 | |
 | |
| Names | |
|---|---|
| Trade names | Zeposia |
| Other names | RPC-1063 |
| |
| Clinical data | |
| Drug class | sphingosine-1-phosphate|S1P blocker[1][2] |
| Main uses | Multiple sclerosis, ulcerative colitis[1][2] |
| Side effects | Upper respiratory infection, liver inflammation, low blood pressure with standing, urinary tract infection, back pain[2] |
| Pregnancy category |
|
| Routes of use | By mouth |
| Typical dose | 0.92 mg OD[2] |
| External links | |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a620029 |
| Legal | |
| License data | |
| Legal status | |
| Pharmacokinetics | |
| Elimination half-life | 19 hours |
| Chemical and physical data | |
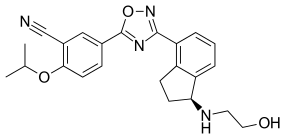
| Formula | C23H24N4O3 |
| Molar mass | 404.470 g·mol−1 |
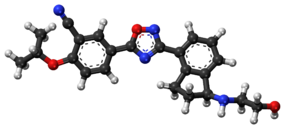
| 3D model (JSmol) | |
| |
| |
Ozanimod, sold under the brand name Zeposia, is a medication used to treat multiple sclerosis (MS) and ulcerative colitis (UC).[1][2] For MS this includes clinically isolated syndrome, relapsing-remitting, and active secondary progressive disease.[2] In UC it is used in those with moderate to severe disease.[2] It is taken by mouth.[2]
Common side effects include upper respiratory infection, liver inflammation, low blood pressure with standing, urinary tract infection, and back pain.[2] Other side effects may include heart arrhythmias, high blood pressure, and macular edema.[2] Use during or in the 3 months before pregnancy may harm the baby.[2] It is a sphingosine-1-phosphate (S1P) receptor agonist, which results in stopping lymphocytes from going to the brain and spinal cord.[1][2]
Ozanimod was approved for medical use in the United States, Europe, and Australia in 2020.[1][2][5] In the United Kingdom 4 weeks of medication costs the NHS about £1,400 as of 2021.[6] IN the United States this amount costs about 7,200 USD.[7]
Medical uses[edit | edit source]
In the United States, ozanimod is used to treat adults with relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease; and with moderately to severely active ulcerative colitis (UC).[4]
In the European Union and in Australia, ozanimod is indicated for the treatment of adults with relapsing remitting multiple sclerosis (RRMS).[5]
Dosage[edit | edit source]
It is typically taken at a dose of 0.92 mg per day.[2] It; however, is started at 0.23 mg per day for 4 days, than 0.46 mg per day for 3 days, followed by the typical dose.[1]
Pharmacology[edit | edit source]
Pharmacodynamics[edit | edit source]
Ozanimod is an agonist of the S1P1 and S1P5 receptors.[8] It demonstrates this effect in a dose-dependent manner, with 10-fold potency to three comparators.[8] This is an improvement of selectivity over its predecessor, fingolimod, which is non-specific to all 5 isotypes.[8] The agonism of S1P directly causes its internalization and degradation through the ubiquitin-proteosome pathway.[9] The loss of S1P leads to a decrease in the total lymphocyte count in circulation, specifically CD4+ CCR7+ and CD8+ CCR7+ T cells.[8][10]
Pharmacokinetics[edit | edit source]
Ozanimod has a high oral bioavailability, a circulating half-life of about 19 hours, and reaches highest blood plasma concentrations after about 6 hours.[8][10] Ozanimod is dehydrogenated by two CYP enzymes into two active metabolites, all with similar pharmacokinetics.[10] The decrease in lymphocyte count lasts for approximately 14 days after treatment discontinuation.[10] Unlike fingolimod, it does not require phosphorylation for activation, nor does it demonstrate cardiac abnormalities or hepatotoxicity.[8]
History[edit | edit source]
Ozanimod was discovered by The Scripps Research Institute and licensed to the biotech company Receptos Inc. which was acquired by Celgene Corp and then acquired by Bristol Myers Squibb.[11][12][13]
The US Food and Drug Administration (FDA) approved ozanimod based on evidence from two clinical trials (Trial 1/NCT02294058 and Trial 2/ NCT02047734) of 1767 subjects with relapsing forms of multiple sclerosis.[14] The trials were conducted at 173 centers in the United States, Belarus, Poland, Russia and Ukraine.[14] Subjects received ozanimod or comparator (interferon β1a, a product approved for the treatment of relapsing forms of multiple sclerosis) for up to one year (in Trial 1) or up to two years (in Trial 2).[14] Neither the subjects nor the health care providers knew which treatment was being given until the trials were completed.[14] The benefit of ozanimod was evaluated based on the percentage of subjects who experienced reduction in disease relapse in comparison to subjects treated with interferon β1a.[14]
In May 2021, the FDA approved ozanimod for an additional indcation for the treatment of moderately to severely active ulcerative colitis.[15]
Society and culture[edit | edit source]
Commercial[edit | edit source]
After going public in May 2013, Receptos, Inc. stock surged with the clinical data ozanimod displayed as a S1P immunomodulating drug.[16][17] In August 2015, Receptos was acquired by Celgene for $7.2 billion through a combination of cash in hand and new debt, leading to a 22% increase in their stock value.[12][18] Receptos, Inc. (Celgene) patented the synthesis of ozanimod in July 2016.[19] With the expansion of Celgene's inflammation and immunology profile, the company had been expecting to generate $4 to $6 billion in annual sales from ozanimod; however, the FDA rejected its application for the drug's approval in February 2018.[17][20][21] Celgene refiled in March 2019.[citation needed] As the new owner, Bristol Myers Squibb received FDA approval on March 26, 2020, for ozanimod (Zeposia) oral capsules to treat adults with relapsing forms of multiple sclerosis (MS), including relapsing-remitting MS (RRMS), active secondary progressive MS (SPMS), and clinically isolated syndrome (CIS).[22] Ozanimod was approved for medical use in the European Union in May 2020,[1] and in Australia in July 2020.[3]
Research[edit | edit source]
Ozanimod is in development for additional immune-inflammatory indications, including ulcerative colitis and Crohn's disease.[22][8][15]
Touchstone[edit | edit source]
Touchstone is a double-blind, placebo controlled phase II clinical for the treatment of ulcerative colitis.[23][24] 197 patients, ages 18–75, with moderate to severe UC (Mayo Score 6-10) were recruited and assigned either placebo, 0.5 mg or 1 mg of oral ozanimod followed by 1 week of dose escalation. The 1 mg dose showed a slight increase in rate of clinical remission of UC and total lymphocyte decrease as compared to the placebo, with the most common adverse effects being headaches and anemia.[23] The authors noted that limitations on this study included a brief duration and small sample size, meaning they could not assess safety nor efficacy.[23]
Radiance[edit | edit source]
Radiance is a double-blind, placebo controlled phase combined II/III clinical trial for the treatment of relapsing multiple sclerosis.[25][26] For the phase II trial, 258 patients, ages 18–55 with RMS (Mean Expanded Disability Status Scale of 2.9) were assigned either placebo, 0.5 mg or 1 mg of oral ozanimod followed by 1 week of dose escalation.[25] Ozanimod significantly reduced MRI lesion activity in participants with relapsing multiple sclerosis over a period of 24 weeks.[25] Both doses of ozanimod reached anticipated range of 60-70% decreased lymphocyte count, and were well tolerated, with a safety profile consistent with a previous phase 1 study in healthy volunteers.[25][27] The most common adverse effects as compared to the placebo were: nasopharyngitis, headache, and urinary-tract infections, with no serious infectious or cardiac adverse effects.[25] With these results, both doses of ozanimod were taken forward into the 2-year long phase III trial and is completed but unpublished as of November 2016.[25][26]
Sunbeam[edit | edit source]
Sunbeam is the second RMS phase III clinical trial to establish the dose with optimum safety-benefit relationship, with an estimated size of 1200 patients.[25][28]It began in November 2014, and has an estimated completion date of February 2017.[28][needs update]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 "Zeposia EPAR". European Medicines Agency. 26 March 2020. Archived from the original on 25 October 2020. Retrieved 17 August 2020.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 "DailyMed - ZEPOSIA- ozanimod hydrochloride capsule ZEPOSIA 7-DAY STARTER PACK- ozanimod hydrochloride kit ZEPOSIA STARTER KIT- ozanimod hydrochloride kit". dailymed.nlm.nih.gov. Archived from the original on 10 November 2021. Retrieved 10 November 2021.
- ↑ 3.0 3.1 3.2 "Zeposia Australian Prescription Medicine Decision Summary". Therapeutic Goods Administration (TGA). 27 July 2020. Archived from the original on 13 August 2020. Retrieved 16 August 2020.
- ↑ 4.0 4.1 "Zeposia (ozanimod) capsules, for oral use" (PDF). Celgene Corporation. 25 March 2020. Archived (PDF) from the original on 26 March 2020. Retrieved 26 March 2020.
- ↑ 5.0 5.1 Australian Public Assessment Report: Ozanimod hydrochloride (PDF) (Report). 25 November 2020. Archived (PDF) from the original on 4 June 2021. Retrieved 4 June 2021.
- ↑ BNF 81: March-September 2021. BMJ Group and the Pharmaceutical Press. 2021. p. 902. ISBN 978-0857114105.
- ↑ "Zeposia Prices, Coupons & Patient Assistance Programs". Drugs.com. Retrieved 10 November 2021.
- ↑ 8.0 8.1 8.2 8.3 8.4 8.5 8.6 Scott FL, Clemons B, Brooks J, Brahmachary E, Powell R, Dedman H, et al. (June 2016). "Ozanimod (RPC1063) is a potent sphingosine-1-phosphate receptor-1 (S1P1 ) and receptor-5 (S1P5 ) agonist with autoimmune disease-modifying activity". British Journal of Pharmacology. 173 (11): 1778–92. doi:10.1111/bph.13476. PMC 4867749. PMID 26990079.
- ↑ Jo E, Sanna MG, Gonzalez-Cabrera PJ, Thangada S, Tigyi G, Osborne DA, et al. (June 2005). "S1P1-selective in vivo-active agonists from high-throughput screening: off-the-shelf chemical probes of receptor interactions, signaling, and fate". Chemistry & Biology. 12 (6): 703–15. doi:10.1016/j.chembiol.2005.04.019. PMID 15975516.
- ↑ 10.0 10.1 10.2 10.3 Juif PE, Kraehenbuehl S, Dingemanse J (August 2016). "Clinical pharmacology, efficacy, and safety aspects of sphingosine-1-phosphate receptor modulators". Expert Opinion on Drug Metabolism & Toxicology. 12 (8): 879–95. doi:10.1080/17425255.2016.1196188. PMID 27249325. S2CID 21915268.
- ↑ "FDA approves ozanimod, a drug invented at Scripps Research, for treatment of multiple sclerosis". Scripps Research (Press release). Archived from the original on 2021-01-22. Retrieved 2020-12-05.
- ↑ 12.0 12.1 "Celgene to Acquire Receptos, Advancing Leadership in Immune-Inflammatory Diseases". Celgene Corporation (Press release). 14 July 2015. Archived from the original on 4 June 2021. Retrieved 4 June 2021.
- ↑ "Bristol-Myers Squibb Completes Acquisition of Celgene, Creating a Leading Biopharma Company". Bristol Myers Squibb (Press release). 12 April 2019. Archived from the original on 28 June 2020. Retrieved 4 June 2021.
- ↑ 14.0 14.1 14.2 14.3 14.4 "Drug Trials Snapshots: Zeposia". U.S. Food and Drug Administration (FDA). 25 March 2020. Archived from the original on 2 April 2020. Retrieved 1 April 2020.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ 15.0 15.1 "U.S. Food and Drug Administration Approves Bristol Myers Squibb's Zeposia (ozanimod), an Oral Treatment for Adults with Moderately to Severely Active Ulcerative Colitis". Bristol Myers Squibb (Press release). 27 May 2021. Archived from the original on 4 June 2021. Retrieved 4 June 2021.
- ↑ Pollack A (2015-07-14). "Celgene Agrees to $7.2 Billion Deal for Receptos". New York Times. Archived from the original on 2021-10-26. Retrieved 2021-06-04.
- ↑ 17.0 17.1 "Celgene 2015 Annual Report" (PDF). Archived from the original (PDF) on 2016-11-08. Retrieved 2021-06-04.
- ↑ "Celgene to Buy Receptos for $7.2 Billion". The Wall Street Journal. July 14, 2015. Archived from the original on April 10, 2021. Retrieved June 4, 2021.
- ↑ US 9388147, Yeager AR, Brahmachary E, Martinborough E, Scott FL, Timony GA, Brooks JL, Tamiya J, Huang L, Moorjani M, Boehm MF, Hanson MA, Peach R, "Selective sphingosine 1 phosphate receptor modulators and methods of chiral synthesis", published 22 October 2015, assigned to Receptos and Celgene International II Sarl
- ↑ "Celgene to Acquire Receptos for $7.2B". Genetic Engineering & Biotechnology News. 2015-07-14. Archived from the original on 2018-03-29. Retrieved 2021-06-04.
- ↑ "U.S. FDA rejects filing for Celgene MS drug, shares fall". Reuters. Archived from the original on 2018-03-29. Retrieved 2018-03-28.
- ↑ 22.0 22.1 "U.S. Food and Drug Administration Approves Bristol Myers Squibb's Zeposia (ozanimod), a New Oral Treatment for Relapsing Forms of Multiple Sclerosis". Bristol-Myers Squibb Company (Press release). 26 March 2020. Archived from the original on 1 October 2020. Retrieved 26 March 2020.
- ↑ 23.0 23.1 23.2 Sandborn WJ, Feagan BG, Wolf DC, D'Haens G, Vermeire S, Hanauer SB, et al. (May 2016). "Ozanimod Induction and Maintenance Treatment for Ulcerative Colitis". The New England Journal of Medicine. 374 (18): 1754–62. doi:10.1056/NEJMoa1513248. PMID 27144850.
- ↑ "Efficacy and Safety Study of Ozanimod in Ulcerative Colitis". ClinicalTrials.gov. 23 July 2012. Archived from the original on 4 June 2021. Retrieved 4 June 2021.
- ↑ 25.0 25.1 25.2 25.3 25.4 25.5 25.6 Cohen JA, Arnold DL, Comi G, Bar-Or A, Gujrathi S, Hartung JP, et al. (April 2016). "Safety and efficacy of the selective sphingosine 1-phosphate receptor modulator ozanimod in relapsing multiple sclerosis (RADIANCE): a randomised, placebo-controlled, phase 2 trial". The Lancet. Neurology. 15 (4): 373–81. doi:10.1016/s1474-4422(16)00018-1. PMID 26879276. S2CID 3236201.
- ↑ 26.0 26.1 Clinical trial number NCT01628393 for "Efficacy and Safety Study of RPC1063 in Relapsing Multiple Sclerosis Patients (Radiance Study)" at ClinicalTrials.gov
- ↑ Hartung J (2012). "Results of a Thorough QT/QTc (TQT) Study of Orally Administered RPC1063, a Novel, Selective S1P1 Receptor Agonist, in Healthy Adult Volunteers" (PDF). Archived (PDF) from the original on 2016-11-09.
- ↑ 28.0 28.1 "Study of Ozanimod (RPC1063) in Relapsing Multiple Sclerosis (MS)". ClinicalTrials.gov. 19 November 2014. Archived from the original on 4 June 2021. Retrieved 4 June 2021.
External links[edit | edit source]
| External sites: | |
|---|---|
| Identifiers: |
|
- "Ozanimod hydrochloride". Drug Information Portal. U.S. National Library of Medicine. Archived from the original on 2020-10-30. Retrieved 2021-06-04.