| Chronic kidney disease | |
|---|---|
| Other names: Chronic renal disease, kidney failure, impaired kidney function[1] | |
 | |
| Uremic frost on the head in someone with chronic kidney disease | |
| Specialty | Nephrology |
| Symptoms | Early: None[2] Later: Leg swelling, feeling tired, vomiting, loss of appetite, confusion[2] |
| Complications | Heart disease, high blood pressure, anemia[3][4] |
| Duration | Long-term[5] |
| Causes | Diabetes, high blood pressure, glomerulonephritis, polycystic kidney disease[5][6] |
| Diagnostic method | Blood tests, urine tests[7] |
| Treatment | Medications to manage blood pressure, blood sugar, and lower cholesterol, renal replacement therapy, kidney transplant[8][9] |
| Frequency | 753 million (2016)[1] |
| Deaths | 1.2 million (2015)[6] |
Chronic kidney disease (CKD) is a type of kidney disease in which there is gradual loss of kidney function over a period of months to years.[2][5] Initially there are generally no symptoms; later, symptoms may include leg swelling, feeling tired, vomiting, loss of appetite, and confusion.[2] Complications include an increased risk of heart disease, high blood pressure, bone disease, and anemia.[3][4][10]
Causes of chronic kidney disease include diabetes, high blood pressure, glomerulonephritis, and polycystic kidney disease.[5][6] Risk factors include a family history of chronic kidney disease.[2] Diagnosis is by blood tests to measure the estimated glomerular filtration rate (eGFR), and a urine test to measure albumin.[7] Ultrasound or kidney biopsy may be performed to determine the underlying cause.[5] Several severity-based staging systems are in use.[11][12]
Screening at-risk people is recommended.[7] Initial treatments may include medications to lower blood pressure, blood sugar, and cholesterol.[9] Angiotensin converting enzyme inhibitors (ACEIs) or angiotensin II receptor antagonists (ARBs) are generally first-line agents for blood pressure control, as they slow progression of the kidney disease and the risk of heart disease.[13] Loop diuretics may be used to control edema and, if needed, to further lower blood pressure.[14][9][15] NSAIDs should be avoided.[9] Other recommended measures include staying active, and certain dietary changes such as a low-salt diet and the right amount of protein.[9][16] Treatments for anemia and bone disease may also be required.[17][18] Severe disease requires hemodialysis, peritoneal dialysis, or a kidney transplant for survival.[8]
Chronic kidney disease affected 753 million people globally in 2016: 417 million females and 336 million males.[1] In 2015 it caused 1.2 million deaths, up from 409,000 in 1990.[6][19] The causes that contribute to the greatest number of deaths are high blood pressure at 550,000, followed by diabetes at 418,000, and glomerulonephritis at 238,000.[6]
Signs and symptoms[edit | edit source]
CKD is initially without symptoms, and is usually detected on routine screening blood work by either an increase in serum creatinine, or protein in the urine. As the kidney function decreases:
- Blood pressure is increased due to fluid overload and production of vasoactive hormones created by the kidney via the renin–angiotensin system, increasing the risk of developing hypertension and heart failure.
- Urea accumulates, leading to azotemia and ultimately uremia (symptoms ranging from lethargy to pericarditis and encephalopathy). Due to its high systemic concentration, urea is excreted in eccrine sweat at high concentrations and crystallizes on skin as the sweat evaporates ("uremic frost").
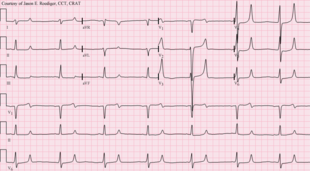
- Potassium accumulates in the blood (hyperkalemia with a range of symptoms including malaise and potentially fatal cardiac arrhythmias). Hyperkalemia usually does not develop until the glomerular filtration rate falls to less than 20–25 ml/min/1.73 m2, at which point the kidneys have decreased ability to excrete potassium. Hyperkalemia in CKD can be exacerbated by acidemia (which leads to extracellular shift of potassium) and from lack of insulin.[20]
- Fluid overload symptoms may range from mild edema to life-threatening pulmonary edema.
- Hyperphosphatemia results from poor phosphate elimination in the kidney. Hyperphosphatemia contributes to increased cardiovascular risk by causing vascular calcification.[21] Circulating concentrations of fibroblast growth factor-23 (FGF-23) increase progressively as the kidney capacity for phosphate excretion declines which may contribute to left ventricular hypertrophy and increased mortality in people with CKD .[22][23]
- Hypocalcemia results from 1,25 dihydroxyvitamin D3 deficiency (caused by high FGF-23 and reduced kidney mass)[24] and resistance to the action of parathyroid hormone.[25] Osteocytes are responsible for the increased production of FGF-23, which is a potent inhibitor of the enzyme 1-alpha-hydroxylase (responsible for the conversion of 25-hydroxycholecalciferol into 1,25 dihydroxyvitamin D3).[26] Later, this progresses to secondary hyperparathyroidism, kidney osteodystrophy, and vascular calcification that further impairs cardiac function. An extreme consequence is the occurrence of the rare condition named calciphylaxis.[27]
- Changes in mineral and bone metabolism that may cause 1) abnormalities of calcium, phosphorus (phosphate), parathyroid hormone, or vitamin D metabolism; 2) abnormalities in bone turnover, mineralization, volume, linear growth, or strength (kidney osteodystrophy); and 3) vascular or other soft-tissue calcification.[10] CKD-mineral and bone disorders have been associated with poor outcomes.[10]
- Metabolic acidosis may result from decreased capacity to generate enough ammonia from the cells of the proximal tubule.[20] Acidemia affects the function of enzymes and increases excitability of cardiac and neuronal membranes by the promotion of hyperkalemia.[28]
- Anemia is common and is especially prevalent in those requiring haemodialysis. It is multifactoral in cause, but includes increased inflammation, reduction in erythropoietin, and hyperuricemia leading to bone marrow suppression.
- In later stages, cachexia may develop, leading to unintentional weight loss, muscle wasting, weakness and anorexia.[29]
- Sexual dysfunction is very common in both men and women with CKD. A majority of men have a reduced sex drive, difficulty obtaining an erection, and reaching orgasm, and the problems get worse with age. A majority of women have trouble with sexual arousal, and painful menstruation and problems with performing and enjoying sex are common.[30]
- People with CKD are more likely than the general population to develop atherosclerosis with consequent cardiovascular disease, an effect that may be at least partly mediated by uremic toxins.[31][unreliable medical source?] People with both CKD and cardiovascular disease have significantly worse prognoses than those with only cardiovascular disease.[32]
Causes[edit | edit source]
The three most common causes of CKD in order of frequency as of 2015 are diabetes mellitus, hypertension, and glomerulonephritis.[33] About one of five adults with hypertension and one of three adults with diabetes have CKD. If the cause is unknown, it is called idiopathic.[34]
By anatomical location[edit | edit source]
- Vascular disease includes large vessel disease such as bilateral kidney artery stenosis and small vessel disease such as ischemic nephropathy, hemolytic-uremic syndrome, and vasculitis.
- Glomerular disease comprises a diverse group and is classified into:
- Primary glomerular disease such as focal segmental glomerulosclerosis and IgA nephropathy (or nephritis)
- Secondary glomerular disease such as diabetic nephropathy and lupus nephritis
- Tubulointerstitial disease includes drug- and toxin-induced chronic tubulointerstitial nephritis, and reflux nephropathy.
- Obstructive nephropathy, as exemplified by bilateral kidney stones and benign prostatic hyperplasia of the prostate gland. Rarely, pinworms infecting the kidney can cause obstructive nephropathy.
Other[edit | edit source]
- Congenital disease such as polycystic kidney disease.
- Mesoamerican nephropathy, is "a new form of kidney disease that could be called agricultural nephropathy".[35] A high and so-far unexplained number of new cases of CKD, referred to as the Mesoamerican nephropathy, has been noted among male workers in Central America, mainly in sugar cane fields in the lowlands of El Salvador and Nicaragua. Heat stress from long hours of piece-rate work at high average temperatures[36][37][38][39] of about 36 °C (96 °F) is suspected, as are agricultural chemicals[40]
Diagnosis[edit | edit source]
Diagnosis of CKD is largely based on history, examination and urine dipstick combined with the measurement of the serum creatinine level (see above). It is important to differentiate CKD from acute kidney injury (AKI) because AKI can be reversible. One diagnostic clue that helps differentiate CKD from AKI is a gradual rise in serum creatinine (over several months or years) as opposed to a sudden increase in the serum creatinine (several days to weeks). In many people with CKD, previous kidney disease or other underlying diseases are already known. A significant number present with CKD of unknown cause.
Screening[edit | edit source]
Screening those who have neither symptoms nor risk factors for CKD is not recommended.[41][42] Those who should be screened include: those with hypertension or history of cardiovascular disease, those with diabetes or marked obesity, those aged > 60 years, subjects with African American ancestry, those with a history of kidney disease in the past, and subjects who have relatives who had kidney disease requiring dialysis.
Screening should include calculation of the estimated GFR (eGFR) from the serum creatinine level, and measurement of urine albumin-to-creatinine ratio (ACR) in a first-morning urine specimen (this reflects the amount of a protein called albumin in the urine), as well as a urine dipstick screen for hematuria.[43]
The glomerular filtration rate (GFR) is derived from the serum creatinine and is proportional to 1/creatinine, i.e. it is a reciprocal relationship:the higher the creatinine, the lower the GFR. It reflects one aspect of kidney function: how efficiently the glomeruli - the filtering units - work. Normal GFR is 90-120 mLs/min. The units of creatinine vary from country to country. But since the glomeruli make up <5% of the mass of the kidney, the GFR does not indicate all aspects of kidney health and function. This can be done by combining the GFR level with the clinical assessment of the person, including fluid status, and measuring the levels of hemoglobin, potassium, phosphate and parathyroid hormone (PTH).
Ultrasound[edit | edit source]
Kidney ultrasonography is useful for diagnostic and prognostic purposes in chronic kidney disease. Whether the underlying pathologic change is glomerular sclerosis, tubular atrophy, interstitial fibrosis or inflammation, the result is often increased echogenicity of the cortex. The echogenicity of the kidney should be related to the echogenicity of either the liver or the spleen (Figure 22 and Figure 23). Moreover, decreased kidney size and cortical thinning are also often seen and especially when disease progresses (Figure 24 and Figure 25). However, kidney size correlates to height, and short persons tend to have small kidneys; thus, kidney size as the only parameter is not reliable.[44]
Chronic renal disease caused by glomerulonephritis with increased echogenicity and reduced cortical thickness. Measurement of kidney length on the US image is illustrated by '+' and a dashed line.[44]
Nephrotic syndrome. Hyperechoic kidney without demarcation of cortex and medulla.[44]
Chronic pyelonephritis with reduced kidney size and focal cortical thinning. Measurement of kidney length on the US image is illustrated by '+' and a dashed line.[44]
End-stage chronic kidney disease with increased echogenicity, homogenous architecture without visible differentiation between parenchyma and renal sinus and reduced kidney size. Measurement of kidney length on the US image is illustrated by '+' and a dashed line.[44]
Additional imaging[edit | edit source]
Additional tests may include nuclear medicine MAG3 scan to confirm blood flow and establish the differential function between the two kidneys. Dimercaptosuccinic acid (DMSA) scans are also used in kidney imaging; with both MAG3 and DMSA being used chelated with the radioactive element technetium-99.[45]
Stages[edit | edit source]
| Chronic kidney disease (CKD) staging - CKD G1-5 A1-3 glomerular filtration rate (GFR) and albumin/creatinine ratio (ACR) | ||||||
|---|---|---|---|---|---|---|
| ACR | ||||||
| A1 | A2 | A3 | ||||
| Normal to mildly increased | Moderately increased | Severely increased | ||||
| <30 | 30-300 | >300 | ||||
| G F R | ||||||
| G1 | Normal | 90+ | 1 if kidney damage present | 1 | 2 | |
| G2 | Mildly decreased | 60-89 | 1 if kidney damage present | 1 | 2 | |
| G3a | Mildly to moderately decreased | 45-59 | 1 | 2 | 3 | |
| G3b | Moderately to severely decreased | 30-44 | 2 | 3 | 3 | |
| G4 | Severely decreased | 15-29 | 3 | 4+ | 4+ | |
| G5 | Kidney failure | <15 | 4+ | 4+ | 4+ | |
| Numbers 1 - 4 indicates risk of progression as well as frequency of monitoring (number of times a year). Kidney Disease Improving Global Outcomes - KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease [46] | ||||||
A glomerular filtration rate (GFR) ≥ 60 ml/min/1.73 m2 is considered normal without chronic kidney disease if there is no kidney damage present.
Kidney damage is defined signs of damage seen in blood, urine, or imaging studies which includes lab albumin/creatinine ratio (ACR) ≥ 30.[47] All people with a GFR <60 ml/min/1.73 m2 for 3 months are defined as having chronic kidney disease.[47]
Protein in the urine is regarded as an independent marker for worsening of kidney function and cardiovascular disease. Hence, British guidelines append the letter "P" to the stage of chronic kidney disease if protein loss is significant.[48]
- Stage 1: Slightly diminished function; kidney damage with normal or relatively high GFR (≥90 ml/min/1.73 m2) and persistent albuminuria. Kidney damage is defined as pathological abnormalities or markers of damage, including abnormalities in blood or urine tests or imaging studies.[47]
- Stage 2: Mild reduction in GFR (60–89 ml/min/1.73 m2) with kidney damage. Kidney damage is defined as pathological abnormalities or markers of damage, including abnormalities in blood or urine tests or imaging studies.[47]
- Stage 3: Moderate reduction in GFR (30–59 ml/min/1.73 m2):.[47] British guidelines distinguish between stage 3A (GFR 45–59) and stage 3B (GFR 30–44) for purposes of screening and referral.[48]
- Stage 4: Severe reduction in GFR (15–29 ml/min/1.73 m2)[47] Preparation for kidney replacement therapy.
- Stage 5: Established kidney failure (GFR <15 ml/min/1.73 m2), permanent kidney replacement therapy,[47] or end-stage kidney disease.
The term "non-dialysis-dependent chronic kidney disease" (NDD-CKD) is a designation used to encompass the status of those persons with an established CKD who do not yet require the life-supporting treatments for kidney failure known as kidney replacement therapy (RRT, including maintenance dialysis or kidney transplantation). The condition of individuals with CKD, who require either of the two types of kidney replacement therapy (dialysis or transplant), is referred to as the end-stage kidney disease (ESKD). Hence, the start of the ESKD is practically the irreversible conclusion of the NDD-CKD. Even though the NDD-CKD status refers to the status of persons with earlier stages of CKD (stages 1 to 4), people with advanced stage of CKD (stage 5), who have not yet started kidney replacement therapy, are also referred to as NDD-CKD.
Management[edit | edit source]
Apart from controlling other risk factors, the goal of therapy is to slow down or halt the progression of CKD. Control of blood pressure and treatment of the original disease are the broad principles of management.
Blood pressure[edit | edit source]
Angiotensin converting enzyme inhibitors (ACEIs) or angiotensin II receptor antagonists (ARBs) are recommended as first-line agents since they have been found to slow the decline of kidney function, relative to a more rapid decline in those not on one of these agents.[13] They have also been found to reduce the risk of major cardiovascular events such as myocardial infarction, stroke, heart failure, and death from cardiovascular disease when compared to placebo in individuals with CKD.[13] ACEIs may be superior to ARBs for protection against progression to kidney failure and death from any cause in those with CKD.[13] Aggressive blood pressure lowering decreases peoples risk of death.[49]
Other measures[edit | edit source]
- Aggressive treatment of high blood lipids is recommended.[50]
- A low-protein, low-salt diet may result in slower progression of CKD and reduction in proteinuria as well as controlling symptoms of advanced CKD to delay dialysis start.[51] A tailored low-protein diet, designed for low acidity, may help prevent damage to kidneys for people with CKD.[52]
- Anemia - A target hemoglobin level of 9–12 g/dL is recommended;[53][54] raising hemoglobin levels to the normal range has not been found to be of benefit.[55]
- Guidelines recommend treatment with parenteral iron prior to treatment with erythropoietin.
- Replacement of erythropoietin is often necessary in people with advanced disease.[56]
- It is unclear if androgens improve anemia.[57]
- Calcitriol is recommended for vitamin D deficiency and control of metabolic bone disease.
- Phosphate binders are used to control the serum phosphate levels, which are usually elevated in advanced chronic kidney disease.
- Phosphodiesterase-5 inhibitors and zinc may improve sexual dysfunction in men.[30]
Referral to a nephrologist[edit | edit source]
Guidelines for referral to a nephrologist vary between countries. Most agree that nephrology referral is required by Stage 4 CKD (when eGFR/1.73m2 is less than 30 ml/min; or decreasing by more than 3 ml/min/year).[58]
It may also be useful at an earlier stage (e.g. CKD3) when urine albumin-to-creatinine ratio is more than 30 mg/mmol, when blood pressure is difficult to control, or when hematuria or other findings suggest either a primarily glomerular disorder or secondary disease amenable to specific treatment. Other benefits of early nephrology referral include proper education regarding options for kidney replacement therapy as well as pre-emptive transplantation, and timely workup and placement of an arteriovenous fistula in those people with chronic kidney disease opting for future hemodialysis.
Renal replacement therapy[edit | edit source]
At stage 5 CKD, kidney replacement therapy is usually required, in the form of either dialysis or a kidney transplant.
In CKD numerous uremic toxins accumulate in the blood. Even when ESKD (largely synonymous with CKD5) is treated with dialysis, the toxin levels do not go back to normal as dialysis is not that efficient. Similarly, after a kidney transplant, the levels may not go back to normal as the transplanted kidney may not work 100%. If it does, the creatinine level is often normal. The toxins show various cytotoxic activities in the serum and have different molecular weights, and some of them are bound to other proteins, primarily to albumin. Uremic toxins are classified into three groups as small water-soluble solutes, middle molecular-weight solutes, and protein-bound solutes.[59] Hemodialysis with high-flux dialysis membrane, long or frequent treatment, and increased blood/dialysate flow has improved removal of water-soluble small molecular weight uremic toxins. Middle molecular weight molecules are removed more effectively with hemodialysis using a high-flux membrane, hemodiafiltration and hemofiltration. However, conventional dialysis treatment is limited in its ability to remove protein-bound uremic toxins.[60]
Prognosis[edit | edit source]
CKD increases the risk of cardiovascular disease, and people with CKD often have other risk factors for heart disease, such as high blood lipids. The most common cause of death in people with CKD is cardiovascular disease rather than kidney failure.
Chronic kidney disease results in worse all-cause mortality (the overall death rate) which increases as kidney function decreases.[61] The leading cause of death in chronic kidney disease is cardiovascular disease, regardless of whether there is progression to stage 5.[61][62][63]
While kidney replacement therapies can maintain people indefinitely and prolong life, the quality of life is negatively affected.[64][65] Kidney transplantation increases the survival of people with stage 5 CKD when compared to other options;[66][67] however, it is associated with an increased short-term mortality due to complications of the surgery. Transplantation aside, high-intensity home hemodialysis appears to be associated with improved survival and a greater quality of life, when compared to the conventional three-times-a-week hemodialysis and peritoneal dialysis.[68]
People with ESKD are at increased overall risk for cancer.[69] This risk is particularly high in younger people and gradually diminishes with age.[69] Medical specialty professional organizations recommend that physicians do not perform routine cancer screening in people with limited life expectancies due to ESKD because evidence does not show that such tests lead to improved outcomes.[70][71]
Epidemiology[edit | edit source]
About one in ten people have chronic kidney disease. In Canada 1.9 to 2.3 million people were estimated to have CKD in 2008.[55] CKD affected an estimated 16.8% of U.S. adults aged 20 years and older in the period from 1999 to 2004.[72] In 2007 8.8% of the population of Great Britain and Northern Ireland had symptomatic CKD.[73]
Chronic kidney disease was the cause of 956,000 deaths globally in 2013, up from 409,000 deaths in 1990.[19]
Race[edit | edit source]
African Americans, American Indians, Hispanics, and South Asians, particularly those from Pakistan, Sri Lanka, Bangladesh, and India, are at high risk of developing CKD. African Americans are at greater risk due to the number of people affected with hypertension among them. As an example, 37% of ESKD cases in African Americans can be attributed to high blood pressure, compared with 19% among Caucasians.[74] Treatment efficacy also differs between racial groups. Administration of antihypertensive drugs generally halts disease progression in white populations but has little effect in slowing kidney disease among black people, and additional treatment such as bicarbonate therapy is often required.[74] While lower socioeconomic status contributes to the number of people affected with CKD, differences in the number of people affected by CKD are still evident between African Americans and Whites when controlling for environmental factors.[74]
Society and culture[edit | edit source]
The International Society of Nephrology is an international body representing specialists in kidney diseases.
United States[edit | edit source]
- The National Kidney Foundation is a national organization representing people with chronic kidney diseases and professionals who treat kidney diseases.
- The American Kidney Fund is a national nonprofit organization providing treatment-related financial assistance to one of every five people undergoing dialysis each year.
- The Renal Support Network is a nonprofit, patient-focused, patient-run organization that provides nonmedical services to those affected by CKD.
- The American Association of Kidney Patients is a nonprofit, patient-centric group focused on improving the health and well-being of CKD and people undergoing dialysis .
- The Renal Physicians Association is an association representing nephrology professionals.
United Kingdom[edit | edit source]
It was said to be costing the British NHS about £1.5 billion a year in 2020.[75]
The UK National Kidney Federation and British Kidney Patient Association (BKPA) represents people with chronic kidney disease. The Renal Association represents Kidney physicians and works closely with the National Service Framework for kidney disease.
Australia[edit | edit source]
Kidney Health Australia serves that country.
Other animals[edit | edit source]
The total rate of CKD in dogs was 16 cases per 10,000 years. The mortality rate of CKD was 10 deaths per 10,000. The breeds with the highest rates were the Bernese mountain dog, miniature schnauzer and boxer. The Swedish elkhound, Siberian husky and Finnish spitz were the breeds with the lowest rates.[76][77]
Research[edit | edit source]
Currently, several compounds are in development for the treatment of CKD. These include the angiotensin receptor blocker (ARB) olmesartan medoxomil; and sulodexide, a mixture of low molecular weight heparin and dermatan sulfate.[78][79]
Unbiased research with complete reporting is required to determine the safety and effectiveness of acupuncture to treat depression, pain, sleep problems, and uraemic pruritus in people who are undergoing dialysis treatments on a regular basis.[80]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Bikbov B, Perico N, Remuzzi G (23 May 2018). "Disparities in Chronic Kidney Disease Prevalence among Males and Females in 195 Countries: Analysis of the Global Burden of Disease 2016 Study". Nephron. 139 (4): 313–318. doi:10.1159/000489897. PMID 29791905. Archived (PDF) from the original on 28 August 2021. Retrieved 27 May 2020.
- ↑ 2.0 2.1 2.2 2.3 2.4 "What Is Chronic Kidney Disease?". National Institute of Diabetes and Digestive and Kidney Diseases. June 2017. Archived from the original on 21 December 2017. Retrieved 19 December 2017.
- ↑ 3.0 3.1 Liao MT, Sung CC, Hung KC, Wu CC, Lo L, Lu KC (2012). "Insulin resistance in patients with chronic kidney disease". Journal of Biomedicine & Biotechnology. 2012: 691369. doi:10.1155/2012/691369. PMC 3420350. PMID 22919275.
- ↑ 4.0 4.1 "Kidney Failure". MedlinePlus. Archived from the original on 4 July 2016. Retrieved 11 November 2017.
- ↑ 5.0 5.1 5.2 5.3 5.4 "What is renal failure?". Johns Hopkins Medicine. Archived from the original on 18 June 2017. Retrieved 18 December 2017.
- ↑ 6.0 6.1 6.2 6.3 6.4 GBD 2015 Mortality Causes of Death Collaborators (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ↑ 7.0 7.1 7.2 "Chronic Kidney Disease Tests & Diagnosis". National Institute of Diabetes and Digestive and Kidney Diseases. October 2016. Archived from the original on 22 December 2017. Retrieved 19 December 2017.
- ↑ 8.0 8.1 "Kidney Failure". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 27 July 2018. Retrieved 11 November 2017.
- ↑ 9.0 9.1 9.2 9.3 9.4 "Managing Chronic Kidney Disease". National Institute of Diabetes and Digestive and Kidney Diseases. October 2016. Archived from the original on 2017-12-21. Retrieved 2017-12-19.
- ↑ 10.0 10.1 10.2 KDIGO: Kidney Disease Improving Global Outcomes (August 2009). "KDIGO Clinical Practice Guideline for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD)" (PDF). Kidney Int. 76 (Suppl 113). Archived from the original (PDF) on 2016-12-13.
- ↑ "Summary of Recommendation Statements". Kidney International Supplements. 3 (1): 5–14. January 2013. doi:10.1038/kisup.2012.77. PMC 4284512. PMID 25598998.
- ↑ Ferri, Fred F. (2017). Ferri's Clinical Advisor 2018 E-Book: 5 Books in 1. Elsevier Health Sciences. pp. 294–295. ISBN 9780323529570. Archived from the original on 2021-08-28. Retrieved 2020-05-27.
- ↑ 13.0 13.1 13.2 13.3 Xie X, Liu Y, Perkovic V, Li X, Ninomiya T, Hou W, et al. (May 2016). "Renin-Angiotensin System Inhibitors and Kidney and Cardiovascular Outcomes in Patients With CKD: A Bayesian Network Meta-analysis of Randomized Clinical Trials". American Journal of Kidney Diseases (Systematic Review & Meta-Analysis). 67 (5): 728–41. doi:10.1053/j.ajkd.2015.10.011. PMID 26597926.
- ↑ Wile D (September 2012). "Diuretics: a review". Annals of Clinical Biochemistry. 49 (Pt 5): 419–31. doi:10.1258/acb.2011.011281. PMID 22783025.
- ↑ James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. (February 2014). "2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8)". JAMA. 311 (5): 507–20. doi:10.1002/14651858.CD011339.pub2. PMC 6485696. PMID 24352797.
- ↑ "Eating Right for Chronic Kidney Disease | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Archived from the original on 2 October 2019. Retrieved 5 September 2019.
- ↑ "Anemia in Chronic Kidney Disease". National Institute of Diabetes and Digestive and Kidney Diseases. July 2016. Archived from the original on 21 December 2017. Retrieved 19 December 2017.
- ↑ "Mineral & Bone Disorder in Chronic Kidney Disease". National Institute of Diabetes and Digestive and Kidney Diseases. November 2015. Archived from the original on 22 December 2017. Retrieved 19 December 2017.
- ↑ 19.0 19.1 GBD 2013 Mortality Causes of Death Collaborators (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442. Table 2, p. 137

- ↑ 20.0 20.1 "Chronic Kidney Disease". medscape. 2018-09-16. Archived from the original on 2014-04-07.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Hruska KA, Mathew S, Lund R, Qiu P, Pratt R (July 2008). "Hyperphosphatemia of chronic kidney disease". Kidney International. 74 (2): 148–57. doi:10.1038/ki.2008.130. PMC 2735026. PMID 18449174.
- ↑ Faul C, Amaral AP, Oskouei B, Hu MC, Sloan A, Isakova T, et al. (November 2011). "FGF23 induces left ventricular hypertrophy". The Journal of Clinical Investigation. 121 (11): 4393–408. doi:10.1172/JCI46122. PMC 3204831. PMID 21985788.
- ↑ Gutiérrez OM, Mannstadt M, Isakova T, Rauh-Hain JA, Tamez H, Shah A, et al. (August 2008). "Fibroblast growth factor 23 and mortality among patients undergoing hemodialysis". The New England Journal of Medicine. 359 (6): 584–92. doi:10.1056/NEJMoa0706130. PMC 2890264. PMID 18687639.
- ↑ Bacchetta J, Sea JL, Chun RF, Lisse TS, Wesseling-Perry K, Gales B, et al. (January 2013). "Fibroblast growth factor 23 inhibits extrarenal synthesis of 1,25-dihydroxyvitamin D in human monocytes". Journal of Bone and Mineral Research. 28 (1): 46–55. doi:10.1002/jbmr.1740. PMC 3511915. PMID 22886720.
- ↑ Bover J, Jara A, Trinidad P, Rodriguez M, Martin-Malo A, Felsenfeld AJ (August 1994). "The calcemic response to PTH in the rat: effect of elevated PTH levels and uremia". Kidney International. 46 (2): 310–7. doi:10.1038/ki.1994.276. PMID 7967341.
- ↑ Longo et al., Harrison's Principles of Internal Medicine, 18th ed., p. 3109
- ↑ Brandenburg VM, Cozzolino M, Ketteler M (2011). "Calciphylaxis: a still unmet challenge". Journal of Nephrology. 24 (2): 142–8. doi:10.5301/jn.2011.6366. PMID 21337312.
- ↑ Adrogué HJ, Madias NE (September 1981). "Changes in plasma potassium concentration during acute acid-base disturbances". The American Journal of Medicine. 71 (3): 456–67. doi:10.1016/0002-9343(81)90182-0. PMID 7025622.
- ↑ Mak RH, Ikizler AT, Kovesdy CP, Raj DS, Stenvinkel P, Kalantar-Zadeh K (March 2011). "Wasting in chronic kidney disease". Journal of Cachexia, Sarcopenia and Muscle. 2 (1): 9–25. doi:10.1007/s13539-011-0019-5. PMC 3063874. PMID 21475675.
- ↑ 30.0 30.1 Vecchio M, Navaneethan SD, Johnson DW, Lucisano G, Graziano G, Saglimbene V, et al. (December 2010). "Interventions for treating sexual dysfunction in patients with chronic kidney disease" (PDF). The Cochrane Database of Systematic Reviews (12): CD007747. doi:10.1002/14651858.CD007747.pub2. PMID 21154382. Archived (PDF) from the original on 2021-08-28. Retrieved 2019-09-27.
- ↑ Hoyer, FF; Nahrendorf, M (2 January 2019). "Uremic Toxins Activate Macrophages". Circulation. 139 (1): 97–100. doi:10.1161/CIRCULATIONAHA.118.037308. PMC 6394415. PMID 30592654.
- ↑ Damman K, Valente MA, Voors AA, O'Connor CM, van Veldhuisen DJ, Hillege HL (February 2014). "Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis". European Heart Journal. 35 (7): 455–69. doi:10.1093/eurheartj/eht386. PMID 24164864. Archived from the original on 2016-02-23. Retrieved 2016-01-06.
- ↑ GBD 2015 Disease Injury Incidence Prevalence Collaborators (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- ↑ "United States Renal Data System (USRDS)". Archived from the original on 2007-02-13.
- ↑ Orantes CM, Herrera R, Almaguer M, Brizuela EG, Núñez L, Alvarado NP, et al. (April 2014). "Epidemiology of chronic kidney disease in adults of Salvadoran agricultural communities". MEDICC Review. 16 (2): 23–30. PMID 24878646. Archived from the original on 2021-06-09. Retrieved 2014-10-12.
- ↑ Tangri N (29 July 2013). "MesoAmerican Nephropathy: A New Entity". eAJKD. National Kidney Foundation. Archived from the original on 4 January 2014. Retrieved 1 October 2013.
- ↑ Wesseling C, Crowe J, Hogstedt C, Jakobsson K, Lucas R, Wegman DH (November 2013). "The epidemic of chronic kidney disease of unknown etiology in Mesoamerica: a call for interdisciplinary research and action". American Journal of Public Health. 103 (11): 1927–30. doi:10.2105/AJPH.2013.301594. PMC 3828726. PMID 24028232.
- ↑ Johnson RJ, Sánchez-Lozada LG (October 2013). "Chronic kidney disease: Mesoamerican nephropathy--new clues to the cause". Nature Reviews. Nephrology. 9 (10): 560–1. doi:10.1038/nrneph.2013.174. PMID 23999393.
- ↑ Roncal Jimenez CA, Ishimoto T, Lanaspa MA, Rivard CJ, Nakagawa T, Ejaz AA, et al. (August 2014). "Fructokinase activity mediates dehydration-induced renal injury". Kidney International. 86 (2): 294–302. doi:10.1038/ki.2013.492. PMC 4120672. PMID 24336030.
- ↑ Chavkin, Sasha; Greene, Ronnie (12 December 2011). "Thousands of sugar cane workers die as wealthy nations stall on solutions". International Consortium of Investigative Journalists. Archived from the original on 26 November 2012. Retrieved November 26, 2012.
- ↑ Qaseem A, Hopkins RH, Sweet DE, Starkey M, Shekelle P (December 2013). "Screening, monitoring, and treatment of stage 1 to 3 chronic kidney disease: A clinical practice guideline from the American College of Physicians". Annals of Internal Medicine. 159 (12): 835–47. doi:10.7326/0003-4819-159-12-201312170-00726. PMID 24145991.
- ↑ Weckmann GF, Stracke S, Haase A, Spallek J, Ludwig F, Angelow A, et al. (October 2018). "Diagnosis and management of non-dialysis chronic kidney disease in ambulatory care: a systematic review of clinical practice guidelines". BMC Nephrology. 19 (1): 258. doi:10.1186/s12882-018-1048-5. PMC 6180496. PMID 30305035.
- ↑ Johnson, David (2011-05-02). "Chapter 4: CKD Screening and Management: Overview". In Daugirdas, John (ed.). Handbook of Chronic Kidney Disease Management. Lippincott Williams and Wilkins. pp. 32–43. ISBN 978-1-58255-893-6.
{{cite book}}:|access-date=requires|url=(help);|archive-url=requires|url=(help); Unknown parameter|chapterurl=ignored (help) - ↑ 44.0 44.1 44.2 44.3 44.4 Content initially copied from: Hansen KL, Nielsen MB, Ewertsen C (December 2015). "Ultrasonography of the Kidney: A Pictorial Review". Diagnostics. 6 (1): 2. doi:10.3390/diagnostics6010002. PMC 4808817. PMID 26838799. (CC-BY 4.0) Archived 2017-10-16 at the Wayback Machine
- ↑ "Kidney scans". Singlehealth. Archived from the original on 2021-08-28.
- ↑ CKD Evaluation and Management Archived 2019-05-01 at the Wayback Machine 2012. Kidney Disease Improving Global Outcomes (KDIGO). Retrieved 2019-07-06.
- ↑ 47.0 47.1 47.2 47.3 47.4 47.5 47.6 National Kidney Foundation (2002). "K/DOQI clinical practice guidelines for chronic kidney disease". Archived from the original on 2005-04-15. Retrieved 2008-06-29.
- ↑ 48.0 48.1 National Institute for Health and Clinical Excellence. Clinical guideline 73: Chronic kidney disease. London, 2008.
- ↑ Malhotra R, Nguyen HA, Benavente O, Mete M, Howard BV, Mant J, et al. (October 2017). "Association Between More Intensive vs Less Intensive Blood Pressure Lowering and Risk of Mortality in Chronic Kidney Disease Stages 3 to 5: A Systematic Review and Meta-analysis". JAMA Internal Medicine. 177 (10): 1498–1505. doi:10.1001/jamainternmed.2017.4377. PMC 5704908. PMID 28873137.
- ↑ Chauhan V, Vaid M (November 2009). "Dyslipidemia in chronic kidney disease: managing a high-risk combination". Postgraduate Medicine. 121 (6): 54–61. doi:10.3810/pgm.2009.11.2077. PMID 19940417.
- ↑ Kalantar-Zadeh K, Fouque D (November 2017). "Nutritional Management of Chronic Kidney Disease". The New England Journal of Medicine. 377 (18): 1765–1776. doi:10.1056/NEJMra1700312. PMID 29091561.
- ↑ Passey C (May 2017). "Reducing the Dietary Acid Load: How a More Alkaline Diet Benefits Patients With Chronic Kidney Disease". J Ren Nutr (Review). 27 (3): 151–160. doi:10.1053/j.jrn.2016.11.006. PMID 28117137.
- ↑ Locatelli F, Aljama P, Canaud B, Covic A, De Francisco A, Macdougall IC, et al. (September 2010). "Target haemoglobin to aim for with erythropoiesis-stimulating agents: a position statement by ERBP following publication of the Trial to reduce cardiovascular events with Aranesp therapy (TREAT) study". Nephrology, Dialysis, Transplantation. 25 (9): 2846–50. doi:10.1093/ndt/gfq336. PMID 20591813. Archived from the original on 2021-08-28. Retrieved 2014-12-24.
- ↑ Clement FM, Klarenbach S, Tonelli M, Johnson JA, Manns BJ (June 2009). "The impact of selecting a high hemoglobin target level on health-related quality of life for patients with chronic kidney disease: a systematic review and meta-analysis". Archives of Internal Medicine. 169 (12): 1104–12. doi:10.1001/archinternmed.2009.112. PMID 19546410.
- ↑ 55.0 55.1 Levin A, Hemmelgarn B, Culleton B, Tobe S, McFarlane P, Ruzicka M, et al. (November 2008). "Guidelines for the management of chronic kidney disease". CMAJ. 179 (11): 1154–62. doi:10.1503/cmaj.080351. PMC 2582781. PMID 19015566.
- ↑ "Anaemia management in people with chronic kidney disease (CG114)". NICE Clinical Guideline. UK National Institute for Health and Care Excellence. February 2011. Archived from the original on 2014-01-04. Retrieved 2014-01-04.
- ↑ journal|last1=Yang|first1=Q|last2=Abudou|first2=M|last3=Xie|first3=XS|last4=Wu|first4=T|title=Androgens for the anaemia of chronic kidney disease in adults.|journal=The Cochrane Database of Systematic Reviews|date=Oct 9, 2014|volume=10|issue=10|pages=CD006881|pmid=25300168|doi=10.1002/14651858.CD006881.pub2}}
- ↑ "CKD Stage 4". davita. Archived from the original on 2020-01-03.
- ↑ Vanholder R, De Smet R, Glorieux G, Argilés A, Baurmeister U, Brunet P, et al. (May 2003). "Review on uremic toxins: classification, concentration, and interindividual variability". Kidney International. 63 (5): 1934–43. doi:10.1046/j.1523-1755.2003.00924.x. PMID 12675874.
- ↑ Yamamoto, Suguru; Kazama, Junichiro James; Wakamatsu, Takuya; Takahashi, Yoshimitsu; Kaneko, Yoshikatsu; Goto, Shin; Narita, Ichiei (14 September 2016). "Removal of uremic toxins by renal replacement therapies: a review of current progress and future perspectives". Renal Replacement Therapy. 2 (1). doi:10.1186/s41100-016-0056-9.
- ↑ 61.0 61.1 Perazella MA, Khan S (March 2006). "Increased mortality in chronic kidney disease: a call to action". The American Journal of the Medical Sciences. 331 (3): 150–3. doi:10.1097/00000441-200603000-00007. PMID 16538076.
- ↑ Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL, et al. (October 2003). "Kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention". Circulation. 108 (17): 2154–69. doi:10.1161/01.CIR.0000095676.90936.80. PMID 14581387.
- ↑ Tonelli M, Wiebe N, Culleton B, House A, Rabbat C, Fok M, et al. (July 2006). "Chronic kidney disease and mortality risk: a systematic review". Journal of the American Society of Nephrology. 17 (7): 2034–47. doi:10.1681/ASN.2005101085. PMID 16738019. Archived from the original on 2008-06-09. Retrieved 2008-06-29.
- ↑ Heidenheim AP, Kooistra MP, Lindsay RM (2004). Quality of life. Contrib Nephrol. Contributions to Nephrology. Vol. 145. pp. 99–105. doi:10.1159/000081673. ISBN 978-3-8055-7808-0. PMID 15496796.
- ↑ de Francisco AL, Piñera C (January 2006). "Challenges and future of renal replacement therapy". Hemodialysis International. International Symposium on Home Hemodialysis. 10 Suppl 1 (Suppl 1): S19-23. doi:10.1111/j.1542-4758.2006.01185.x. PMID 16441862.
- ↑ Groothoff JW (July 2005). "Long-term outcomes of children with end-stage renal disease". Pediatric Nephrology. 20 (7): 849–53. doi:10.1007/s00467-005-1878-9. PMID 15834618.
- ↑ Giri M (2004). "Choice of renal replacement therapy in patients with diabetic end stage renal disease". EDTNA/ERCA Journal. 30 (3): 138–42. doi:10.1111/j.1755-6686.2004.tb00353.x. PMID 15715116.
- ↑ Pierratos A, McFarlane P, Chan CT (March 2005). "Quotidian dialysis--update 2005". Current Opinion in Nephrology and Hypertension. 14 (2): 119–24. doi:10.1097/00041552-200503000-00006. PMID 15687837. Archived from the original on 2020-08-27. Retrieved 2019-06-30.
- ↑ 69.0 69.1 Maisonneuve P, Agodoa L, Gellert R, Stewart JH, Buccianti G, Lowenfels AB, et al. (July 1999). "Cancer in patients on dialysis for end-stage renal disease: an international collaborative study". Lancet. 354 (9173): 93–9. doi:10.1016/S0140-6736(99)06154-1. PMID 10408483.
- ↑ American Society of Nephrology. "Five Things Physicians and Patients Should Question" (PDF). Choosing Wisely: An Initiative of the ABIM Foundation. Archived (PDF) from the original on April 16, 2012. Retrieved August 17, 2012.
- ↑ Chertow GM, Paltiel AD, Owen WF, Lazarus JM (June 1996). "Cost-effectiveness of cancer screening in end-stage renal disease". Archives of Internal Medicine. 156 (12): 1345–50. doi:10.1001/archinte.1996.00440110117016. PMID 8651845.
- ↑ Centers for Disease Control Prevention (CDC) (March 2007). "Prevalence of chronic kidney disease and associated risk factors--United States, 1999-2004". MMWR. Morbidity and Mortality Weekly Report. 56 (8): 161–5. PMID 17332726. Archived from the original on 2017-07-19. Retrieved 2017-09-09.
- ↑ Morgan T (21 January 2009). "Chronic Kidney Disease (stages 3–5) prevalence estimates using data from the Neoerica study (2007)". Association of Public Health Observatories. Archived from the original on 18 July 2011. Retrieved 4 March 2010.
- ↑ 74.0 74.1 74.2 Appel LJ, Wright JT, Greene T, Kusek JW, Lewis JB, Wang X, et al. (April 2008). "Long-term effects of renin-angiotensin system-blocking therapy and a low blood pressure goal on progression of hypertensive chronic kidney disease in African Americans". Archives of Internal Medicine. 168 (8): 832–9. doi:10.1001/archinte.168.8.832. PMC 3870204. PMID 18443258.[permanent dead link]
- ↑ "Tackling the £1.5bn a year cost of chronic kidney disease". Health Service Journal. 20 March 2020. Archived from the original on 28 September 2020. Retrieved 16 May 2020.
- ↑ Lena, Pelander (2018). Chronic kidney disease in the dog. ISBN 978-91-7760-208-8. Archived from the original on 12 June 2018. Retrieved 8 June 2018.
- ↑ Pelander L, Ljungvall I, Egenvall A, Syme H, Elliott J, Häggström J (June 2015). "Incidence of and mortality from kidney disease in over 600,000 insured Swedish dogs". The Veterinary Record. 176 (25): 656. doi:10.1136/vr.103059. PMID 25940343.
- ↑ "Olmesartan". clinicaltrials. Archived from the original on 2021-08-28.
- ↑ "Angiotesin Receptor". Archived from the original on 2020-01-27.
- ↑ Kim, Kun Hyung; Lee, Myeong Soo; Kim, Tae-Hun; Kang, Jung Won; Choi, Tae-Young; Lee, Jae Dong (2016-06-28). "Acupuncture and related interventions for symptoms of chronic kidney disease". The Cochrane Database of Systematic Reviews (6): CD009440. doi:10.1002/14651858.CD009440.pub2. ISSN 1469-493X. PMID 27349639.
External links[edit | edit source]
| Classification | |
|---|---|
| External resources |
- Dialysis Complications of Chronic Renal Failure at eMedicine
- Chronic Renal Failure Information Archived 2013-03-15 at the Wayback Machine from Great Ormond Street Hospital
![Chronic renal disease caused by glomerulonephritis with increased echogenicity and reduced cortical thickness. Measurement of kidney length on the US image is illustrated by '+' and a dashed line.[44]](data/media/images/200px-Ultrasonography_of_chronic_renal_disease_caused_by_glomerulonephritis.jpg)
![Nephrotic syndrome. Hyperechoic kidney without demarcation of cortex and medulla.[44]](data/media/images/200px-Ultrasonography_of_kidney_with_nephrotic_syndrome.jpg)
![Chronic pyelonephritis with reduced kidney size and focal cortical thinning. Measurement of kidney length on the US image is illustrated by '+' and a dashed line.[44]](data/media/images/200px-Ultrasonography_of_chronic_pyelonephritis_with_reduced_kidney_size_and_focal_cortical_thinning.jpg)
![End-stage chronic kidney disease with increased echogenicity, homogenous architecture without visible differentiation between parenchyma and renal sinus and reduced kidney size. Measurement of kidney length on the US image is illustrated by '+' and a dashed line.[44]](data/media/images/200px-Ultrasonography_of_end-stage_chronic_kidney_disease.jpg)