Rolling Submission of Biologics License Application for U.S. FDA Approval of Their COVID 19 Vaccine". Pfizer (Press release). 7 May 2021. Archived from the original on 9 June 2021. Retrieved 9 June 2021.
- ↑ "Moderna Announces Initiation of Rolling Submission of Biologics License Application (BLA) with U.S. FDA for the Moderna COVID-19 Vaccine" (Press release). Moderna. 1 June 2021. Archived from the original on 9 June 2021. Retrieved 9 June 2021 – via Business Wire.
- ↑ "COVID-19 vaccine tracker (Refresh URL to update)". vac-lshtm.shinyapps.io. London School of Hygiene & Tropical Medicine. 12 July 2021. Retrieved 10 March 2021.
- ↑ "COVID-19 vaccine tracker (Choose vaccines tab, apply filters to view select data)". Milken Institute. 8 December 2020. Retrieved 11 December 2020.
- ↑ "Draft landscape of COVID 19 candidate vaccines". World Health Organization (WHO). 10 December 2020. Retrieved 11 December 2020.
- ↑ "Study of Monovalent and Bivalent Recombinant Protein Vaccines Against COVID-19 in Adults 18 Years of Age and Older (VAT00008)". ClinicalTrials.gov. 27 May 2021. NCT04904549. Retrieved 28 May 2021.
- ↑ "Safety and efficacy of Monovalent and Bivalent Recombinant Protein Vaccines against COVID-19 in Adults 18 Years of Age and Older". ctri.nic.in. Clinical Trials Registry India. CTRI/2021/06/034442. Retrieved 3 August 2021.
- ↑ "Study of Recombinant Protein Vaccine with Adjuvant against COVID-19 in Adults 18 Years of Age and Older". pactr.samrc.ac.za. Pan African Clinical Trials Registry. Retrieved 24 March 2021.
- ↑ "Tarjeta del participante del estudio VAT00008: ejemplo central para adaptación a nivel de país" [VAT00008 Study Participant Card: Central Example for Country-Level Adaptation] (PDF). incmnsz.mx. Salvador Zubirán National Institute of Health Sciences and Nutrition. 15 April 2021.
- ↑ "Study of Recombinant Protein Vaccine Formulations Against COVID-19 in Healthy Adults 18 Years of Age and Older". ClinicalTrials.gov. 3 September 2020. NCT04537208. Retrieved 11 March 2021.
- ↑ "Study of Recombinant Protein Vaccine With Adjuvant Against COVID-19 in Adults 18 Years of Age and Older (VAT00002)". ClinicalTrials.gov. 21 February 2021. NCT04762680. Retrieved 11 March 2021.
- ↑ "Sanofi and GSK confirm agreement with European Union to supply up to 300 million doses of adjuvanted COVID-19 vaccine". GSK (Press release). Retrieved 1 April 2021.
- ↑ https://www.ema.europa.eu/en/human-regulatory/overview/public-health-threats/coronavirus-disease-covid-19/treatments-vaccines/vaccines-covid-19/covid-19-vaccines-under-evaluation
- ↑ "Sanofi and GSK sign agreements with the Government of Canada to supply up to 72 million doses of adjuvanted COVID-19 vaccine". GSK (Press release). Retrieved 1 April 2021.
- ↑ "U.S. Likely to Get Sanofi Vaccine First If It Succeeds". Bloomberg.com. 13 May 2020. Retrieved 1 April 2021.
- ↑ "Coronavirus vaccine: UK signs deal with GSK and Sanofi". BBC News Online. 29 July 2020. Retrieved 1 April 2021.
- ↑ 30.0 30.1 "Status of COVID-19 Vaccines within WHO EUL/PQ evaluation process". World Health Organization (WHO).
- ↑ "VN starts injection of homegrown COVID-19 vaccine in first-stage human trial". Viet Nam News. 17 December 2020.
- ↑ "Draft landscape and tracker of COVID-19 candidate vaccines". World Health Organization (WHO). 26 February 2021.
- ↑ "How much does first Made-in Vietnam COVID-19 vaccine cost?". Voice of Vietnam. 11 December 2020.
- ↑ "Local Nanocovax vaccine's phase 3 trial to begin next week". vietnamnet.vn. 26 May 2021. Retrieved 28 May 2021.
- ↑ "Study to Evaluate the Safety, Immunogenicity, and Efficacy of Nanocovax Vaccine Against COVID-19". ClinicalTrials.gov. 11 June 2021. NCT04922788. Retrieved 11 June 2021.
- ↑ Le C, Thu A (26 February 2021). "Vietnam enters second phase of Covid-19 vaccine trials". VnExpress.
- ↑ Onishi T (15 June 2021). "Vietnam homegrown COVID vaccine heads for full approval by year-end". Nikkei Asia.
- ↑ "A Study to Evaluate UB-612 COVID-19 Vaccine in Adolescent, Younger and Elderly Adult Volunteers". ClinicalTrials.gov. 26 February 2021. NCT04773067. Retrieved 20 March 2021.
- ↑ "A Study to Evaluate the Safety, Immunogenicity, and Efficacy of UB-612 COVID-19 Vaccine". ClinicalTrials.gov. 24 December 2020. NCT04683224. Retrieved 20 March 2021.
- ↑ Liao, George (27 June 2021). "Taiwan's second domestic COVID vaccine's midterm performance in phase II trials inferior to local competitor: experts". Taiwan News. Retrieved 8 July 2021.
- ↑ "A Study to Evaluate the Safety, Tolerability, and Immunogenicity of UB-612 COVID-19 Vaccine". ClinicalTrials.gov. 11 September 2020. NCT04545749. Retrieved 20 March 2021.
- ↑ Strong, Matthew (30 June 2021). "Taiwan's United Biomedical applies for COVID vaccine EUA". Taiwan News.
- ↑ "SCB-2019 as COVID-19 Vaccine". ClinicalTrials.gov. 28 May 2020. NCT04405908. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ "Clover Biopharmaceuticals starts Phase I Covid-19 vaccine trial". Clinical Trials Arena. 20 June 2020. Archived from the original on 11 October 2020. Retrieved 25 June 2020.
- ↑ "About Us". Clover Biopharmaceuticals. Archived from the original on 11 October 2020. Retrieved 1 August 2020.
- ↑ "A Controlled Phase 2/3 Study of Adjuvanted Recombinant SARS-CoV-2 Trimeric S-protein Vaccine (SCB-2019) for the Prevention of COVID-19 (SCB-2019)". ClinicalTrials.gov. 17 December 2020. NCT04672395. Retrieved 10 March 2021.
- ↑ "Clover Biopharmaceuticals and Dynavax Announce First Participants Dosed in SPECTRA, a Global Phase 2/3 Clinical Trial for Adjuvanted S-Trimer COVID-19 Vaccine Candidate". Dynavax. 24 March 2021. Retrieved 7 June 2021.
- ↑ "A Study of Safety and Immunogenicity of Adjuvanted SARS-CoV-2 (SCB-2019) Vaccine in Adults With Chronic Immune-Mediated Diseases". ClinicalTrials.gov. 19 August 2021. NCT05012787. Retrieved 19 August 2021.
- ↑ "Immunogenicity and Safety Study of Adjuvanted SARS-CoV-2 (SCB-2019) Vaccine in Adults in China". ClinicalTrials.gov. 8 July 2021. NCT04954131. Retrieved 8 July 2021.
- ↑ "A Phase 2/3 Study of S-268019". jrct.niph.go.jp. Japan Registry of Clinical Trials. Retrieved 20 October 2021.
- ↑ "A Phase 3 Study of S-268019 for the Prevention of COVID-19". ClinicalTrials.gov. 28 January 2022. NCT05212948. Retrieved 28 January 2022.
- ↑ "Safety and Immunogenicity of an Intranasal RSV Vaccine Expressing SARS-CoV-2 Spike Protein (COVID-19 Vaccine) in Adults". jrct.niph.go.jp. Japan Registry of Clinical Trials. Retrieved 21 March 2021.
- ↑ "A Global Phase III Clinical Trial of Recombinant COVID- 19 Vaccine (Sf9 Cells)". ClinicalTrials.gov. 27 May 2021. NCT04904471. Retrieved 28 May 2021.
- ↑ "A global phase III clinical trial of recombinant COVID-19 vaccine (Sf9 cells) in adults aged 18 years and older". chictr.org.cn. 12 May 2021. ChiCTR2100046272. Retrieved 12 May 2021.
- ↑ "A global multicenter, randomized, double-blind, placebo-controlled, phase III clinical trial to evaluate the efficacy, safety, and immunogenicity of recombinant COVID-19 vaccine (Sf9 cells), for the prevention of COVID-19 in adults aged 18 years and older". registry.healthresearch.ph. PHRR210712-003704.
- ↑ "Phase I Trial of a Recombinant SARS-CoV-2 Vaccine (Sf9 Cell)". ClinicalTrials.gov. 28 August 2020. NCT04530656. Retrieved 20 March 2021.
- ↑ "A Phase II Clinical Trial of Recombinant Corona Virus Disease-19 (COVID-19) Vaccine (Sf9 Cells)". ClinicalTrials.gov. 23 November 2020. NCT04640402. Retrieved 20 March 2021.
- ↑ "Phase IIb Clinical Trial of Recombinant Novel Coronavirus Pneumonia (COVID-19) Vaccine (Sf9 Cells)". ClinicalTrials.gov. 22 January 2021. NCT04718467. Retrieved 20 March 2021.
- ↑ "A Phase III Clinical Trial of Influenza Virus Vector COVID- 19 Vaccine for Intranasal Spray (DelNS1-2019-nCoV-RBD-OPT1)". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 23 September 2021.
- ↑ "A Phase I Clinical Trial of Influenza virus Vector COVID-19 Vaccine for intranasal Spray (DelNS1-2019-nCoV-RBD-OPT1)". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 24 March 2021.
- ↑ "A Phase II Clinical Trial of Influenza virus Vector COVID-19 Vaccine for intranasal Spray (DelNS1-2019-nCoV-RBD-OPT1)". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 24 March 2021.
- ↑ "Entenda ponto a ponto a Versamune, vacina contra a Covid-19 financiada pelo governo federal". G1 Globo. 26 March 2021. Retrieved 19 September 2021.
- ↑ "Vacina Versamune: o que se sabe sobre imunizante anunciado pelo governo federal". BBC News Brazil. 26 March 2021. Retrieved 19 September 2021.
- ↑ "Vacina Versamune: o que se sabe sobre imunizante anunciado pelo governo federal". BBC News Brazil. 26 March 2021. Retrieved 19 September 2021.
- ↑ "Randomized Controlled-trial to Evaluate Safety and Immunogenicity of a Novel Vaccine for Prevention of Covid-19 in Adults Previously Immunized". clinicaltrials.gov. 23 August 2021. NCT05016934. Retrieved 23 August 2021.
- ↑ "A Phase I clinical trial to evaluate the safety, tolerance and preliminary immunogenicity of different doses of a SARS-CoV-2 mRNA vaccine in population aged 18–59 years and 60 years and above". Chinese Clinical Trial Register. 24 June 2020. ChiCTR2000034112. Archived from the original on 11 October 2020. Retrieved 6 July 2020.
- ↑ "Company introduction". Walvax Biotechnology. Archived from the original on 11 October 2020. Retrieved 1 August 2020.
- ↑ "A Phase III Clinical Study to Evaluate the Protective Efficacy, Safety, and Immunogenicity of a SARS-CoV-2 Messenger Ribonucleic Acid (mRNA) Vaccine Candidate in Population Aged 18 Years and Above". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 17 April 2020.
- ↑ "A Global, Multi-center, Randomized, Double-Blind, Placebo-controlled, Phase III Clinical Study to Evaluate the Protective Efficacy, Safety and Immunogenicity of SARS-CoV-2 mRNA Vaccine in Population Aged 18 Years and Older". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 21 July 2021.
- ↑ "A Phase I/II Clinical Trial to Evaluate the Immunogenicity and Safety of the SARS-CoV-2 mRNA Vaccine in Healthy Population Aged 60 Years and Older". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 2 August 2021.
- ↑ "A Phase II clinical trial to evaluate the immunogenicity and safety of different doses of a novel coronavirus pneumonia (COVID-19) mRNA vaccine in population aged 18-59 years". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 20 March 2021.
- ↑ "Recombinant SARS-CoV-2 Fusion Protein Vaccine (V-01) Phase III (COVID-19)". ClinicalTrials.gov. 27 October 2021. NCT05096845. Retrieved 27 October 2021.
- ↑ "评价重组新型冠状病毒融合蛋白疫苗在健康人群免疫原性和安全性随机、双盲、安慰剂对照的II期临床试验". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 21 April 2021.
- ↑ "评价重组新型冠状病毒融合蛋白疫苗在健康人群安全性和免疫原性随机、双盲、安慰剂对照的I期临床试验". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 21 April 2021.
- ↑ "Arcturus Therapeutics Collaborates with Vingroup to Establish Manufacturing Facility in Vietnam for Arcturus' Investigational mRNA Vaccines for COVID-19". Business Wire. 2 August 2021.
- ↑ "Arcturus Allows Vietnam's Vingroup to Make Covid Vaccines". Bloomberg. 2 August 2021.
- ↑ "Vingroup collaborates with Arcturus Therapeutics to establish a manufacturing facility in Vietnam for Arcturus' mRNA Covid-19 vaccine". Yahoo! Finance. 2 August 2021.
- ↑ "Arcturus to start clinical trial of COVID-19 vaccine in Vietnam". Reuters. 2 August 2021.
- ↑ "Arcturus Therapeutics lines up Phase 1/2/3 trial for next-generation mRNA COVID-19 vaccine". Biopharma Reporter. 2 August 2021.
- ↑ "The ARCT-154 Self-Amplifying RNA Vaccine Efficacy Study (ARCT-154-01) (ARCT-154-01)". United States National Library of Medicine. 19 August 2021. NCT05012943. Retrieved 19 August 2021.
- ↑ "Efficacy, Safety, and Immunogenicity Study of the Recombinant Two-component COVID-19 Vaccine (CHO Cell) (ReCOV)". ClinicalTrials.gov. 20 October 2021. NCT05084989. Retrieved 20 October 2021.
- ↑ "Safety, Reactogenicity and Immunogenicity Study of ReCOV". ClinicalTrials.gov. 26 March 2021. NCT04818801. Retrieved 2 April 2021.
- ↑ "A Phase I/II Randomized, Multi-Center, Placebo-Controlled, Dose-Escalation Study to Evaluate the Safety, Immunogenicity and Potential Efficacy of an rVSV-SARS-CoV-2-S Vaccine (IIBR-100) in Adults". ClinicalTrials.gov. 1 November 2020. NCT04608305.
- ↑ "Phase 2b Dose-confirmatory Trial to Evaluate the Safety, Immunogenicity and Potential Efficacy of an VSV-ΔG SARS-CoV-2 Vaccine (BRILIFE001)". ClinicalTrials.gov. 29 July 2021. NCT04990466. Retrieved 13 September 2021.
- ↑ "As Israel goes vaccine-wild, will the homegrown version lose its shot?". The Times of Israel. 29 December 2020. Retrieved 1 January 2021.
- ↑ "Efficacy, safety and immunogenicity of a recombinant protein subunit vaccine (CHO cells) against COVID-19 in adults: an international multicenter, randomized, double-blind, placebo-controlled phase III study". chictr.org.cn. Chinese Clinical Trial Registry. 5 September 2021. ChiCTR2100050849. Retrieved 5 September 2021.
- ↑ "Phase I Trial of a Recombinant COVID-19 Vaccine (CHO Cell)". ClinicalTrials.gov. United States National Library of Medicine. 19 November 2020. NCT04636333. Retrieved 13 April 2021.
- ↑ "Immunogenicity and Safety of Recombinant COVID-19 Vaccine (CHO Cells)". ClinicalTrials.gov. United States National Library of Medicine. 24 March 2021. NCT04813562. Retrieved 13 April 2021.
- ↑ "Safety and Immunogenicity Study of GX-19, a COVID-19 Preventive DNA Vaccine in Healthy Adults". ClinicalTrials.gov. 24 June 2020. NCT04445389. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ "Safety and Immunogenicity Study of GX-19N, a COVID-19 Preventive DNA Vaccine in Healthy Adults". ClinicalTrials.gov. 20 January 2021. NCT04715997. Retrieved 16 March 2021.
- ↑ "S. Korea's Genexine begins human trial of coronavirus vaccine". Reuters. 19 June 2020. Archived from the original on 11 October 2020. Retrieved 25 June 2020.
- ↑ "Genexine consortium's Covid-19 vaccine acquires approval for clinical trails in Korea". 11 June 2020. Retrieved 1 August 2020.
- ↑ "Safety and Immunogenicity of GX-19N, a COVID-19 Preventive DNA Vaccine in Elderly Individuals". ClinicalTrials.gov. 7 June 2021. NCT04915989. Retrieved 8 June 2021.
- ↑ "Evaluation of Efficacy, Safety and Immunogenicity of GX-19N in Healthy Individuals Who Have Received COVID-19 Vaccines". ClinicalTrials.gov. 5 October 2021. NCT05067946. Retrieved 5 October 2021.
- ↑ "GRAd-COV2 Vaccine Against COVID-19". ClinicalTrials.gov. 27 August 2020. NCT04528641.
- ↑ "ReiThera Announces its GRAd-COV2 COVID-19 Vaccine Candidate is Well Tolerated and Induces Clear Immune Responses in Healthy Subjects Aged 18–55 Years". ReiThera Srl. Yahoo! Finance. 24 November 2020. Retrieved 12 January 2021.
- ↑ "Study of GRAd-COV2 for the Prevention of COVID-19 in Adults (COVITAR)". ClinicalTrials.gov. 10 March 2021. NCT04791423. Retrieved 20 March 2021.
- ↑ "ReiThera's COVID-19 vaccine candidate enters Phase 2/3 clinical study". ReiThera. 18 March 2021. Retrieved 20 March 2021.
- ↑ "New ReiThera vaccine safe, response peak at 4 wks". ANSA. 5 January 2021.
- ↑ "Safety, Tolerability and Immunogenicity of INO-4800 for COVID-19 in Healthy Volunteers". ClinicalTrials.gov. 7 April 2020. NCT04336410. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ "IVI, INOVIO, and KNIH to partner with CEPI in a Phase I/II clinical trial of INOVIO's COVID-19 DNA vaccine in South Korea". International Vaccine Institute. 16 April 2020. Retrieved 23 April 2020.
- ↑ "Safety, Immunogenicity, and Efficacy of INO-4800 for COVID-19 in Healthy Seronegative Adults at High Risk of SARS-CoV-2 Exposure". ClinicalTrials.gov. 24 November 2020. NCT04642638. Retrieved 12 March 2021.
- ↑ "Safety, Tolerability and Immunogenicity of INO-4800 Followed by Electroporation in Healthy Volunteers for COVID19". United States National Library of Medincine. Retrieved 12 March 2021.
- ↑ "A Phase II, Randomized, Double-Blinded, Placebo-Controlled, Dose-Finding Clinical Trial to Evaluate the Safety and Immunogenicity of Different Doses of COVID-19 DNA Vaccine INO-4800 Administered Intradermally Followed by Electroporation in Healthy Adult and Elderly Volunteers". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 27 March 2021.
- ↑ "Daiichi Sankyo Initiates Phase 1/2 Clinical Trial for mRNA COVID-19 vaccine in Japan" (PDF) (Press release). Daiichi Sankyo. Retrieved 17 April 2021.
- ↑ "Daiichi takes mRNA COVID-19 vaccine into clinic as Japanese R&D belatedly fires up". Fierce Biotech. 22 March 2021. Retrieved 12 April 2021.
- ↑ "既承認SARS-CoV-2 ワクチンの初回接種完了者を対象としたDS-5670a による追加免疫効果を検討する第I/II/III 相、無作為化、実薬対照、評価者盲検試験". jrct.niph.go.jp. 28 December 2021. jRCT2071210106. Retrieved 28 December 2021.
- ↑ "Study of DS-5670a (COVID-19 Vaccine) in Japanese Healthy Adults and Elderly Subjects". ClinicalTrials.gov. 29 March 2021. NCT04821674. Retrieved 12 April 2021.
- ↑ "SK Bioscience Submitted Phase 3 IND for COVID-19 Vaccine". SK Bioscience.
- ↑ "A Phase III Study to Assess the Immunogenicity and Safety of SK SARS-CoV-2 Recombinant Nanoparticle Vaccine Adjuvanted With AS03 (GBP510) in Adults Aged 18 Years and Older". ClinicalTrials.gov. 17 August 2021. NCT05007951. Retrieved 17 August 2021.
- ↑ "Safety and Immunogenicity Study of SARS-CoV-2 Nanoparticle Vaccine (GBP510) Adjuvanted With or Without AS03 (COVID-19)". ClinicalTrials.gov. 11 February 2021. NCT04750343. Retrieved 22 April 2021.
- ↑ "Safety and Immunogenicity Study of SARS-CoV-2 Nanoparticle Vaccine (GBP510) Adjuvanted With Aluminum Hydroxide (COVID-19)". ClinicalTrials.gov. 8 February 2021. NCT04742738. Retrieved 22 April 2021.
- ↑ "Indigenous mRNA vaccine candidate supported by DBT gets Drug Controller nod to initiate Human clinical trials" (Press release). Press Information Bureau. Retrieved 13 January 2021.
- ↑ "mRNA Vaccines – HGC019". Gennova Biopharmaceuticals Limited. Retrieved 13 January 2021.
- ↑ "Safety and immunogenicity study of an mRNA based vaccine (HGCO19) for COVID19 in healthy adult participants". ctri.nic.in. Clinical Trials Registry India. Retrieved 9 September 2021.
- ↑ Raghavan P (15 December 2020). "Pune-based Gennova to begin human trials of its Covid vaccine 'soon'". The Indian Express.
- ↑ "Safety and immunogenicity study of mRNA based vaccine (HGCO19) against COVID-19 in healthy adult participants". ctri.nic.in. Clinical Trials Registry India. Retrieved 5 June 2021.
- ↑ "Safety and immunogenicity study of mRNA based vaccine (HGCO19) against COVID-19 in healthy adult participants". Cochrane COVID-19 Study Register. 4 August 2021. Archived from the original on 11 September 2021.
- ↑ "18歳以上の健康な日本人を対象に、COVID-19に対するワクチン(KD-414)を2回接種した際の免疫原性及び安全性を確認する多施設共同非盲検非対照試験。". jrct.niph.go.jp. Japan Registry of Clinical Trials. Retrieved 22 October 2021.
- ↑ "Japan's KM Biologics begins clinical trial of COVID-19 vaccine candidate". Reuters. 22 March 2021.
- ↑ "20歳以上65歳未満の健康成人、及び65歳以上の健康な高齢者を対象に、COVID-19に対するワクチン(KD-414)の安全性及び免疫原性を検討するための、プラセボを対照とする多施設共同二重盲検ランダム化並行群間比較試験". jrct.niph.go.jp. Japan Registry of Clinical Trials. Retrieved 7 May 2021.
- ↑ "Phase Ⅱ and Ⅲ Trial of a SARS-CoV-2 Vaccine LYB001". ClinicalTrials.gov. 30 November 2021. NCT05137444. Retrieved 30 November 2021.
- ↑ "A Phase Ⅰ Trial to Evaluate the Safety and Immunogenicity of SARS-CoV-2 Vaccine LYB001". ClinicalTrials.gov. 18 November 2021. NCT05125926. Retrieved 18 November 2021.
- ↑ "Immunogenicity and safety of a SARS-CoV-2 Vaccine LYB001 against COVID-19 in healthy adults: a randomized, double blinded, placebo-controlled phase II trial and a single-armed, open-label expanded safety phase III trial". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 15 October 2021.
- ↑ "Safety, Reactogenicity, and Immunogenicity of a Recombinant SARS-CoV-2 Vaccine LYB001 in healthy adults: a randomized, double blinded, placebo-controlled phase I trial". chictr.org.cn. Chinese Clinical Trial Registry. Retrieved 15 October 2021.
- ↑ "A study to assess the safety and immunogenicity of Anti-COVID-19 AKS-452 vaccine for SARS-Сov-2 infection in Indian healthy subjects". ctri.nic.in. 11 October 2021. CTRI/2021/10/037269. Retrieved 11 October 2021.
- ↑ "Anti-COVID19 AKS-452 – ACT Study (ACT)". ClinicalTrials.gov. 23 December 2020. NCT04681092. Retrieved 21 March 2021.
- ↑ "Study of COVID-19 DNA Vaccine (AG0301-COVID19)". ClinicalTrials.gov. 9 July 2020. NCT04463472. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ "Study of COVID-19 DNA Vaccine (AG0302-COVID19)". ClinicalTrials.gov. 26 August 2020. NCT04527081. Retrieved 11 March 2021.
- ↑ "About AnGes – Introduction". AnGes, Inc. Archived from the original on 11 October 2020. Retrieved 1 August 2020.
- ↑ "Phase II / III Study of COVID-19 DNA Vaccine (AG0302-COVID19)". ClinicalTrials.gov. 7 December 2020. NCT04655625. Retrieved 11 March 2021.
- ↑ "Phase II Clinical Trial of Recombinant SARS-CoV-2 Spike Protein Vaccine (CHO Cell)". ClinicalTrials.gov. 4 August 2021. NCT04990544. Retrieved 4 August 2021.
- ↑ "Phase I Clinical Trial of Recombinant SARS-CoV-2 Spike Protein Vaccine (CHO Cell)". ClinicalTrials.gov. 4 July 2021. NCT04982068. Retrieved 29 July 2021.
- ↑ "A Ph 2 Trial With an Oral Tableted COVID-19 Vaccine". ClinicalTrials.gov. 5 October 2021. NCT05067933. Retrieved 5 October 2021.
- ↑ "Safety and Immunogenicity Trial of an Oral SARS-CoV-2 Vaccine (VXA-CoV2-1) for Prevention of COVID-19 in Healthy Adults". ClinicalTrials.gov. 24 September 2020. NCT04563702. Retrieved 22 March 2021.
- ↑ "Ph 1b: Safety & Immunogenicity of Ad5 Based Oral Norovirus Vaccine (VXA-NVV-104)". ClinicalTrials.gov. 22 April 2021. NCT04854746. Retrieved 25 May 2021.
- ↑ 137.0 137.1 "Made-in-Canada coronavirus vaccine starts human clinical trials". Canadian Broadcasting Corporation. 26 January 2021.
- ↑ "PTX-COVID19-B, an mRNA Humoral Vaccine, Intended for Prevention of COVID-19 in a General Population. This Study is Designed to Demonstrate the Safety, Tolerability, and Immunogenicity of PTX-COVID19-B in Comparison to the Pfizer-BioNTech COVID-19 Vaccine". ClinicalTrials.gov. 4 January 2022. NCT05175742. Retrieved 6 January 2022.
- ↑ "PTX-COVID19-B, an mRNA Humoral Vaccine, is Intended for Prevention of COVID-19 in a General Population. This Study is Designed to Evaluate Safety, Tolerability, and Immunogenicity of PTX-COVID19-B Vaccine in Healthy Seronegative Adults Aged 18-64". ClinicalTrials.gov. 21 February 2021. NCT04765436. Retrieved 22 April 2021.
- ↑ "Randomized, double-blind, placebo-controlled phase II clinical trial of immunogenicity, immunopersistence, and safety of graded Novel Coronavirus inactivated vaccine (Vero cells) in healthy persons aged 18 years and older". chictr.org.cn. 29 September 2021. ChiCTR2100050024. Retrieved 3 October 2021.
- ↑ "A randomized, double-blind, placebo-controlled phase I clinical trial to evaluate the safety and immunogenicity of the Novel Coronavirus inactivated vaccine (Vero cells) in healthy individuals 18 years of age and older". chictr.org.cn. 16 August 2021. ChiCTR2100050024. Retrieved 16 August 2021.
- ↑ "Another Chinese adenovirus vector COVID-19 vaccine ready for human trials". Xinhua. 28 December 2020. Retrieved 27 July 2021.
- ↑ "A Phase II Clinical Trial of the Recombinant SARS-CoV-2 Vaccine (Chimpanzee Adenoviral Vector)". chictr.org.cn. 2 August 2021. ChiCTR2100049530. Retrieved 2 August 2021.
- ↑ "Phase I Clinical Trial of the Candidate Recombinant SARS-CoV-2 Vaccine (Chimpanzee Adenoviral Vector)". chictr.org.cn. 23 May 2021. ChiCTR2100046612. Retrieved 23 May 2021.
- ↑ "INNA-051 intranasal safety and tolerability study". clinicaltrials.gov. 12 November 2021. NCT05118763. Retrieved 12 November 2021.
- ↑ "INNA-051 intranasal safety and tolerability study". anzctr.org.au. 21 April 2021. ACTRN12621000607875p. Retrieved 20 May 2021.
- ↑ "A Study to Evaluate the Immunogenicity and Safety of mRNA-1283 COVID-19 Vaccine Boosters". ClinicalTrials.gov. 30 November 2021. NCT05137236. Retrieved 30 November 2021.
- ↑ "A Study to Evaluate Safety, Reactogenicity, and Immunogenicity of mRNA-1283 and mRNA-1273 Vaccines in Healthy Adults Between 18 Years and 55 Years of Age to Prevent COVID-19". ClinicalTrials.gov. 24 March 2021. NCT04813796. Retrieved 17 August 2021.
- ↑ "Study of a Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) Virus-like Particle (VLP) Vaccine (COVID-19)". ClinicalTrials.gov. 15 July 2021. NCT04962893. Retrieved 15 July 2021.
- ↑ "Study of a Severe Acute Respiratory Syndrome CoV-2 (SARS-CoV-2) Virus-like Particle (VLP) Vaccine in Healthy Adults (COVID-19)". ClinicalTrials.gov. 26 March 2021. NCT04818281. Retrieved 3 April 2021.
- ↑ "SARS-CoV-2 Vaccine (COH04S1) Versus Emergency Use Authorization SARS-COV-2 Vaccine for the Treatment of COVID-19 in Patients With Blood Cancer". ClinicalTrials.gov. 26 July 2021. NCT04977024. Retrieved 26 July 2021.
- ↑ "A Synthetic MVA-based SARS-CoV-2 Vaccine, COH04S1, for the Prevention of COVID-19". ClinicalTrials.gov. 20 November 2020. NCT04639466. Retrieved 21 March 2021.
- ↑ "Bavarian Nordic reports encouraging preclinical data for COVID-19 vaccine candidate ahead of first-in-human trial". Bavarian Nordic. 8 March 2021. Retrieved 13 April 2021.
- ↑ "Bavarian Nordic Initiates Phase 2 Clinical Trial of COVID-19 Booster Vaccine". Bavarian Nordic. 23 August 2021. Retrieved 24 August 2021.
- ↑ "ABNCoV2 Vaccine in SARS-CoV-2 Seronegative and Seropositive Adult Subjects". ClinicalTrials.gov. 14 October 2021. NCT05077267. Retrieved 14 October 2021.
- ↑ "Safety and Tolerability of ABNCoV2 (COUGH-1)". ClinicalTrials.gov. 9 April 2021. NCT04839146. Retrieved 13 April 2021.
- ↑ "Clover Announces Positive Preclinical Data for Second-Generation Protein-Based COVID-19 Vaccine Candidate Demonstrating Broad Neutralization Against Variants of Concern". Clover Biopharmaceutical. 18 May 2021. Retrieved 9 July 2021.
- ↑ "Immunogenicity and Safety of Adjuvanted SCB-2020S Vaccines in Adults". United States National Library of Medicine. 6 July 2021. NCT04950751. Retrieved 6 July 2021.
- ↑ "The Safety and Efficacy of SCTV01C in Population Aged ≥18 Years Previously Vaccinated With Inactivated COVID-19 Vaccine.Healthy Population Aged ≥18 Years Previously Vaccinated With Adenovirus Vectored or mRNA COVID-19 Vaccine". United States National Library of Medicine. 14 September 2021. NCT05043311. Retrieved 14 September 2021.
- ↑ "The Safety and Efficacy of SCTV01C in Population Aged ≥18 Years Previously Vaccinated With Inactivated COVID-19 Vaccine.Healthy Population Aged ≥18 Years Previously Vaccinated With Inactivated COVID-19 Vaccine". United States National Library of Medicine. 14 September 2021. NCT05043285. Retrieved 14 September 2021.
- ↑ "Safety, Tolerability and Immunogenicity of SCTV01C in Healthy Population Aged ≥18 Years Previously Unvaccinated". United States National Library of Medicine. 8 December 2021. NCT05148091. Retrieved 8 December 2021.
- ↑ "A Phase 1/2 Safety and Immunogenicity Trial of COVID-19 Vaccine COVIVAC". ClinicalTrials.gov. 5 April 2021. NCT04830800. Retrieved 13 April 2021.
- ↑ "A Live Recombinant Newcastle Disease Virus-vectored COVID-19 Vaccine Phase 1 Study". ClinicalTrials.gov. 25 January 2022. NCT05205746. Retrieved 25 January 2022.
- ↑ "Assess the Safety and Immunogenicity of NDV-HXP-S Vaccine in Thailand". ClinicalTrials.gov. 21 February 2021. NCT04764422. Retrieved 7 April 2021.
- ↑ "A Live Recombinant Newcastle Disease Virus-vectored COVID-19 Vaccine Phase 1 Study". ClinicalTrials.gov. 6 January 2022. NCT05181709. Retrieved 6 January 2022.
- ↑ "Vaccine COVID-19 "made in Vietnam" COVIVAC thử nghiệm giai đoạn 2". VTV. 10 August 2021. Retrieved 12 August 2021.
- ↑ Zimmer C (5 April 2021). "Researchers Are Hatching a Low-Cost Coronavirus Vaccine". The New York Times. Retrieved 7 April 2021.
- ↑ "Randomized, double-blind, placebo-controlled phase I clinical trial to evaluate the safety and immunogenicity of mRNACOVID-19 vaccine in healthy susceptible populations aged 18 years and older people". Chinese Clinical Trial Registry (ChiCTR). Retrieved 15 May 2021.
- ↑ "A Phase I/II Clinical Trial in Healthy People Aged 18 Years and Above". ClinicalTrials.gov. 3 December 2021. NCT05144139. Retrieved 3 December 2021.
- ↑ "CTI and Arcturus Therapeutics Announce Initiation of Dosing of COVID-19 STARR mRNA Vaccine Candidate, LUNAR-COV19 (ARCT-021) in a Phase 1/2 study". UK BioIndustry Association. 13 August 2020. Archived from the original on 11 October 2020. Retrieved 23 August 2020.
- ↑ "Ascending Dose Study of Investigational SARS-CoV-2 Vaccine ARCT-021 in Healthy Adult Subjects". Archived from the original on 11 October 2020. Retrieved 23 August 2020.
- ↑ "A Trial Evaluating the Safety and Effects of an RNA Vaccine ARCT-021 in Healthy Adults". ClinicalTrials.gov. 16 December 2020. NCT04668339. Retrieved 10 March 2021.
- ↑ "Open Label Extension Study to Assess the Safety and Long-Term Immunogenicity of ARCT-021". ClinicalTrials.gov. 28 January 2021. NCT04728347. Retrieved 13 March 2021.
- ↑ "Phase I/II of the Safety and Immunogenicity of SARS-CoV-2 Protein Subunit Recombinant Vaccine in Healthy Populations". ClinicalTrials.gov. 5 October 2021. NCT05067894. Retrieved 5 October 2021.
- ↑ "VBI Vaccines Announces Initiation of Enrollment in Adaptive Phase 1/2 Study of Prophylactic COVID-19 Vaccine Candidate, VBI-2902". VBI Vaccines (Press release). 9 March 2021. Retrieved 22 March 2021.
- ↑ "Safety, Tolerability, and Immunogenicity of the COVID-19 Vaccine Candidates VBI-2902a and VBI-2905a". ClinicalTrials.gov. 26 February 2021. NCT04773665. Retrieved 8 October 2021.
- ↑ "Novavax Announces Positive Preclinical Data for Combination Influenza and COVID-19 Vaccine Candidate". Novavax. 10 May 2021.
- ↑ "Evaluation of the Safety and Immunogenicity of Influenza and COVID-19 Combination Vaccine". ClinicalTrials.gov. 14 July 2021. NCT04961541. Retrieved 26 July 2021.
- ↑ "Safety, Tolerance and Immunogenicity of EuCorVac-19 for the Prevention of COVID-19 in Healthy Adults". ClinicalTrials.gov. 5 March 2021. NCT04783311. Retrieved 20 March 2021.
- ↑ Limon, Raul (12 August 2021). "First Spanish Covid-19 vaccine approved for human clinical trial". El Pais. Retrieved 15 August 2021.
- ↑ "Safety and Immunogenicity Study of Recombinant Protein RBD Candidate Vaccine Against SARS-CoV-2 in Adult Healthy Volunteers (COVID-19)". clinicaltrials.gov. 16 August 2021. NCT05007509. Retrieved 16 August 2021.
- ↑ "Safety and Immunogenicity of Recombinant Protein RBD Fusion Dimer Vaccine Against the Virus That Cause COVID-19, Known as Severe Acute Respiratoy Syndrome Coronavirus 2 (SARS-CoV-2)". clinicaltrials.gov. 2 December 2021. NCT05142514. Retrieved 2 December 2021.
- ↑ "Trial registered on ANZCTR". anzctr.org.au. Australian New Zealand Clinical Trials Registry. Retrieved 24 March 2021.
- ↑ "Phase I-II Trial of Dendritic Cell Vaccine to Prevent COVID-19 in Adults". ClinicalTrials.gov. 13 May 2020. NCT04386252. Retrieved 23 March 2021.
- ↑ "Dendritic Cell Vaccine to Prevent COVID-19". ClinicalTrials.gov. 28 December 2020. NCT04685603. Retrieved 23 March 2021.
- ↑ "Safety and Immunogenicity of COVID-eVax, a Candidate Plasmid DNA Vaccine for COVID-19, in Healthy Adult Volunteers". ClinicalTrials.gov. 9 March 2021. NCT04788459. Retrieved 21 March 2021.
- ↑ 187.0 187.1 "Safety and Immunogenicity of an Intranasal SARS-CoV-2 Vaccine (BBV154) for COVID-19". ClinicalTrials.gov. 12 February 2021. NCT04751682. Archived from the original on 24 February 2021.
- ↑ "Intranasal Vaccine For Covid-19". Bharat Biotech. Retrieved 5 March 2021.
- ↑ Gaurav, Kunal (13 August 2021). "First nasal vaccine developed by Bharat Biotech gets nod for Phase 2/3 trial". Hindustan Times.
- ↑ "Intranasal COVID-19 vaccine Phase 2 study in Healthy volunteers". ctri.nic.in. Clinical Trials Registry India. Retrieved 3 September 2021.
- ↑ "Vaccibody reports promising preclinical data with a second-generation COVID-19 vaccine and announces its infectious disease strategy" (PDF). vaccibody.com. 10 December 2020.
- ↑ "Vaccibody reports promising preclinical data with a second-generation COVID-19 vaccine and announces its infectious disease strategy" (PDF). vaccibody.com. 10 December 2020.
- ↑ "Vaccibody to initiate a phase 1/2 trial to evaluate two second-generation SARS CoV-2 virus DNA vaccine candidates to address emerging variants of concern" (PDF). vaccibody.com. 29 June 2021.
- ↑ "A Phase 1/2, Dose Escalation Study to Determine Safety and Immunogenicity of Two COVID 19 Vaccines VB10.2129 (RBD Candidate) and VB10.2210 (T Cell Candidate) in Healthy Adult Volunteers". ClinicalTrials.gov. 6 October 2021. NCT05069623. Retrieved 6 October 2021.
- ↑ "ChulaCov19 mRNA Vaccine in Healthy Adults". ClinicalTrials.gov. 28 September 2020. NCT04566276. Retrieved 21 March 2021.
- ↑ 196.0 196.1 "Safety and Immunity of Covid-19 aAPC Vaccine". ClinicalTrials.gov. 9 March 2020. NCT04299724. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ 197.0 197.1 "About Us". Shenzhen Genoimmune Medical Institute. Archived from the original on 11 October 2020. Retrieved 1 August 2020.
- ↑ 198.0 198.1 "Immunity and Safety of Covid-19 Synthetic Minigene Vaccine". ClinicalTrials.gov. 19 February 2020. NCT04276896. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ "COVID-19 Vaccination Using a 2nd Generation (E1/E2B/E3-Deleted) Adenoviral Platform in Healthy South African Adults". ClinicalTrials.gov. 14 January 2021. NCT04710303. Retrieved 23 March 2021.
- ↑ "COVID-19 Oral and Subcutaneous Vaccination Using a 2nd Generation (E1/E2B/E3-Deleted) Adenovirus Platform in Healthy Volunteers in USA". ClinicalTrials.gov. 1 February 2021. NCT04732468. Retrieved 23 March 2021.
- ↑ "COVID-19 Vaccination Using a 2nd Generation (E1/E2B/E3-Deleted) Adenoviral-COVID-19 in Normal Healthy Volunteers". ClinicalTrials.gov. 19 October 2020. NCT04591717. Retrieved 23 March 2021.
- ↑ "COVID-19 Subcutaneously and Orally Administered Supplemental Vaccine Boost to Enhance T Cell Protection in Those Who Have Already Received EUA S-Based Vaccines". ClinicalTrials.gov. 14 April 2021. NCT04845191. Retrieved 22 April 2021.
- ↑ "COVID-19 Supplemental Vaccine Boost to Enhance T Cell Protection in Those Who Have Already Received EUA S-Based Vaccines". ClinicalTrials.gov. 13 April 2021. NCT04843722. Retrieved 22 April 2021.
- ↑ 204.0 204.1 "VIDO COVID-19 vaccine moves to Phase 1 clinical testing". globalnews.ca. 10 February 2021.
- ↑ "A Clinical Trial of COVAC-2 in Healthy Adults". ClinicalTrials.gov. 8 January 2021. NCT04702178. Retrieved 20 April 2021.
- ↑ "A Clinical Trial of COVAC-1 in Generally Healthy Adults". ClinicalTrials.gov. 14 December 2021. NCT05155982. Retrieved 14 December 2021.
- ↑ "Serum Institute starts manufacturing Codagenix's nasal COVID-19 vaccine". mint. 22 September 2020.
- ↑ "Safety and Immunogenicity of COVI-VAC, a Live Attenuated Vaccine Against COVID-19". ClinicalTrials.gov. 6 November 2020. NCT04619628.
- ↑ "A Study of the Safety of and Immune Response to Varying Doses of a Vaccine Against COVID-19 in Healthy Adults". ClinicalTrials.gov. 17 February 2021. NCT04758962.
- ↑ "COVALIA study update: first healthy volunteers dosed in needle-free SARS-CoV2 DNA vaccine phase 1 trial". Bionet Asia. 30 June 2021. Retrieved 19 July 2021.
- ↑ "The Safety and Immunogenicity of a DNA-based Vaccine (COVIGEN) in Healthy Volunteers (COVALIA)". ClinicalTrials.gov. 8 February 2021. NCT04742842.
- ↑ "Meissa Announces IND Clearance for Phase 1 Study of Intranasal Live Attenuated Vaccine Candidate for COVID-19". Business Wire. 16 March 2021. Retrieved 20 March 2021.
- ↑ "Safety and Immunogenicity of an Intranasal RSV Vaccine Expressing SARS-CoV-2 Spike Protein (COVID-19 Vaccine) in Adults". ClinicalTrials.gov. 15 March 2021. NCT04798001. Retrieved 20 March 2021.
- ↑ "KBP-201 COVID-19 Vaccine Trial in Healthy Volunteers". ClinicalTrials.gov. 16 July 2020. NCT04473690. Retrieved 21 March 2021.
- ↑ "Safety and Immunogenicity Study of AdCLD-CoV19: A COVID-19 Preventive Vaccine in Healthy Volunteers". ClinicalTrials.gov. 14 December 2020. NCT04666012. Retrieved 23 March 2021.
- ↑ "A Study to Evaluate the Safety and Immunogenicity of COVID-19 (AdimrSC-2f) Vaccine". ClinicalTrials.gov. 21 August 2020. NCT04522089. Retrieved 21 March 2021.
- ↑ "Dose-finding Study for AdimrSC-2f Vaccine". ClinicalTrials.gov. 3 November 2021. NCT05104489. Retrieved 3 November 2021.
- ↑ "GLS-5310 Vaccine for the Prevention of SARS-CoV-2 (COVID-19)". ClinicalTrials.gov. 17 December 2020. NCT04673149. Retrieved 21 March 2021.
- ↑ "A Clinical Trial of a Plasmid DNA Vaccine for COVID-19 [Covigenix VAX-001] in Adults". ClinicalTrials.gov. 19 October 2020. NCT04591184. Retrieved 21 March 2021.
- ↑ "Safety and Immunogenicity of a SARS-CoV-2 Vaccine (NBP2001) in Healthy Adults (COVID-19)". ClinicalTrials.gov. 18 February 2021. NCT04760743. Retrieved 21 March 2021.
- ↑ "Safety and Immunogenicity Trial of Multi-peptide Vaccination to Prevent COVID-19 Infection in Adults (pVAC)". ClinicalTrials.gov. 14 September 2020. NCT04546841. Retrieved 21 March 2021.
- ↑ "B-pVAC-SARS-CoV-2: Study to Prevent COVID-19 Infection in Adults With Bcell/ Antibody Deficiency (B-pVAC)". ClinicalTrials.gov. 8 July 2020. NCT04954469. Retrieved 8 July 2021.
- ↑ "Evaluating the Safety, Tolerability and Immunogenicity of bacTRL-Spike Vaccine for Prevention of COVID-19". ClinicalTrials.gov. 6 April 2020. NCT04334980. Retrieved 21 March 2021.
- ↑ "Chimpanzee Adenovirus and Self-Amplifying mRNA Prime-Boost Prophylactic Vaccines Against SARS-CoV-2 in Healthy Adults". ClinicalTrials.gov. 1 March 2021. NCT04776317. Retrieved 22 March 2021.
- ↑ "SARS-COV-2-Spike-Ferritin-Nanoparticle (SpFN) Vaccine With ALFQ Adjuvant for Prevention of COVID-19 in Healthy Adults". ClinicalTrials.gov. 5 March 2021. NCT04784767. Retrieved 24 March 2021.
- ↑ "Safety, Tolerability and Immunogenicity of the Candidate Vaccine MVA-SARS-2-S Against COVID-19". ClinicalTrials.gov. 29 September 2020. NCT04569383. Retrieved 24 March 2021.
- ↑ "Safety, Tolerability and Immunogenicity of the Candidate Vaccine MVA-SARS-2-ST Against COVID-19 (MVA-SARS-2-ST)". ClinicalTrials.gov. 20 May 2021. NCT04895449. Retrieved 21 May 2021.
- ↑ "Safety and Immunogenicity of the Inactivated Koçak-19 Inaktif Adjuvanlı COVID-19 Vaccine Compared to Placebo". ClinicalTrials.gov. 8 April 2021. NCT04838080. Retrieved 3 April 2021.
- ↑ "First-In-Human Study Of Orally Administered CoV2-OGEN1 In Healthy Subjects". ClinicalTrials.gov. 19 May 2021. NCT04893512. Retrieved 26 May 2021.
- ↑ "OSE Immunotherapeutics Receives Authorization for Phase 1 Clinical Trial of its Multi-Target Multi-Variant COVID-19 Vaccine". BioSpace. 1 April 2021. Retrieved 13 April 2021.
- ↑ "To Evaluate the Safety, and Immunogenicity of Vaccine Candidate Against COVID-19, in Healthy Adults (COVEPIT 3)". ClinicalTrials.gov. 13 May 2021. NCT04885361. Retrieved 13 May 2021.
- ↑ "HDT Bio Receives Notice to Proceed from FDA for US Phase 1 Clinical Trial of RNA COVID-19 Vaccine". HDT Bio. 1 July 2021. Retrieved 24 December 2021.
- ↑ "HDT Bio Partner Quratis Doses First Healthy Volunteers in Phase 1 Trial of HDT Bio's RNA COVID-19 Vaccine in South Korea". HDT Bio. 13 December 2021. Retrieved 24 December 2021.
- ↑ "Phase 1 Study to Assess Safety, Reactogenicity and Immunogenicity of the HDT-301 Vaccine Against COVID-19". ClinicalTrials.gov. 14 April 2021. NCT04844268. Retrieved 4 August 2021.
- ↑ "Safety And Immunogenicity Of HDT-301 Targeting A SARS-CoV-2 Variant Spike Protein". ClinicalTrials.gov. 24 November 2021. NCT05132907. Retrieved 24 November 2021.
- ↑ "A Phase 1, First-In-Human Study of the Investigational COVID-19 Vaccine SC-Ad6-1 in Healthy Volunteers". ClinicalTrials.gov. 9 April 2021. NCT04839042. Retrieved 17 April 2021.
- ↑ "Study of a Severe Acute Respiratory Syndrome-Coronavirus-2 (SARS-CoV-2) Adjuvanted Inactivated Vaccine in Healthy Adults (COVID-19)". ClinicalTrials.gov. 29 April 2021. NCT04866069. Retrieved 30 April 2021.
- ↑ "Safety and Immunogenicity of EXG-5003". ClinicalTrials.gov. 28 April 2021. NCT04863131. Retrieved 2 May 2021.
- ↑ "Icosavax Initiates Phase 1/2 Trial of COVID-19 VLP Vaccine Candidate". Icosavax. 8 June 2021.
- ↑ "A Study to Evaluate the Safety and Immunogenicity of COVID-19 Vaccine (IVX-411) in Healthy Adults". Australian New Zealand Clinical Trials Registry. Retrieved 14 June 2021.
- ↑ "НАЧАТЫ КЛИНИЧЕСКИЕ ИССЛЕДОВАНИЯ СУБЪЕДИНИЧНОЙ ВАКЦИНЫ ПРОТИВ COVID-19, РАЗРАБОТАННОЙ УЧЁНЫМИ НИИПББ". Biosafty and Biotechnology Journal. 15 June 2021.
- ↑ "Reactogenicity, Safety and Immunogenicity of QazCoVac-P COVID-19 Vaccine". ClinicalTrials.gov. 18 June 2021. NCT04930003. Retrieved 22 June 2021.
- ↑ "Safety and Immunogenicity of LNP-nCOV saRNA-02 Vaccine Against SARS-CoV-2, the Causative Agent of COVID-19 (COVAC-Uganda)". ClinicalTrials.gov. 22 June 2021. NCT04934111. Retrieved 22 June 2021.
- ↑ Rujivanarom, Pratch (6 June 2021). "Local jabs yet to join Covid fight". Bangkok Post. Retrieved 8 July 2021.
- ↑ "A Study to Evaluate Safety, Tolerability, and Reactogenicity of an RBD-Fc-based Vaccine to Prevent COVID-19". ClinicalTrials.gov. 7 July 2021. NCT04953078. Retrieved 7 July 2021.
- ↑ "Phase 1 Intranasal Parainfluenza Virus Type 5-SARS CoV-2 S Vaccine in Healthy Adults (CVXGA1-001)". ClinicalTrials.gov. 8 July 2021. NCT04954287. Retrieved 8 July 2021.
- ↑ "FMBA begins clinical trials of its coronavirus vaccine, press service says". Russian News Agency. 19 July 2021. Retrieved 20 July 2021.
- ↑ "The Objectives of This Study Are Study the Immunogenicity, Safety and Tolerability of the Coronavirus Vaccine in Healthy Adult Volunteer Aged 18 to 60 Years". ClinicalTrials.gov. 14 December 2021. NCT05156723. Retrieved 14 December 2021.
- ↑ "Phase I clinical trial to evaluate the safety, tolerability and preliminary immunogenicity of the new coronavirus mRNA vaccine (LVRNA009) in Chinese people aged 18 years and over". chictr.org.cn. 31 July 2021. ChiCTR2100049349. Retrieved 31 July 2021.
- ↑ "A Trial Evaluating the Safety and Immunogenicity of 3 COVID-19 SARS-CoV-2 RNA Vaccines in Healthy Adults". clinicaltrials.gov. 8 September 2021. NCT05037097. Retrieved 8 September 2021.
- ↑ "Clinical Study of the Safety and Immunogenicity of a Recombinant Viral Vector AAV5 (Adeno-Associated Virus Type 5 )-RBD (Receptor Binding Domain)-S Vaccine for the Prevention of Coronavirus Infection (COVID-19) (COVER)". clinicaltrials.gov. 8 September 2021. NCT05037188. Retrieved 8 September 2021.
- ↑ "A study of the safety of EDV nanocells packaged with spike-protein plasmid and glycolipid as a COVID-19 vaccine in healthy volunteers". 27 August 2021. ACTRN12621001159842. Retrieved 17 September 2021.
- ↑ "COVIDITY". Scancell. Retrieved 17 September 2021.
- ↑ "A First Time in Human Phase 1 Open-Label Study of the COVIDITY Vaccine Administered by Needle-free Injection". clinicaltrials.gov. 17 September 2021. NCT05047445. Retrieved 17 September 2021.
- ↑ "Evaluation of the Safety and Immunogenicity of SII Vaccine Constructs Based on the SARS-CoV-2 (COVID-19) Variant in Adults". clinicaltrials.gov. 1 September 2021. NCT05029856. Retrieved 16 September 2021.
- ↑ Chan-hyuk, Kim (1 September 2021). "Eyegene wins approval for trial of mRNA Covid-19 vaccine". Korea Biomedical Review. Retrieved 7 October 2021.
- ↑ "아이진, 부작용 줄인 코로나 mRNA 백신 개발한다". 한국경제TV. 23 September 2021. Retrieved 7 October 2021.
- ↑ "Study to Assess the Safety, Tolerability and Explore the Immunogenicity of EG-COVID in Healthy Adult Volunteers". clinicaltrials.gov. 12 January 2022. NCT05188469. Retrieved 12 January 2022.
- ↑ "To Evaluate the Safety, Tolerability, and Immunogenicity of a PIKA-Adjuvanted Recombinant SARS-CoV-2 Spike (S) Protein Subunit Vaccine in Healthy Individuals". anzctr.org.au. 15 July 2021. ACTRN12621001009808. Retrieved 2 August 2021.
- ↑ "Phase 1 Trial of ChAd68 and Ad5 Adenovirus COVID-19 Vaccines Delivered by Aerosol". clinicaltrials.gov. 26 October 2021. NCT05094609. Retrieved 26 October 2021.
- ↑ "A Study to Evaluate Safety & Immunogenicity of SARS-CoV-2 DNA Vaccine Delivered Intramuscularly Followed by Electroporation for COVID-19". clinicaltrials.gov. 1 November 2021. NCT05102643. Retrieved 1 November 2021.
- ↑ Jaffe-Hoffman, Maayan (11 June 2021). "Israeli oral COVID-19 vaccine en route to clinical trials". The Jerusalem Post. Retrieved 2 November 2021.
- ↑ Jaffe-Hoffman, Maayan (22 July 2021). "Israel to become first in world to test Oravax oral COVID-19 vaccine". The Jerusalem Post. Retrieved 2 November 2021.
- ↑ "Oramed Announces Oravax's Oral COVID-19 Vaccine Has Received South African Approval to Initiate Phase 1 Trial". Cision PR News Wire. 29 October 2021. Retrieved 2 November 2021.
- ↑ "inno.N, 코로나19 백신 후보물질 임상1상 신청". HK inno.N.
- ↑ "Study to Evaluate the Safety and Immunogenicity of SARS-CoV-2 Vaccine (IN-B009) in Healthy Adults (COVID-19)". clinicaltrials.gov. 9 November 2021. NCT05113849. Retrieved 9 November 2021.
- ↑ "Evaluation of Safety and Immunogenicity of a T-Cell Priming Peptide Vaccine Against Coronavirus (naNO-COVID)". clinicaltrials.gov. 9 November 2021. NCT05113862. Retrieved 9 November 2021.
- ↑ "Russian health ministry approves clinical trials of Betuvax-CoV-2 COVID-19 vaccine". Russian News Agency. 27 September 2021. Retrieved 4 November 2021.
- ↑ "Private Russian company starts trials for new COVID-19 vaccine - TASS". Reuters. 15 October 2021. Retrieved 4 November 2021.
- ↑ "Egypt announces clinical trials of its own COVID-19 vaccine". Associated Press News. 15 November 2021. Retrieved 23 November 2021.
- ↑ "Evaluation of Inactivated Vaccine in Healthy Adults Against Coronavirus Disease of 2019 (COVID-19)". clinicaltrials.gov. 22 November 2021. NCT05128721. Retrieved 22 November 2021.
- ↑ "自己増殖型mRNAワクチンVLPCOV-01の第1相試験 並行群間、二重盲検、プラセボ対照ヒト初回投与試験(FIH試験)(COVID-19)" [Clinical research implementation plan / research outline disclosure system]. jrct.niph.go.jp. Japan Registry of Clinical Trials. Retrieved 5 October 2021.
- ↑ "Study of GRT-R910 Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Boost Vaccine in Healthy Volunteers". clinicaltrials.gov. 8 December 2021. NCT05148962. Retrieved 8 December 2021.
- ↑ "Development of a COVID19 Oral Vaccine Consisting of Bacillus Subtilis Spores Expressing and Displaying the Receptor Binding Domain of Spike Protein of SARS-COV2". chictr.org.cn. 28 November 2021. ChiCTR2100053747. Retrieved 28 November 2021.
- ↑ "Phase-I Study to Evaluate the Safety and Immunogenicity of a Prophylactic pDNA Vaccine Candidate Against COVID-19 in Healthy Adults". clinicaltrials.gov. 29 December 2021. NCT05171946. Retrieved 29 December 2021.
- ↑ "신형코로나비루스후보왁찐을 새로 개발". North's State Commission of Science and Technology. Archived from the original on 4 May 2021.
- ↑ "Dự kiến cuối quý 3-2021, Việt Nam sẽ có vaccine phòng Covid-19 đầu tiên". Nhân Dân. 22 March 2021. Retrieved 25 March 2021.
- ↑ "INOVIO's Pan-COVID-19 Vaccine Candidate (INO-4802) Induces Broad Immunity Against Major Viral Variants in Preclinical Studies". Inovio Pharmaceutical. 12 May 2021. Retrieved 10 June 2021.
- ↑ "Bangavax Vaccine: Permission sought for clinical trial". The Daily Star. 18 January 2021.
- ↑ "Bangladesh joins global COVID-19 vaccine race with Bongavax set for clinical trial". Arab News. 8 January 2021.
- ↑ "Bangavax first buzzed with hope, then fizzled". bdnews24. 6 May 2021. Retrieved 9 May 2021.
- ↑ "The vaccine is expected to provide long-lasting protection with a single dose administration with an anticipated safety profile similar to other licensed vaccines for active immunization" (PDF). Indian Immunologicals. 8 April 2020. Retrieved 24 July 2021.
- ↑ Medeiros, Danielle (31 December 2020). "EpiVax and EpiVax Therapeutics Advance COVID-19 Vaccine Program, EPV-CoV-19". EpiVax.
- ↑ "Intravacc announces positive pre-clinical data for its SARS-CoV-2 nose spray vaccine". Intravacc. 7 April 2021. Retrieved 5 September 2021.
- ↑ "Second-Generation COVID-19 Vaccine Candidate, CV2CoV, Demonstrates High Immunogenicity Against Virus Variants in Preclinical Study". CureVac. 13 May 2021.
- ↑ "Sorrento and Dyadic Announce Binding Term Sheet to License Dyadic's Lead COVID-19 Vaccine Candidate "DYAI-100" and C1 Technology for Protein-Based Coronavirus Vaccines and Therapeutics". Sorrento Therapeutics. 11 August 2021. Retrieved 20 August 2021.
- ↑ "Sorrento Announces Its Lead Protein-Based COVID-19 Vaccine Candidate – DYAI-100 – Elicits Strong Neutralizing Immune Responses in Vaccinated Animals Against SARS-CoV-2 and Multiple Major Variants of Concern". Sorrento Therapeutics. 19 August 2021. Retrieved 20 August 2021.
- ↑ "Malaysian mRNA vaccine against Covid-19 under development, says Adham". The Edge. 21 June 2021. Retrieved 22 June 2021.
- ↑ "COVID-19". CureVac. Retrieved 21 December 2020.
- ↑ "A Study to Determine the Safety and Efficacy of SARS-CoV-2 mRNA Vaccine CVnCoV in Adults for COVID-19". ClinicalTrials.gov. 3 December 2020. NCT04652102. Retrieved 22 July 2021.
- ↑ "A Study to Evaluate the Safety and Immunogenicity of Vaccine CVnCoV in Healthy Adults in Germany for COVID-19". ClinicalTrials.gov. 19 December 2020. NCT04674189. Retrieved 23 March 2021.
- ↑ "A Study to Evaluate the Immunogenicity and Safety of the SARS-CoV-2 mRNA Vaccine CVnCoV in Elderly Adults Compared to Younger Adults for COVID-19". ClinicalTrials.gov. 9 April 2021. NCT04838847. Retrieved 26 April 2021.
- ↑ "A Study to Evaluate Safety, Reactogenicity and Immunogenicity of the SARS-CoV-2 mRNA Vaccine CVnCoV in Adults With Co-morbidities for COVID-19". ClinicalTrials.gov. 26 April 2021. NCT04860258. Retrieved 26 April 2021.
- ↑ "COVID-19: A Trial Studying the SARS-CoV-2 mRNA Vaccine CVnCoV to Learn About the Immune Response, the Safety, and the Degree of Typical Vaccination Reactions When CVnCoV is Given at the Same Time as a Flu Vaccine Compared to When the Vaccines Are Separately Given in Adults 60 Years of Age and Older (CV-NCOV-011)". ClinicalTrials.gov. 19 April 2021. NCT04848467. Retrieved 18 June 2021.
- ↑ "COVID-19: A Phase 2b/3, Randomized, Observer-Blinded, Placebo Controlled, Multicenter Clinical Study Evaluating the Efficacy and Safety of Investigational SARS-CoV-2 mRNA Vaccine CVnCoV in Adults 18 Years of Age and Older". EU Clinical Trials Register. 19 November 2020. 2020-003998-22. Retrieved 19 December 2020.
- ↑ "A Study to Evaluate the Safety, Reactogenicity and Immunogenicity of Vaccine CVnCoV in Healthy Adults". ClinicalTrials.gov. 26 June 2020. NCT04449276. Archived from the original on 11 October 2020. Retrieved 14 July 2020.
- ↑ "A Dose-Confirmation Study to Evaluate the Safety, Reactogenicity and Immunogenicity of Vaccine CVnCoV in Healthy Adults for COVID-19". ClinicalTrials.gov. 17 August 2020. NCT04515147. Archived from the original on 23 August 2020. Retrieved 28 August 2020.
- ↑ "EMA starts rolling review of CureVac's COVID-19 vaccine (CVnCoV)". European Medicines Agency (EMA) (Press release). 1 December 2020. Retrieved 12 February 2021.
- ↑ "CureVac seeks Covid-19 shot approval in Switzerland". Swissinfo. 20 April 2021. Retrieved 22 April 2021.
- ↑ "CORVax12: SARS-CoV-2 Spike (S) Protein Plasmid DNA Vaccine Trial for COVID-19 (SARS-CoV-2) (CORVax12)". ClinicalTrials.gov. 13 November 2020. NCT04627675. Retrieved 21 March 2021.
- ↑ "Sanofi and Translate Bio initiate Phase 1/2 clinical trial of mRNA COVID-19 vaccine candidate" (Press release). Sanofi. 12 March 2021. Retrieved 20 March 2021.
- ↑ "Study of mRNA Vaccine Formulation Against COVID-19 in Healthy Adults 18 Years of Age and Older (VAW00001)". ClinicalTrials.gov. 15 March 2021. NCT04798027. Retrieved 20 March 2021.
- ↑ "Safety and Immunogenicity of AdCOVID in Healthy Adults (COVID-19 Vaccine Study)". ClinicalTrials.gov. 22 December 2020. NCT04679909. Retrieved 22 March 2021.
- ↑ "Altimmune Announces Update On AdCOVID Phase 1 Clinical Trial". Altimmune. 29 June 2021. Retrieved 1 July 2021.
- ↑ Ward D, McCormack S (22 May 2020). "Clinical trial to assess the safety of a coronavirus vaccine in healthy men and women". ISRCTN. doi:10.1186/ISRCTN17072692. ISRCTN17072692.
- ↑ "Clinical Trial to Evaluate the Safety and Immunogenicity of the COVID-19 Vaccine (COVID-19-101)". ClinicalTrials.gov. 4 August 2020. NCT04497298. Retrieved 23 March 2021.
- ↑ "A Study on the Safety, Tolerability and Immune Response of SARS-CoV-2 Sclamp (COVID-19) Vaccine in Healthy Adults". ClinicalTrials.gov. 3 August 2020. NCT04495933. Archived from the original on 11 October 2020. Retrieved 4 August 2020.
- ↑ "UQ-CSL V451 Vaccine". precisionvaccinations.com. Retrieved 11 December 2020.
- ↑ "Dose Ranging Trial to Assess Safety and Immunogenicity of V590 (COVID-19 Vaccine) in Healthy Adults (V590-001)". 30 September 2020. Retrieved 26 January 2021.
- ↑ "A Study to Assess Safety, Tolerability, and Immunogenicity of V591 (COVID-19 Vaccine) in Healthy Participants (V591-001)". 4 August 2020. Retrieved 26 January 2021.
- ↑ "Participant Enrollment Begins for Phase I Trial of IAVI-Merck COVID-19 Vaccine Candidate". IAVI. Retrieved 14 March 2021.
- ↑ "V591 SARS-CoV-2 Vaccine". www.precisionvaccinations.com. Retrieved 14 March 2021.
- ↑ "Merck Discontinues Development of SARS-CoV-2/COVID-19 Vaccine Candidates; Continues Development of Two Investigational Therapeutic Candidates". Merck (Press release). 25 January 2021. Retrieved 25 January 2021.
- ↑ "Joint CDC and FDA Statement on Vaccine Boosters". U.S. Food and Drug Administration (FDA) (Press release). 8 July 2021. Archived from the original on 9 July 2021. Retrieved 9 July 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "Coronavirus (COVID-19) Update: FDA Authorizes Additional Vaccine Dose for Certain Immunocompromised Individuals". U.S. Food and Drug Administration (FDA) (Press release). 12 August 2021. Archived from the original on 7 December 2021. Retrieved 13 August 2021.
- ↑ "COVID-19 Vaccines for Moderately to Severely Immunocompromised People". U.S. Centers for Disease Control and Prevention (CDC). 13 August 2021. Retrieved 13 August 2021.
- ↑ "FDA Authorizes Booster Dose of Pfizer-BioNTech COVID-19 Vaccine for Certain Populations". U.S. Food and Drug Administration (FDA) (Press release). 22 September 2021. Archived from the original on 8 December 2021. Retrieved 23 September 2021.
- ↑ "Advisory committee recommends many be offered Covid vaccine boosters". Stat News. 23 September 2021. Retrieved 23 September 2021.
- ↑ "C.D.C. Chief C.D.C. Chief Overrules Agency Panel and Endorses Pfizer Boosters for Frontline Workers". The New York Times. 24 September 2021. Retrieved 24 September 2021.
- ↑ 320.0 320.1 "Coronavirus (COVID-19) Update: FDA Takes Additional Actions on the Use of a Booster Dose for COVID-19 Vaccines". U.S. Food and Drug Administration. 21 October 2021. Retrieved 22 October 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 321.0 321.1 "CDC Expands Eligibility for COVID-19 Booster Shots". Centers for Disease Control and Prevention (CDC). 21 October 2021. Retrieved 22 October 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ "WHO Technical Consultation: Heterologous Prime-Boost Immunization in Ebola vaccine development and testing, licensure and use; 21 November 2014" (PDF). World Health Organization (WHO). Geneva. 9 February 2015. Retrieved 10 December 2021.
- ↑ Lu, S (June 2009). "Heterologous prime-boost vaccination". Current opinion in immunology. 21 (3): 346–51. doi:10.1016/j.coi.2009.05.016. PMID 19500964.
- ↑ Ledford, Heidi (February 2021). "Could mixing COVID vaccines boost immune response?". Nature. 590 (7846): 375–376. Bibcode:2021Natur.590..375L. doi:10.1038/d41586-021-00315-5. ISSN 0028-0836. PMID 33547431. S2CID 231946137.
- ↑ "Angela Merkel receives Moderna dose after first AstraZeneca shot". Al Jazeera. 22 June 2021. Retrieved 28 June 2021.
- ↑ "Getting One Vaccine Is Good. How About Mix-and-Match?". The New York Times. 30 March 2021. Retrieved 30 June 2021.
- ↑ "About". Com-COV. Retrieved 28 June 2021.
- ↑ 328.0 328.1 Stuart, Arabella; Shaw, Robert; Walker, Laura (August 2021). "Comparing coronavirus (COVID-19) vaccine schedule combinations". ISRCTN Registry. doi:10.1186/ISRCTN69254139. S2CID 242713503. ISRCTN69254139.
- ↑ "Safety and Immunogenicity Report from the Com-COV Study – a Single-Blind Randomised Non-Inferiority Trial Comparing Heterologous And Homologous Prime-Boost Schedules with An Adenoviral Vectored and mRNA COVID-19 Vaccine". June 2021. SSRN 3874014.
- ↑ 330.0 330.1 Vichos, Iason; Snape, Matthew (12 March 2021). "Comparing COVID-19 vaccine schedule combinations – stage 2". ISRCTN Registry. doi:10.1186/ISRCTN27841311. S2CID 243068742. ISRCTN27841311. Retrieved 9 July 2021.
- ↑ Faust, Saul (June 2021). "Evaluating COVID-19 Vaccination Boosters". doi:10.1186/ISRCTN73765130. S2CID 240704676. ISRCTN73765130. Retrieved 7 September 2021.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Interim recommendations for heterologous COVID-19 vaccine schedules (Guidance). World Health Organization (WHO). 16 December 2021. WHO/2019-nCoV/vaccines/SAGE_recommendation/heterologous_schedules/2021.1. Retrieved 23 December 2021.
- ↑ "Combination of the first component of Sputnik V vaccine (Sputnik Light vaccine) with vaccines by AstraZeneca, Sinopharm and Moderna demonstrates high safety profile during the study in Argentina's Buenos-Aires province" (Press release). Moscow: Russian Direct Investment Fund. 4 August 2021. Archived from the original on 5 August 2021. Retrieved 5 August 2021.
- ↑ "Study on Sequential Immunization of Recombinant COVID-19 Vaccine (Ad5 Vector) and RBD-based Protein Subunit Vaccine". ClinicalTrials.gov. 6 April 2021. NCT04833101. Retrieved 9 July 2021.
- ↑ "Vaccination With COMIRNATY in Subjects With a VAXZEVRIA First Dose (CombiVacS)". ClinicalTrials.gov. 27 April 2021. NCT04860739. Retrieved 9 July 2021.
- ↑ "Mix and Match of the Second COVID-19 Vaccine Dose for Safety and Immunogenicity (MOSAIC)". ClinicalTrials.gov. 20 May 2021. NCT04894435. Retrieved 9 July 2021.
- ↑ "Compare Immunological Efficacy of a Vaccine Regimen Combining Two Covid19 mRNA Vaccines (Pfizer-BioNTech and Moderna) With That of a Homologous Vaccination of Each Covid19 mRNA Vaccine (ARNCOMBI)". ClinicalTrials.gov. 25 May 2021. NCT04900467. Retrieved 9 July 2021.
- ↑ "Heterologous Vaccination With an Vaxzevria (ChAdOx1-S) Prime and a Comirnaty (BNT162b2) Boost Compared With Homolog Vaccination With Vaxzervria (Prime/Boost) or Comirnaty (Prime/Boost) (HeVacc)". ClinicalTrials.gov. 28 May 2021. NCT04907331. Retrieved 9 July 2021.
- ↑ Kuy, Hugo van der (16 June 2021). "A Trial Among HealthCare Workers (HCW) Vaccinated With Janssen Vaccine: the SWITCH Trial (SWITCH)". ClinicalTrials.gov. NCT04927936. Retrieved 9 July 2021.
- ↑ "Chile realiza primer estudio a nivel mundial sobre uso de dosis de refuerzo en vacunas inactivadas: Aumenta efectividad en prevención y hospitalización por COVID-19" [Chile conducts the first study worldwide on inactivated vaccine boosters: increased effectiveness against disease and hospitalization due to COVID-19] (Press release) (in Spanish). Ministry of Health of Chile. 7 October 2021. Archived from the original on 11 November 2021. Retrieved 11 November 2021.
{{cite press release}}: CS1 maint: unrecognized language (link) - ↑ "Elderly Chileans line up for booster jabs to reinforce CoronaVac vaccine". Reuters. 11 August 2021. Retrieved 17 November 2021.
- ↑ 342.0 342.1 "FDA Briefing Document: Pfizer–BioNTech COVID-19 Vaccine" (PDF). U.S. Food and Drug Administration (FDA). 10 December 2020. Retrieved 1 January 2021.
- ↑ Zimmer C (20 November 2020). "2 Companies Say Their Vaccines Are 95% Effective. What Does That Mean? You might assume that 95 out of every 100 people vaccinated will be protected from Covid-19. But that's not how the math works". The New York Times. Retrieved 21 November 2020.
- ↑ "#DoNotSqueezeMyArm: Doctor Sounds Alarm on How to Properly Inject COVID-19 Vaccine".
- ↑ Ng, Jia Yu (June 2021). "Inadvertent subcutaneous injection of COVID-19 vaccine". Postgraduate Medical Journal. 97 (1148): 400. doi:10.1136/postgradmedj-2021-139870. PMC 7886662. PMID 33589486.
- ↑ "COVID-19 Vaccine Administration Errors and Deviations" (PDF). CDC.
- ↑ Branswell H (2 February 2021). "Comparing three Covid-19 vaccines: Pfizer, Moderna, J&J". Stat. Retrieved 28 February 2021.
- ↑ "Bharat's Intranasal Covid-19 Vaccine Moves Forward". 16 August 2021.
- ↑ Randolph HE, Barreiro LB (May 2020). "Herd Immunity: Understanding COVID-19". Immunity. 52 (5): 737–41. doi:10.1016/j.immuni.2020.04.012. PMC 7236739. PMID 32433946.
- ↑ "The FDA's cutoff for Covid-19 vaccine effectiveness is 50 percent. What does that mean?". NBCNews.com. Retrieved 8 January 2021.
- ↑ "EMA sets 50% efficacy goal – with flexibility – for COVID vaccines". Regulatory Affairs Professionals Society (RAPS). Retrieved 8 January 2021.
- ↑ Krause P, Fleming TR, Longini I, Henao-Restrepo AM, Peto R, Dean NE, et al. (September 2020). "COVID-19 vaccine trials should seek worthwhile efficacy". The Lancet. 396 (10253): 741–43. doi:10.1016/S0140-6736(20)31821-3. PMC 7832749. PMID 32861315.
- ↑ 353.0 353.1 Bartsch SM, O'Shea KJ, Ferguson MC, Bottazzi ME, Wedlock PT, Strych U, et al. (October 2020). "Vaccine Efficacy Needed for a COVID-19 Coronavirus Vaccine to Prevent or Stop an Epidemic as the Sole Intervention". American Journal of Preventive Medicine. 59 (4): 493–503. doi:10.1016/j.amepre.2020.06.011. PMC 7361120. PMID 32778354.
- ↑ "FDA Briefing Document for mRNA 1273". Food and Drug Administration. 17 December 2020. Retrieved 18 August 2021.
{{cite web}}: CS1 maint: url-status (link) - ↑ Anderson, Evan J.; Rouphael, Nadine G.; Widge, Alicia T.; Jackson, Lisa A.; Roberts, Paul C.; Makhene, Mamodikoe; Chappell, James D.; Denison, Mark R.; Stevens, Laura J.; Pruijssers, Andrea J.; McDermott, Adrian B. (17 December 2020). "Safety and Immunogenicity of SARS-CoV-2 mRNA-1273 Vaccine in Older Adults". New England Journal of Medicine. 383 (25): 2427–38. doi:10.1056/NEJMoa2028436. ISSN 0028-4793. PMC 7556339. PMID 32991794.
- ↑ Hunziker, Patrick (24 July 2021). "Personalized-dose Covid-19 vaccination in a wave of virus Variants of Concern: Trading individual efficacy for societal benefit". Precision Nanomedicine. 4 (3): 805–20. doi:10.33218/001c.26101.
- ↑ Dooling, Kathleen (13 August 2021). "Evidence to Recommendations Framework: Additional doses of mRNA COVID-19 vaccines as part of a primary series for immunocompromised" (PDF). CDC Advisory Board for Immunization Practices.
{{cite web}}: CS1 maint: url-status (link) - ↑ Chen, Zhimin; Liu, Kaihui; Liu, Xiuxiang; Lou, Yijun (February 2020). "Modelling epidemics with fractional-dose vaccination in response to limited vaccine supply". Journal of Theoretical Biology. 486: 110085. Bibcode:2020JThBi.48610085C. doi:10.1016/j.jtbi.2019.110085. PMID 31758966. S2CID 208254350.
- ↑ Dean N, Madewell Z (5 March 2021). "Understanding the spectrum of vaccine efficacy measures". The BMJ Opinion. Retrieved 1 March 2021.
- ↑ Voysey M, Costa Clemens SA, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. (March 2021). "Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine: a pooled analysis of four randomised trials". Lancet. 397 (10277): 881–891. doi:10.1016/S0140-6736(21)00432-3. PMC 7894131. PMID 33617777.
- ↑ Falsey AR, Sobieszczyk ME, Hirsch I, Sproule S, Robb ML, Corey L, et al. (16 December 2021). "Phase 3 Safety and Efficacy of AZD1222 (ChAdOx1 nCoV-19) Covid-19 Vaccine". New England Journal of Medicine. 385 (25): 2348–2360. doi:10.1056/NEJMoa2105290.
- ↑ 362.0 362.1 Committee for Medicinal Products for Human Use (19 February 2021). Assessment report: Comirnaty (PDF) (European public assessment report). Corr.1. European Medicines Agency (EMA). COVID-19 Case Definitions; tables 2, 5, 12, 13. EMA/707383/2020. Archived (PDF) from the original on 20 June 2021. Retrieved 23 June 2021.
- ↑ 363.0 363.1 "Pfizer–BioNTech COVID-19 Vaccine – rna ingredient bnt-162b2 injection, suspension". DailyMed. U.S. National Institutes of Health. Retrieved 14 December 2020.
- ↑ 364.0 364.1 364.2 "Janssen COVID-19 Vaccine – ad26.cov2.s injection, suspension". DailyMed. U.S. National Institutes of Health. Retrieved 15 March 2021.
- ↑ "FDA Briefing Document: Janssen Ad26.COV2.S Vaccine for the Prevention of COVID-19". US Food & Drug Administration (FDA). 26 February 2021. Retrieved 1 April 2021.
- ↑ 366.0 366.1 366.2 "Moderna COVID-19 Vaccine – cx-024414 injection, suspension". DailyMed. U.S. National Institutes of Health. Retrieved 20 December 2020.
- ↑ Al Kaabi N, Zhang Y, Xia S, Yang Y, Al Qahtani MM, Abdulrazzaq N, et al. (July 2021). "Effect of 2 Inactivated SARS-CoV-2 Vaccines on Symptomatic COVID-19 Infection in Adults: A Randomized Clinical Trial". JAMA. 326 (1): 35–45. doi:10.1001/jama.2021.8565. PMC 8156175. PMID 34037666.
- ↑ Interim recommendations for use of the inactivated COVID-19 vaccine BIBP developed by China National Biotec Group (CNBG), Sinopharm (Guidance). World Health Organization. 7 May 2021.
- ↑ Logunov DY, Dolzhikova IV, Shcheblyakov DV, Tukhvatulin AI, Zubkova OV, Dzharullaeva AS, et al. (February 2021). "Safety and efficacy of an rAd26 and rAd5 vector-based heterologous prime-boost COVID-19 vaccine: an interim analysis of a randomised controlled phase 3 trial in Russia". Lancet. 397 (10275): 671–681. doi:10.1016/S0140-6736(21)00234-8. PMC 7852454. PMID 33545094.
- ↑ "Summary of Clinical Trial Data of Sinovac's COVID-19 Vaccine (CoronaVac)" (Press release). Sinovac Biotech. 3 April 2021. Retrieved 12 April 2021.
- ↑ Palacios R, Batista AP, Albuquerque CS, Patiño EG, Santos Jd, Tilli Reis Pessoa Conde M, et al. (April 2021). "Efficacy and Safety of a COVID-19 Inactivated Vaccine in Healthcare Professionals in Brazil: The PROFISCOV Study". SSRN 3822780.
- ↑ Toscano C (29 April 2021). "Evidence Assessment: Sinovac/CoronaVac COVID-19 vaccine" (PDF). World Health Organization.
- ↑ Tanriover MD, Doğanay HL, Akova M, Güner HR, Azap A, Akhan S, et al. (July 2021). "Efficacy and safety of an inactivated whole-virion SARS-CoV-2 vaccine (CoronaVac): interim results of a double-blind, randomised, placebo-controlled, phase 3 trial in Turkey". Lancet. 398 (10296): 213–222. doi:10.1016/S0140-6736(21)01429-X. PMC 8266301. PMID 34246358. S2CID 235770533.
- ↑ "WHO issues emergency use listing for eighth COVID-19 vaccine" (Press release). World Health Organization. Retrieved 3 November 2021.
- ↑ Ella R, Reddy S, Blackwelder W, Potdar V, Yadav P, Sarangi V, et al. (December 2021). "Efficacy, safety, and lot-to-lot immunogenicity of an inactivated SARS-CoV-2 vaccine (BBV152): interim results of a randomised, double-blind, controlled, phase 3 trial". Lancet. 398 (10317): 2173–2184. doi:10.1016/S0140-6736(21)02000-6. PMC 8584828. PMID 34774196.
- ↑ "Single dose vaccine, Sputnik Light, authorized for use in Russia" (Press release). Russian Direct Investment Fund. 6 May 2021. Retrieved 1 July 2021.
The single dose Sputnik Light vaccine demonstrated 79.4% efficacy according to analyzed data taken from 28 days after the injection was administered as part of Russia's mass vaccination program between 5 December 2020 and 15 April 2021.
- ↑ Peshimam G, Farooq U (8 February 2021). "CanSinoBIO's COVID-19 vaccine 65.7% effective in global trials, Pakistan official says". Reuters. Islamabad. Retrieved 5 March 2021.
its single-dose regimen and normal refrigerator storage requirement could make it a favourable option for many countries
- ↑ Al Kaabi N, Zhang Y, Xia S, Yang Y, Al Qahtani MM, Abdulrazzaq N, et al. (July 2021). "Effect of 2 Inactivated SARS-CoV-2 Vaccines on Symptomatic COVID-19 Infection in Adults: A Randomized Clinical Trial". JAMA. 326 (1): 35–45. doi:10.1001/jama.2021.8565. PMC 8156175. PMID 34037666.
- ↑ "El candidato vacunal Abdala mostró una eficacia de un 92,28% en su esquema de tres dosis". BioCubaFarma (Press release). 21 June 2021. Retrieved 1 July 2021.
- ↑ "How was the efficacy of the Cuban COVID-19 vaccine candidates calculated?". OnCubaNews English. 27 June 2021. Retrieved 28 June 2021.
- ↑ 381.0 381.1 Toledo-Romani ME, Garcia-Carmenate M, Silva CV, Baldoquin-Rodriguez W, Pérez MM, Gonzalez MC, et al. (6 November 2021). "Efficacy and safety of SOBERANA 02, a COVID-19 conjugate vaccine in heterologous three-dose combination". medRxiv (Preprint). doi:10.1101/2021.10.31.21265703. S2CID 240302516.
- ↑ طاهره نبی الهی قهفرخی (21 November 2021). "نتایج مطالعات ۶ واکسن ایرانی کرونا ارایه شد". ایرنا (in فارسی). Retrieved 23 November 2021.
- ↑ جبارپور, عبدالکریم (2 December 2021). "پاستوکووک ۹۶.۵ درصد از بستری و ابتلای شدید به کرونا پیشگیری میکند". IRNA (in فارسی). Retrieved 9 December 2021.
- ↑ Wadman M, Cohen J (28 January 2021). "Novavax vaccine delivers 89% efficacy against COVID-19 in UK – but is less potent in South Africa". Science. doi:10.1126/science.abg8101.
- ↑ "Novavax Publishes Results of United Kingdom Phase 3 Clinical Trial in New England Journal of Medicine, Demonstrating High Levels of Efficacy of COVID-19 Vaccine". Novavax Inc. (Press release). Retrieved 30 June 2021.
- ↑ "Novavax COVID-19 Vaccine Demonstrates 90% Overall Efficacy and 100% Protection Against Moderate and Severe Disease in PREVENT-19 Phase 3 Trial". Novavax Inc. (Press release). 14 June 2021. Retrieved 15 June 2021.
- ↑ "CureVac Final Data from Phase 2b/3 Trial of First-Generation COVID-19 Vaccine Candidate, CVnCoV, Demonstrates Protection in Age Group of 18 to 60". CureVac (Press release). 30 June 2021. Retrieved 1 July 2021.
- ↑ "Zydus applies to the DCGI for EUA to launch ZyCoV-D, the world's first Plasmid DNA vaccine for COVID-19" (PDF). Cadila Healthcare (Press release). 1 July 2021. Retrieved 1 July 2021.
- ↑ "EpivacCorona vaccine's immunological efficacy proves to be 79% — newspaper". Russian News Agency. 5 August 2021. Retrieved 22 December 2021.
- ↑ "China's Zhifei says unit's COVID shot shows 81.76% efficacy in late-stage trial". Reuters. 27 August 2021.
- ↑ "Clover's COVID-19 Vaccine Candidate Demonstrates 79% Efficacy Against Delta in Global Phase 2/3 SPECTRA Trial Dominated by Variants of Concern and Interest". Clover Biopharmaceutical (Press release). 22 September 2021. Retrieved 11 November 2021.
- ↑ "Medicago and GSK announce positive Phase 3 efficacy and safety results for adjuvanted plant-based COVID-19 vaccine candidate". Medicago (Press release). 7 December 2021. Retrieved 28 December 2021.
- ↑ "Sanofi and GSK to seek regulatory authorization for COVID-19 vaccine". Sanofi (Press release). 23 February 2022. Retrieved 25 February 2022.
- ↑ "Vaccine Effectiveness". Virginia Dept. of Health. 23 August 2021.
- ↑ Holcombe, Madeline; Waldrop, Theresa (11 September 2021). "CDC study: Unvaccinated 11 times more likely to die from Covid-19". CNN. Retrieved 11 September 2021.
{{cite web}}: CS1 maint: url-status (link) - ↑ Scobie, Heather; Johnson, Amelia; Suthar, Amitabh (10 September 2021). [https://web.archive.org/web/20220128163934/https://www.cdc.gov/mmwr/volumes/70/wr/mm7037e1.htm?s_cid=mm7037e1_w Archived] 28 January 2022 at the [[Wayback Machine]][[Category:Webarchive template wayback links]] "Monitoring Incidence of COVID-19 Cases, Hospitalizations, and Deaths, by Vaccination Status". Physiotherapy. 64 (2): 39–40. doi:10.15585/mmwr.mm7037e1. PMID 345296. S2CID 237547342. Retrieved 10 September 2021.
{{cite journal}}: Check|url=value (help)CS1 maint: url-status (link) - ↑ ""Unvaccinated 67 times more likely to die from COVID-19, adjusted data shows"". King5 News. 27 August 2021.
- ↑ Fowlkes, Ashley (2021). "Effectiveness of COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Frontline Workers Before and During B.1.617.2 (Delta) Variant Predominance – Eight U.S. Locations, December 2020–August 2021". MMWR. Morbidity and Mortality Weekly Report. 70 (34): 1167–1169. doi:10.15585/mmwr.mm7034e4. ISSN 0149-2195. PMC 8389394. PMID 34437521.
- ↑ Schreiber, Melody; Chayka, Kyle; Chayka, Kyle; Beyerstein, Lindsay; Beyerstein, Lindsay; Wilson, Jennifer; Wilson, Jennifer; Renault, Marion; Renault, Marion (1 July 2021). "The Delta Covid Variant's Urgent Message for America". The New Republic. ISSN 0028-6583. Retrieved 28 October 2021.
- ↑ "Among the unvaccinated, Delta variant more than doubles risk of hospitalization" Archived 8 November 2021 at the Wayback Machine, Los Angeles Times, 28 August 2021
- ↑ "Coronavirus (COVID-19) booster vaccine". NHS. Government Digital Service. 17 September 2021. Archived from the original on 22 December 2021. Retrieved 11 December 2021.
- ↑ SARS-CoV-2 variants of concern and variants under investigation in England, technical briefing 31 (PDF) (Briefing). Public Health England. 10 December 2021. pp. 3–5, 20–22. GOV-10645. Retrieved 10 December 2021.
- ↑ "What is the difference between efficacy and effectiveness?". Gavi, the Vaccine Alliance (GAVI). 18 November 2020. Retrieved 21 April 2021.
- ↑ Tal A, Cohen E (29 January 2021). "Israel's health data suggests Pfizer and Moderna vaccines may be more effective than we thought". CNN. Retrieved 27 March 2021.
- ↑ Thompson MG, Burgess JL, Naleway AL, Tyner HL, Yoon SK, Meece J, et al. (April 2021). "Interim Estimates of Vaccine Effectiveness of BNT162b2 and mRNA-1273 COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Health Care Personnel, First Responders, and Other Essential and Frontline Workers – Eight U.S. Locations, December 2020 – March 2021" (PDF). MMWR Morb Mortal Wkly Rep. 70 (13): 495–500. doi:10.15585/mmwr.mm7013e3. PMC 8022879. PMID 33793460.
- ↑ Hall VJ, Foulkes S, Saei A, Andrews N, Oguti B, Charlett A, et al. (The SIREN Study Group) (February 2021). "Effectiveness of BNT162b2 mRNA Vaccine Against Infection and COVID-19 Vaccine Coverage in Healthcare Workers in England, Multicentre Prospective Cohort Study (the SIREN Study)". SSRN 3790399.
- ↑ "Real-World Evidence Confirms High Effectiveness of Pfizer-BioNTech COVID-19 Vaccine and Profound Public Health Impact of Vaccination One Year After Pandemic Declared | Pfizer". www.pfizer.com. Archived from the original on 2 February 2023. Retrieved 17 February 2023.
- ↑ Tande AJ, Pollock BD, Shah ND, Farrugia G, Virk A, Swift M, et al. (March 2021). "Impact of the COVID-19 Vaccine on Asymptomatic Infection Among Patients Undergoing Pre-Procedural COVID-19 Molecular Screening". Clinical Infectious Diseases. doi:10.1093/cid/ciab229. PMC 7989519. PMID 33704435.
- ↑ Lopez Bernal J, Andrews N, Gower C, Robertson C, Stowe J, Tessier E, et al. (May 2021). "Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study". BMJ. 373: n1088. doi:10.1136/bmj.n1088. ISSN 1756-1833. PMC 8116636. PMID 33985964.
- ↑ COVID-19 vaccine surveillance report (week 21) (PDF) (Technical report). Public Health England. 27 May 2021. GOV-8481.
- ↑ COVID-19 vaccine surveillance report (week 20) (PDF) (Technical report). Public Health England. 20 May 2021. GOV-8401.
- ↑ 413.0 413.1 413.2 "Ministros de Salud de todo el país consensuaron redoblar esfuerzos para completar los esquemas de vacunación en mayores de 40 años" [Health ministers from all over the country agreed to redouble their efforts to complete vaccination schedules in people over 40 years of age] (in Spanish). Government of Argentina. Ministry of Health (Argentina). 1 July 2021. Retrieved 12 July 2021.
{{cite news}}: CS1 maint: unrecognized language (link) - ↑ 414.0 414.1 414.2 414.3 414.4 Vokó Z, Kiss Z, Surján G, Surján O, Barcza Z, Pályi B, et al. (25 November 2021). "Nationwide effectiveness of five SARS-CoV-2 vaccines in Hungary - The HUN-VE study". Clinical Microbiology and Infection. Table 2. doi:10.1016/j.cmi.2021.11.011. ISSN 1198-743X.
- ↑ Haas EJ, Angulo FJ, McLaughlin JM, Anis E, Singer SR, Khan F, et al. (May 2021). "Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data". Lancet. 397 (10287): 1819–1829. doi:10.1016/S0140-6736(21)00947-8. PMC 8099315. PMID 33964222.
- ↑ Dagan N, Barda N, Kepten E, Miron O, Perchik S, Katz MA, et al. (April 2021). "BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Mass Vaccination Setting". New England Journal of Medicine. 384 (15): 1412–23. doi:10.1056/NEJMoa2101765. PMC 7944975. PMID 33626250.
- ↑ "Real-World Evidence Confirms High Effectiveness of Pfizer–BioNTech COVID-19 Vaccine and Profound Public Health Impact of Vaccination One Year After Pandemic Declared". Pfizer. 11 March 2021. Retrieved 1 April 2021.
- ↑ 418.0 418.1 "Tercer estudio de efectividad de vacunación anti SARS-CoV-2 en Uruguay al 30 de junio de 2021" [Third study of effectiveness of vaccination against SARS-CoV-2 in Uruguay as of June 30, 2021]. Ministerio de Salud Pública (in español). 3 July 2021. Retrieved 7 July 2021.
- ↑ Hall VJ, Foulkes S, Saei A, Andrews N, Oguti B, Charlett A, et al. (May 2021). "COVID-19 vaccine coverage in health-care workers in England and effectiveness of BNT162b2 mRNA vaccine against infection (SIREN): a prospective, multicentre, cohort study". The Lancet. 397 (10286): 1725–35. doi:10.1016/S0140-6736(21)00790-X. ISSN 0140-6736. PMC 8064668. PMID 33901423.
- ↑ 420.0 420.1 Thompson MG, Burgess JL, Naleway AL, Tyner HL, Yoon SK, Meece J, et al. (April 2021). "Interim Estimates of Vaccine Effectiveness of BNT162b2 and mRNA-1273 COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Health Care Personnel, First Responders, and Other Essential and Frontline Workers – Eight U.S. Locations, December 2020 – March 2021" (PDF). MMWR Morb Mortal Wkly Rep. 70 (13): 495–500. doi:10.15585/mmwr.mm7013e3. PMC 8022879. PMID 33793460.
- ↑ Silvia-Valencia J, Soto-Becerra P, Escobar-Agreda S, Fernández-Navarro M, Moscoso-Porras M, Solari L, et al. (22 July 2021). Efectividad de la vacuna BBIBP-CorV para prevenir infección y muerte en personal de salud [Effectiveness of the BBIBP-CorV vaccine to prevent infection and death in health personnel] (Technical report) (in Spanish). Ministry of Health of Peru. Tabla 4, figura 2.
{{cite techreport}}: CS1 maint: unrecognized language (link) - ↑ "Russia's Sputnik V vaccine 97.6% effective in real-world study". Reuters. Moscow. 19 April 2021. Retrieved 21 April 2021.
- ↑ "Sputnik V demonstrates 97.6% efficacy according to analysis of data from 3.8 million vaccinated persons in Russia making it the most efficient COVID-19 vaccine in the world" (Press release). Moscow: Russian Direct Investment Fund. 19 April 2021. Retrieved 21 April 2021.
- ↑ "Sputnik V has demonstrated 97.8% efficacy against COVID cases and 100% efficacy against severe cases of COVID in UAE" (Press release). Moscow: Russian Direct Investment Fund. 29 June 2021. Retrieved 2 July 2021.
- ↑ Jara A, Undurraga EA, González C, Paredes F, Fontecilla T, Jara G, et al. (July 2021). "Effectiveness of an Inactivated SARS-CoV-2 Vaccine in Chile". New England Journal of Medicine. doi:10.1056/NEJMoa2107715. PMC 8279092. PMID 34233097. S2CID 235766915.
- ↑ "Reporte COVID-19: Vacuna Coronavac Tiene Un 90,3% De Efectividad Para Prevenir El Ingreso a UCI" [COVID-19 report: CoronaVac vaccine is 90.3% effective in preventing admission to the ICU]. Ministerio de Salud – Gobierno de Chile (in español). 17 May 2021.
- ↑ Aditya A. "China Sinovac Shot Seen Highly Effective in Real World Study". Bloomberg. Retrieved 15 May 2021.
- ↑ "Kajian Cepat Kemenkes : Vaksin Sinovac Efektif Cegah Kematian" [Ministry of Health Quick Study: Sinovac Vaccine Effectively Prevents Death]. Sehat Negeriku (in Bahasa Indonesia). 12 May 2021. Retrieved 15 May 2021.
- ↑ "Mass vaccination creates healthy oasis in Brazilian city". Reuters. 31 May 2021. Retrieved 2 June 2021.
- ↑ "Sinovac vaccine restores a Brazilian city to near normal". Associated Press. 1 June 2021. Retrieved 2 June 2021.
- ↑ González S, Olszevicki S, Salazar M, Calabria A, Regairaz L, Marín L, et al. (1 October 2021). "Effectiveness of the first component of Gam-COVID-Vac (Sputnik V) on reduction of SARS-CoV-2 confirmed infections, hospitalisations and mortality in patients aged 60-79: a retrospective cohort study in Argentina". EClinicalMedicine. 40. doi:10.1016/j.eclinm.2021.101126. ISSN 2589-5370. PMC 8435263.
- ↑ Fine P, Eames K, Heymann DL (April 2011). ""Herd Immunity": A Rough Guide". Clinical Infectious Diseases. 52 (7): 911–16. doi:10.1093/cid/cir007. ISSN 1058-4838. PMID 21427399.
- ↑ Billah MA, Miah MM, Khan MN (November 2020). "Reproductive number of coronavirus: A systematic review and meta-analysis based on global level evidence". PLOS ONE. 15 (11): e0242128. Bibcode:2020PLoSO..1542128B. doi:10.1371/journal.pone.0242128. PMC 7657547. PMID 33175914.
- ↑ "Science Brief: COVID-19 Vaccines and Vaccination". U.S. Centers for Disease Control and Prevention (CDC). 27 May 2021. Archived from the original on 16 June 2021. Retrieved 17 June 2021.
Substantial reductions in SARS-CoV-2 infections (both symptomatic and asymptomatic) will reduce overall levels of disease, and therefore, viral transmission in the United States. However, investigations are ongoing to assess further the impact of COVID-19 vaccination on transmission.
- ↑ Dyer, Owen (2 August 2021). "Covid-19: Delta infections threaten herd immunity vaccine strategy". BMJ. 374: n1933. doi:10.1136/bmj.n1933. ISSN 1756-1833. PMID 34340962. S2CID 236778544.
- ↑ Katella, Kathy (13 August 2021). "5 Things To Know About the Delta Variant". Yale Medicine News. Retrieved 18 August 2021.
- ↑ Burioni R, Topol EJ (June 2021). "Has SARS-CoV-2 reached peak fitness?". Nature Medicine. 27 (8): 1323–24. doi:10.1038/s41591-021-01421-7. PMID 34155413.
- ↑ 439.0 439.1 Office of the Commissioner (23 February 2021). "Coronavirus (COVID-19) Update: FDA Issues Policies to Guide Medical Product Developers Addressing Virus Variants". U.S. Food and Drug Administration (FDA). Retrieved 7 March 2021.
- ↑ Rella, Simon A.; Kulikova, Yuliya A.; Dermitzakis, Emmanouil T.; Kondrashov, Fyodor A. (30 July 2021). "Rates of SARS-CoV-2 transmission and vaccination impact the fate of vaccine-resistant strains". Scientific Reports. 11 (1): 15729. doi:10.1038/s41598-021-95025-3. ISSN 2045-2322. PMC 8324827. PMID 34330988.
- ↑ Mahase E (March 2021). "Covid-19: Where are we on vaccines and variants?". BMJ. 372: n597. doi:10.1136/bmj.n597. PMID 33653708. S2CID 232093175.
- ↑ 442.0 442.1 442.2 442.3 Weekly epidemiological update on COVID-19 – 8 June 2021 (Situation report). World Health Organization (WHO). 8 June 2021. Table 3. Retrieved 14 June 2021.
- ↑ "Inside the B.1.1.7 Coronavirus Variant". The New York Times. 18 January 2021. Retrieved 29 January 2021.
- ↑ Muik A, Wallisch AK, Sänger B, Swanson KA, Mühl J, Chen W, et al. (March 2021). "Neutralization of SARS-CoV-2 lineage B.1.1.7 pseudovirus by BNT162b2 vaccine-elicited human sera". Science. 371 (6534): 1152–53. Bibcode:2021Sci...371.1152M. doi:10.1126/science.abg6105. PMC 7971771. PMID 33514629.
- ↑ 445.0 445.1 Wang P, Nair MS, Liu L, Iketani S, Luo Y, Guo Y, et al. (March 2021). "Antibody Resistance of SARS-CoV-2 Variants B.1.351 and B.1.1.7". Nature. 593 (7857): 130–35. Bibcode:2021Natur.593..130W. doi:10.1038/s41586-021-03398-2. PMID 33684923.
- ↑ Emary KR, Golubchik T, Aley PK, Ariani CV, Angus BJ, Bibi S, et al. (February 2021). "Efficacy of ChAdOx1 nCoV-19 (AZD1222) Vaccine Against SARS-CoV-2 VOC 202012/01 (B.1.1.7)". SSRN 3779160.
- ↑ Mahase E (February 2021). "Covid-19: Novavax vaccine efficacy is 86% against UK variant and 60% against South African variant". BMJ. 372: n296. doi:10.1136/bmj.n296. PMID 33526412. S2CID 231730012.
- ↑ Kuchler H (25 January 2021). "Moderna develops new vaccine to tackle mutant Covid strain". Financial Times. Retrieved 30 January 2021.
- ↑ Liu Y, Liu J, Xia H, Zhang X, Fontes-Garfias CR, Swanson KA, et al. (February 2021). "Neutralizing Activity of BNT162b2-Elicited Serum – Preliminary Report". The New England Journal of Medicine. doi:10.1056/nejmc2102017. PMID 33596352.
- ↑ 450.0 450.1 Hoffmann M, Arora P, Gross R, Seidel A, Hoernich BF, Hahn AS, et al. (March 2021). "1 SARS-CoV-2 variants B.1.351 and P.1 escape from neutralizing antibodies". Cell. 184 (9): 2384–2393.e12. doi:10.1016/j.cell.2021.03.036. PMC 7980144. PMID 33794143.
- ↑ "Pfizer and BioNTech Confirm High Efficacy and No Serious Safety Concerns Through Up to Six Months Following Second Dose in Updated Topline Analysis of Landmark COVID-19 Vaccine Study". Pfizer (Press release). 1 April 2021. Archived from the original on 17 April 2021. Retrieved 2 April 2021.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedauto - ↑ Francis D, Andy B (6 February 2021). "Oxford/AstraZeneca COVID shot less effective against South African variant: study". Reuters. Retrieved 8 February 2021.
- ↑ 454.0 454.1 "Covid: South Africa halts AstraZeneca vaccine rollout over new variant". BBC News Online. 8 February 2021. Retrieved 8 February 2021.
- ↑ Booth W, Johnson CY (7 February 2021). "South Africa suspends Oxford-AstraZeneca vaccine rollout after researchers report 'minimal' protection against coronavirus variant". The Washington Post. London. Retrieved 8 February 2021.
South Africa will suspend use of the coronavirus vaccine being developed by Oxford University and AstraZeneca after researchers found it provided 'minimal protection' against mild to moderate coronavirus infections caused by the new variant first detected in that country.
- ↑ "A Phase 2A/B, Randomized,Observer-blinded, Placebo-controlled Study to Evaluate the Efficacy, Immunogenicity, and Safety of a SARS-CoV-2 Recombinant Spike Protein Nanoparticle Vaccine (SARS-CoV-2 rS) With Matrix-M1 Adjuvant in South African Adult Subjects Living Without HIV; and Safety and Immunogenicity in Adults Living With HIV". ClinicalTrials.gov. 30 October 2020.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ "PANGO lineages". cov-lineages.org. Retrieved 18 April 2021.
- ↑ Koshy J (8 April 2021). "Coronavirus | Indian 'double mutant' strain named B.1.617". The Hindu.
- ↑ "India's variant-fuelled second wave coincided with spike in infected flights landing in Canada". Toronto Sun. 10 April 2021. Retrieved 10 April 2021.
- ↑ Edara, Venkata-Viswanadh; Pinsky, Benjamin A.; Suthar, Mehul S.; Lai, Lilin; Davis-Gardner, Meredith E.; Floyd, Katharine; Flowers, Maria W.; Wrammert, Jens; Hussaini, Laila; Ciric, Caroline Rose; Bechnak, Sarah; Stephens, Kathy; Graham, Barney S.; Bayat Mokhtari, Elham; Mudvari, Prakriti; Boritz, Eli; Creanga, Adrian; Pegu, Amarendra; Derrien-Colemyn, Alexandrine; Henry, Amy R.; Gagne, Matthew; Douek, Daniel C.; Sahoo, Malaya K.; Sibai, Mamdouh; Solis, Daniel; Webby, Richard J.; Jeevan, Trushar; Fabrizio, Thomas P. (August 2021). "Infection and Vaccine-Induced Neutralizing-Antibody Responses to the SARS-CoV-2 B.1.617 Variants". New England Journal of Medicine. 385 (7): 664–66. doi:10.1056/NEJMc2107799. PMC 8279090. PMID 34233096.
- ↑ Planas, Delphine; Veyer, David; Baidaliuk, Artem; Staropoli, Isabelle; Guivel-Benhassine, Florence; Rajah, Maaran Michael; Planchais, Cyril; Porrot, Françoise; Robillard, Nicolas; Puech, Julien; Prot, Matthieu; Gallais, Floriane; Gantner, Pierre; Velay, Aurélie; Le Guen, Julien; Kassis-Chikhani, Najiby; Edriss, Dhiaeddine; Belec, Laurent; Seve, Aymeric; Courtellemont, Laura; Péré, Hélène; Hocqueloux, Laurent; Fafi-Kremer, Samira; Prazuck, Thierry; Mouquet, Hugo; Bruel, Timothée; Simon-Lorière, Etienne; Rey, Felix A.; Schwartz, Olivier (August 2021). "Reduced sensitivity of SARS-CoV-2 variant Delta to antibody neutralization". Nature. 596 (7871): 276–80. Bibcode:2021Natur.596..276P. doi:10.1038/s41586-021-03777-9. PMID 34237773. S2CID 235775860.
- ↑ Biswas S (25 March 2021). "'Double mutant': What are the risks of India's new Covid-19 variant". BBC News Online. Retrieved 11 April 2021.
- ↑ Haseltine WA (12 April 2021). "An Indian SARS-CoV-2 Variant Lands In California. More Danger Ahead?". Forbes. Retrieved 14 April 2021.
- ↑ "Confirmed cases of COVID-19 variants identified in UK". Public Health England. 15 April 2021. Retrieved 16 April 2021.
- ↑ "expert reaction to VUI-21APR-02/B.1.617.2 being classified by PHE as a variant of concern". Science Media Centre. 7 May 2021. Retrieved 15 May 2021.
- ↑ Khoury DS, Cromer D, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, et al. (May 2021). "Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 infection". Nature Medicine. 27 (7): 1205–11. doi:10.1038/s41591-021-01377-8. ISSN 1546-170X. PMID 34002089. S2CID 234769053.
- ↑ Montgomery J, Ryan M, Engler R, Hoffman D, McClenathan B, Collins L, et al. (June 2021). "Myocarditis Following Immunization With mRNA COVID-19 Vaccines in Members of the US Military". JAMA Cardiology. 6 (10): 1202–1206. doi:10.1001/jamacardio.2021.2833. PMC 8243257. PMID 34185045.
{{cite journal}}: CS1 maint: PMC embargo expired (link) - ↑ Polania Gutierrez JJ, Munakomi S (January 2020). "Intramuscular Injection". StatPearls. PMID 32310581. Archived from the original on 8 December 2020. Retrieved 27 January 2022.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Background document on the mRNA-1273 vaccine (Moderna) against COVID-19 (Report). World Health Organization (WHO). February 2021. hdl:10665/339218. WHO/2019-nCoV/vaccines/SAGE_recommendation/mRNA-1273/background/2021.1. Archived from the original on 13 June 2021. Retrieved 27 January 2022. Lay summary.
{{cite report}}: Cite uses deprecated parameter|lay-url=(help) - ↑ "COVID-19 Vaccine Janssen EPAR". European Medicines Agency (EMA). 5 March 2021. Archived from the original on 15 March 2021. Retrieved 16 March 2021. Text was copied from this source which is © European Medicines Agency. Reproduction is authorized provided the source is acknowledged.
- ↑ "Information about the J&J/Janssen COVID-19 Vaccine". U.S. Centers for Disease Control and Prevention (CDC). 31 March 2021. Archived from the original on 7 April 2021. Retrieved 7 April 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ CDC COVID-19 Response Team (January 2021). "Allergic Reactions Including Anaphylaxis After Receipt of the First Dose of Pfizer-BioNTech COVID-19 Vaccine – United States, December 14–23, 2020" (PDF). MMWR. Morbidity and Mortality Weekly Report. 70 (2): 46–51. doi:10.15585/mmwr.mm7002e1. PMC 7808711. PMID 33444297. Archived (PDF) from the original on 24 January 2021. Retrieved 2 February 2021.
- ↑ "COVID-19 vaccine safety update: Comirnaty" (PDF). European Medicines Agency. 28 January 2021. Archived (PDF) from the original on 2 June 2021. Retrieved 30 January 2021.
- ↑ "About Yellow Card". yellowcard.mhra.gov.uk. Retrieved 3 October 2021.
- ↑ 475.0 475.1 475.2 475.3 "Coronavirus Vaccine - summary of Yellow Card reporting" (PDF). assets.publishing.service.gov.uk. 22 September 2021. Retrieved 3 October 2021.
- ↑ Gabrielle Settles (3 May 2021). "Federal VAERS database is a critical tool for researchers, but a breeding ground for misinformation". PolitiFact.
- ↑ "Safety of COVID-19 Vaccines". U.S. Centers for Disease Control and Prevention (CDC). 11 February 2020. Retrieved 13 July 2021.
- ↑ "Clinical Considerations: Myocarditis after mRNA COVID-19 Vaccines". U.S. Centers for Disease Control and Prevention (CDC). Retrieved 27 June 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ National Center for Immunization and Respiratory Diseases (23 June 2021). "Myocarditis and Pericarditis Following mRNA COVID-19 Vaccination". U.S. Centers for Disease Control and Prevention (CDC). Retrieved 2 July 2021.
- ↑ Greenberger LM, Saltzman LA, Senefeld JW, Johnson PW, DeGennaro LJ, Nichols GL (August 2021). "Antibody response to SARS-CoV-2 vaccines in patients with hematologic malignancies". Cancer Cell. 39 (8): 1031–33. doi:10.1016/j.ccell.2021.07.012. PMC 8295014. PMID 34331856.